Abstract
Background
Plasmodium ovale malaria is usually considered a tropical infectious disease associated with low morbidity and mortality. However, severe disease and death have previously been reported.
Case presentation
A case of severe P. ovale malaria in a healthy Caucasian man with a triangle splenic infarction and clinical progression towards Acute Respiratory Distress Syndrome was reported despite a rapid response to oral chloroquine treatment with 24-h parasitaemia clearance.
Conclusion
Plasmodium ovale malaria is generally considered as a benign disease, with low parasitaemia. However, severe disease and death have occasionally been reported. It is important to be aware that occasionally it can progress to serious illness and death even in immunocompetent individuals.
Similar content being viewed by others
Background
Plasmodium ovale malaria is usually considered a tropical infectious disease associated with low morbidity and mortality. However, severe disease and death have previously been reported [1]. A case of severe P. ovale malaria with a triangle splenic infarction and progression towards acute respiratory distress syndrome (ARDS) was reported in a healthy Caucasian man despite a rapid response to oral chloroquine treatment with 24-h parasitaemia clearance.
Case presentation
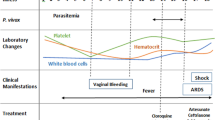
A case of a 4-year-old Caucasian man admitted in the Lazzaro Spallanzani National Institute for Infectious Diseases in Rome, Italy, due to “fever in returning travellers” was reported. At admission, the patient, a healthy man with benign prostatic hyperplasia only, in his medical history, was in good condition. He reported one week of asthenia, headache, night sweats, loss of appetite and, the day before, high fever with syncope. The patient reported travel to South Korea and, two weeks earlier, to Guinea Conakry without taking any anti-malarial chemoprophylaxis. On admission, blood tests showed thrombocytopenia (platelet count 50.000/mmc), C-reactive protein (CRP) 10.6 mg/dl, procalcitonin (PCT) 1.05 ng/ml, aspartate aminotransferase 103 U/L, alanine aminotransferase 67 U/L, gamma-glutamyl transferase 173U/L, with normal renal function and coagulation. Pan-malarial rapid test was positive for non-falciparum malaria and Plasmodium vivax rapid test was negative, thick and thin blood smear were positive and showed the presence of P. ovale trophozoites, with a 0.001% parasitaemia (40 parasites/µl). Oral chloroquine, 10 mg/kg as initial dose followed by 10 mg/kg on the second day and 5 mg/kg on the third day, was prescribed. In-house nested-polymerase chain reaction (PCR) confirmed the diagnosis of P. ovale excluding mixed infections [2]. Plasmodium ovale wallikeri was identified by using a nested PCR followed by 2% agarose gel electrophoresis (a 245 bp band confirmed P. o. wallikeri) and verified with amplicon sequencing [3]. Blood PCR for Leishmania and Dengue were negative; serology for Leishmania, Schistosoma, Strongyloides, Dengue, Chikungunya, HCV, HBV, HIV, HEV, Widal-Wright reaction for Salmonella and blood cultures were negative. Multiplex Real-Time PCR (Norovirus GII, Rotavirus A, Astrovirus, Norovirus G I, Cryptosporidium spp, Entamoeba histolytica, Giardia lamblia, Cyclospora cayetanensis, Vibrio parahaemolyticus, Clostridium difficile toxin A/B, Vibrio vulnificus, Enteropathogenic Escherichia coli, Campylobacter spp., Yersinia enterocolitica, Enterotoxigenic E. coli (It/st), Enteroinvasive E. coli/Shigella. STEC (stx1/stx2), Enteroaggregative E. coli, Salmonella spp., Plesiomonas shigelloides, Sapovirus. Vibrio cholerae STEC-0157:H7, Adenovirus F40/F41) on stool was negative. Posterior-anterior chest X-ray showed bilateral and diffused peribronchovascular thickening (Fig. 1) and abdominal ultrasound confirmed mild splenomegaly (bipolar diameter 15.5 cm) with homogeneous structure. The day after admission, despite a negative thick smear, the patient’s condition suddenly worsened: he developed dyspnea with a increased respiratory rate of 40 breaths per minute, low peripheral oxygen saturation less than 90%, and acute hypoxaemia confirmed by blood gas analysis. Chest auscultation revealed bilateral crackles in both respiratory phases. The patient started oxygen supplementation with 40% fractional inspired oxygen (FiO2) Venturi mask with improvement of blood gas analysis: PH: 7.47, pCO2: 31, PO2: 104 mmHg with an arterial oxygen tension (PaO2/FiO2 ratio) of 260. Therefore, antibacterial therapy with intravenous ceftriaxone 2 g daily was started. A multiplex Real-Time RT-PCR on sputum was positive for Staphylococcus aureus; sputum cultures, quantiferon TB Gold, nasopharynx swab for SARS-CoV-2 and pneumococcal/legionella urine antigen test were negative. After 24 h arterial blood gas analysis showed a reduced oxygen tension (pO2 72, pCo2 29, PaO2/FiO2 ratio of 180), Continuous positive airway pressure (CPAP) by using 40%FiO2 Boussignac mask and 5 mmhg positive end-expiratory pressure (PEEP) was started. A chest and abdomen computed tomography scan with intravenous contrast showed interstitial ground glass opacities involving all right and left lobes with early parenchymal lung consolidation, bilateral pleural and pericardium effusion (Fig. 2) and in the abdomen there was hypodense area with triangular morphology at splenic site (Fig. 3). The findings of the CT scan lay for cardiogenic oedema and triangle splenic infarction. The patient had no abdominal pain. Patient fluid balance was initially positive. Intravenous furosemide (20 mg every 12 h) and piperacillin/tazobactam (4.5 g every 8 h), oral doxycycline (100 mg every 12 h), enoxaparin 40 mg subcutaneous daily were started. In the following days, the patient gradually improved with decreasing the needs of oxygen until the definitive ending on day 15 since admission. Oral primaquine (30 mg daily for 14 days) was given after confirming a normal level of glucose-6-phosphate dehydrogenase activity in erythrocytes. The patient was discharged in good clinical condition after 18 days of hospitalization, with normal blood tests. Two weeks later at follow-up visit, blood tests were repeated with unremarkable results and no evidences of sequelae or relapse were reported.
Discussion and conclusion
A severe P. ovale malaria with a triangle splenic infarction and clinical progression towards ARDS was described despite a rapid response to chloroquine with fast parasitaemia clearance. Suddenly, with no underlying risk factors for severe disease, patient’s condition worsened with acute respiratory failure with CPAP-oxygen supplementation. Severe malaria is usually associated with Plasmodium falciparum infection. Plasmodium vivax and Plasmodium knowlesi are recognized as possible causes of severe disease. In contrast, P. ovale malaria is generally considered a benign disease, with low parasitaemia [4]. Two sympatric species of P. ovale occur globally: P. ovale curtisi (classic type) and P. ovale wallikeri (variant type) [5]. Rare case reports of complicated P. ovale malaria are reported and only in few of them P. ovale sub-species have been identified. ARDS is the prevalent severe condition described [6, 7]; anecdotal cases of splenic rupture [8] and a single case of splenic infarction are described previously [9]. A recent case report describes a haemophagocytic lymphohistiocytosis secondary to P. ovale wallikeri infection [10]. The 2023 WHO Guidelines for uncomplicated P. ovale malaria recommend either an artemisinin-based combination therapy (ACT) or chloroquine, in areas with chloroquine-susceptible infections. In areas with chloroquine-resistant infections, adults and children with uncomplicated P. ovale malaria should be treated with ACT [11]. Chloroquine is the only option recommended by CDC [12]. The pathogenesis of P. ovale severe infection has not been well established. It is well known that ARDS in P. falciparum malaria is caused by increased pro-inflammatory process with unbalanced endothelial permeability; intravenous over hydration, sequestration of red cells, and disseminated intravascular coagulation are all other likely determinants of severe ARDS [13]. In this case, the patient presented a positive fluid balance, thrombocytopenia and both increased CRP and PCT [14]. Chloroquine-resistance was excluded because of the early negative thick smear. Although chloroquine is known to have an anti-inflammatory modulation, inhibiting the production of cytokines such as TNF, IL-1β and IL-6 [15], in this case it did not seem to prevent the cascade of the inflammatory phenomenon leading to respiratory distress. Regarding splenic infarction, this is the second case described in the literature due to P. ovale malaria [16], likely to be part of a Plasmodium-driven coagulation and proinflammatory disbalance leading to an increased adhesion of malaria-infected red blood cells (iRBCs) to endothelial cells, with rosetting of iRBCs and non-iRBCs, and to splenic cell hyperplasia [9, 17]. Splenic infarction has rarely been reported as a complication of P. falciparum or P. vivax malaria. This event is likely to be underdiagnosed and underreported. Indeed, patients with splenic infarction can be asymptomatic or present only mild symptoms and, in resource-limited settings, abdomen ultrasound or computer tomography imaging could be not available [9].
In conclusion, more studies are needed to better define the pathogenesis of severe malaria due to P. ovale and the clinical implication with its wallikeri or curtisi sub-species. Plasmodium o. wallikeri may be more frequent in males and Caucasians. Moreover, P. o. wallikeri could have greater pathogenicity with a deeper thrombocytopenia, a higher INR and shorter latency than P. o. curtisi [18]. Severe cases can be seen in both species but in a French cohort, although the difference was not statistically significant, P. o. wallikeri–infected patients were 5 times more frequently hospitalized in intensive care or intermediate care than P. o. curtisi–infected patients [19]. Furthermore, severe cases of P. ovale malaria could be under-reported due to misclassification by rapid diagnostic tests poor sensitivity for P. ovale species [20], to diagnostic difficulties in the detection of a low parasitaemia and in the differential species detection between P. ovale and P. vivax, when PCR is not available. Finally, host–pathogen risk factor, genetic determinants, comorbidities and predictive markers of clinical progression to severe malaria and acute respiratory distress in P. ovale are unclear.
Availability of data and materials
Not applicable.
Abbreviations
- CRP:
-
C-reactive protein
- PCT:
-
Procalcitonin
- PCR:
-
Polymerase chain reaction
- FiO2:
-
Fractional inspired oxygen
- PaO2:
-
Arterial oxygen tension
- CPAP:
-
Continuous positive airway pressure
- PEEP:
-
Positive end-expiratory pressure
- ARDS:
-
Acute respiratory distress syndrome
- WHO:
-
World Health Organization
- ACT:
-
Artemisinin-based combination therapy
- CDC:
-
Centers for disease control and prevention
- iRBCs:
-
Malaria-infected red blood cells
References
Groger M, Fischer HS, Veletzky L, Lalremruata A, Ramharter M. A systematic review of the clinical presentation, treatment and relapse characteristics of human Plasmodium ovale malaria. Malar J. 2017;16:112.
Snounou G, Viriyakosol S, Zhu XP, Jarra W, Pinheiro L, do Rosario VE, et al. High sensitivity of detection of human malaria parasites by the use of nested polymerase chain reaction. Mol Biochem Parasitol. 1993;61:315–20.
Oguike MC, Betson M, Burke M, Nolder D, Stothard JR, Kleinschmidt I, et al. Plasmodium ovale curtisi and Plasmodium ovale wallikeri circulate simultaneously in African communities. Int J Parasitol. 2011;41:677–83.
Collins WE, Jeffery GM. Plasmodium ovale: parasite and disease. Clin Microbiol Rev. 2005;18:570–81.
Sutherland CJ, Tanomsing N, Nolder D, Oguike M, Jennison C, Pukrittayakamee S, et al. Two nonrecombining sympatric forms of the human malaria parasite Plasmodium ovale occur globally. J Infect Dis. 2010;201:1544–50.
D’Abramo A, Gebremeskel Tekle S, Iannetta M, Scorzolini L, Oliva A, Paglia MG, et al. Severe Plasmodium ovale malaria complicated by acute respiratory distress syndrome in a young Caucasian man. Malar J. 2018;17:139.
Lau YL, Lee WC, Tan LH, Kamarulzaman A, Syed Omar SF, Fong MY, et al. Acute respiratory distress syndrome and acute renal failure from Plasmodium ovale infection with fatal outcome. Malar J. 2013;12:389.
Facer CA, Rouse D. Spontaneous splenic rupture due to Plasmodium ovale malaria. Lancet. 1991;338:896.
Hwang JH, Lee CS. Malaria-induced splenic infarction. Am J Trop Med Hyg. 2014;91:1094–100.
Novella-Mena M, Cantudo-Muñoz P, Tallón-Pérez JD, Gómez-Rodríguez MDM, Rojo-Marcos G. Hemophagocytic lymphohistiocytosis secondary to Plasmodium ovale wallikeri infection. Am J Trop Med Hyg. 2023;109:608–10.
WHO. Guidelines for malaria. Geneva: World Health Organization; 2023. p. 2023.
CDC Treatment of Malaria: Guidelines for Clinicians. Last Reviewed: June 28. 2023
Taylor WRJ, Hanson J, Turner GDH, White NJ, Dondorp AM. Respiratory manifestations of malaria. Chest. 2012;142:492–505.
Mahittikorn A, Kotepui KU, Mala W, Wilairatana P, Kotepui M. Procalcitonin as a candidate biomarker for malarial infection and severe malaria: a meta-analysis. Int J Environ Res Public Health. 2022;19:11389.
Jang CH, Choi JH, Byun MS, Jue DM. Chloroquine inhibits production of TNF-alpha, IL-1beta and IL-6 from lipopolysaccharide-stimulated human monocytes/macrophages by different modes. Rheumatology. 2006;45:703–10.
Cinquetti G, Banal F, Rondel C, Plancade D, de Saint RC, Adriamanantena D, et al. Splenic infarction during Plasmodium ovale acute malaria: first case reported. Malar J. 2010;9:288.
Bush MA, Anstey NM, Yeo TW, Florence SM, Granger DL, Mwaikambo ED, et al. Vascular dysfunction in malaria: understanding the role of the endothelial glycocalyx. Front Cell Dev Biol. 2021;9:751251.
Rojo-Marcos G, Rubio-Muñoz JM, Angheben A, Jaureguiberry S, García-Bujalance S, Tomasoni LR, et al. Prospective comparative multi-centre study on imported Plasmodium ovale wallikeri and Plasmodium ovale curtisi infections. Malar J. 2018;17:399.
Joste V, Bailly J, Hubert V, Pauc C, Gendrot M, Guillochon E, et al. Plasmodium ovale wallikeri and P. ovale curtisi infections and diagnostic approaches to imported malaria France. Emerg Infect Dis. 2021;27:372–84.
Bigaillon C, Fontan E, Cavallo JD, Hernandez E, Spiegel A. Ineffectiveness of the Binax NOW malaria test for diagnosis of Plasmodium ovale malaria. J Clin Microbiol. 2005;43:1011.
Funding
This work was supported by Line1 Ricerca Corrente “Studio dei patogeni ad alto impatto sociale: emergent, da importazione, multiresistenti, negletti” funded by Italian Ministry of Health.
Author information
Authors and Affiliations
Contributions
Maria Virginia Tomassi: performed the clinical assessments, treated the patient and drafted the manuscript Alessandra D’Abramo: performed the clinical assessments, treated the patient and drafted the manuscript, Writing-review and editing. Validation Serena Vita: performed the clinical assessments, treated the patient and drafted the manuscript, writing-review and editing. Validation. Angela Corpolongo: performed the clinical assessments, treated the patient and drafted the manuscript, Francesca Faraglia: performed the clinical assessments and treated the patient. Tommaso Ascoli Bartoli: performed the clinical assessments and treated the patient. Antonella Vulcano: performed molecular diagnostic test, Barbara Bartolini: performed molecular diagnostic test Emanuele Nicastri: Supervision, Funding acquisition, Writing-review and editing. Validation. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional Review Board approval is not required by the Ethical Committee of the authors’ institution for the presentation of a single case report.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tomassi, M.V., D’Abramo, A., Vita, S. et al. A case of severe Plasmodium ovale malaria with acute respiratory distress syndrome and splenic infarction in a male traveller presenting in Italy. Malar J 23, 93 (2024). https://doi.org/10.1186/s12936-024-04911-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-024-04911-4