Abstract
Background
To mitigate hospital-acquired transmission of coronavirus disease 2019 (COVID-19), various prevention and control measures have been strictly implemented in medical institutions. These stringent measures can potentially reduce the incidence of hospital-acquired respiratory infections. This study aimed to assess if there were changes in the prevalence of hospital-acquired respiratory infections during a period of national attention focused on COVID-19 prevention.
Methods
A retrospective analysis of the clinical data from adult patients with hospital-acquired respiratory infections admitted between October and December 2019 and during the same period in 2020 was performed. All patients were referred from a general hospital in Beijing China and COVID-19 patients were not treated at the hospital. Hospital-acquired respiratory infections were diagnosed based on the criteria of the Centers for Disease Control and Prevention/National Healthcare Safety Network (CDC/NHSN). A comparison of the incidence and mortality rate of hospital-acquired respiratory infections between the two selected time periods was conducted. Additionally, multivariate logistics regression analysis was used to identify mortality-associated risk factors.
Results
This study included 2,211 patients from October to December 2019 (pre-COVID-19 pandemic) and 2,921 patients from October to December 2020 (during the COVID-19 pandemic). The incidence of hospital-acquired respiratory infections in 2019 and 2020 was 4.7% and 2.9%, respectively, with odds ratio (OR): 0.61, 95% confidence interval (CI): 0.46–0.81, and P = 0.001. In-hospital mortality of hospital-acquired respiratory infections in 2019 and 2020 was 30.5% and 38.4%, respectively, with OR: 1.42, 95%CI: 0.78–2.59, and P = 0.25. Multivariate logistics regression analysis revealed that a history of previous malignancy (OR: 2.50, 95%CI: 1.16–5.35, P = 0.02), was associated with in-hospital mortality.
Conclusions
The incidence of hospital-acquired respiratory infections was significantly decreased following the implementation of various prevention and control measures during the COVID-19 pandemic. A history of previous malignancy was associated with higher in-hospital mortality in older inpatients with hospital-acquired respiratory infections.
Similar content being viewed by others
Introduction
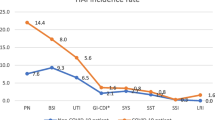
Healthcare-associated infections (HAIs) have emerged as the most prevalent adverse events in medical institutions, affecting approximately 5-15% of inpatients [1]. In mainland China, the prevalence of HAIs is estimated to be around 3.12% [2]. These infections can lead to several detrimental consequences, such as prolonged hospital stays, increased rates of bacterial drug resistance, escalated medical expenses, and higher mortality rates, thereby imposing a substantial socioeconomic burden. Studies have demonstrated that patients with HAIs experience significantly extended hospital stays, with an average duration of 25.05 days, contrary to 7.10 days for those without HAIs [3]. Among HAIs, respiratory infections are the most common, accounting for 14.9% of cases, with hospital-acquired pneumonia (HAP) and lower respiratory tract infections accounting for 14.9% and 4.1% of cases, respectively [4]. Interestingly, a study conducted in the United States revealed that pneumonia accounted for 26% of HAIs in 2018 [5]. Meanwhile, a Chinese study demonstrated that 43.8% of HAIs were respiratory infections, followed by blood infections (15.74%), urinary system infections (12.69%), surgical site infections (8.58%), and gastrointestinal infections (7.43%) [6].
The coronavirus disease 2019 (COVID-19) has rapidly spread worldwide since January 2020. To combat this, the Chinese government has implemented robust prevention and control measures, including mandatory mask-wearing in public places, promoting hand hygiene, improving room ventilation, discouraging crowded spaces, and canceling large gatherings. Moreover, specific preventive measures have been strictly enforced within medical institutions to prevent the transmission of COVID-19, such as patients who tested positive for COVID-19 were treated in specialized infectious disease hospitals, minimizing unnecessary hospital visits, restricting and designating caregivers, ensuring at least 1-m spacing between hospital beds, closely monitoring adherence to hand hygiene protocols, and mandating the use of N95 masks and protective equipment. Additionally, these measures may also have implications for hospital-acquired respiratory infections. To date, relatively few studies have explored the impact of COVID-19 prevention and control measures on the incidence of HAIs, and the results have been inconsistent [7, 8]. We conducted this study to assess any potential changes in the prevalence of hospital-acquired respiratory infections during the COVID-19 pandemic.
Methods
Study design and settings
A retrospective observational study was conducted at a tertiary teaching hospital in Beijing, China. This study included adult inpatients diagnosed with hospital-acquired respiratory infections who were hospitalized during two periods: October to December 2019 (pre-COVID-19 pandemic) and October to December 2020 (during the COVID-19 pandemic). Patients with COVID-19 were not treated at the hospital as they were admitted to designated medical institutions, according to the prevention and control policy of China for COVID-19 at that time. The exclusion criteria were as follows: (1) patients < 18 years old; (2) patients undergoing immunosuppressive treatment or chemotherapy during the last three months. In the case of multiple episodes of hospital-acquired respiratory infections, only the first episode was considered for inclusion in the study.
We retrieved data from the electronic medical records. The extracted information included gender, age, admission to hospital pre- or during the COVID-19 pandemic, length of hospital stay, underlying diseases, laboratory parameters, diagnosis and outcomes, as presented in Table 1. In this study, the exposure variable was whether admitted during the COVID-19 pandemic (October to December 2020). The primary outcome was the incidence of hospital-acquired respiratory infections pre- and during the COVID-19 pandemic. Moreover, we analyzed the in-hospital mortality rate and risk factors for mortality of hospital-acquired respiratory infections.
Screening criteria
Patients discharged with a diagnosis of pneumonia, bronchitis, or respiratory infections were screened out using the international classification of disease (ICD) codes on the first page of medical records (ICD codes refer to Supplementary Appendix 1). We reviewed the medical records of these patients and determined whether they had a hospital-acquired respiratory infection following the Centers for Disease Control and Prevention/National Healthcare Safety Network (CDC/NHSN) surveillance definition of healthcare-associated Infections [9] (refer to Supplementary Appendix 2).
To ensure accuracy and reliability, two attending specialists further validated the diagnosis based on the CDC/NHSN diagnostic criteria.
Definitions and diagnostic criteria
CDC/NHSN defined hospital-acquired infections as a localized or systemic condition resulting from an adverse reaction to the presence of an infectious agent(s) or its toxin(s). The infection must not be present or in the incubation period at the time of admission.
Upper respiratory infections include upper respiratory tract, pharyngitis, laryngitis, and epiglottitis. Lower respiratory infections were defined as bronchitis, tracheobronchitis, bronchiolitis, and tracheitis, without evidence of pneumonia.
CDC/NHSN considered patients as HAP if two or more serial chest radiographs demonstrated at least one of the following: (1) New or progressive and persistent infiltrated; (2) Consolidation; (3) Cavitation. For any patients, at least one of the following: (1) Fever with no other recognized cause; (2) Leukopenia (< 4,000 white blood cells (WBC)/mm3) or leukocytosis ( ≧ 12,000 WBC/mm3); (3) For adults ≧ 70 years old, altered mental status with no other recognized cause. And at least 2 of the following: (1) New onset of purulent sputum or change in character of sputum or increased respiratory secretions or increased suctioning requirements; (2) New onset or worsening cough, or dyspnea, or tachypnea; (3) Rales or bronchial breath sounds; (4) Worsening gas exchange.
Hospital-acquired respiratory infections were defined as infections that occurred 48 h or more after hospital admission in accordance with the CDC/NHSN guidelines.
Severe pneumonia was diagnosed according to the IDSA/ATS 2007 [10]. Validated definition included either one major criterion or three or more minor criteria. Major criteria included the following: septic shock with the need for vasopressors; respiratory failure requiring mechanical ventilation. Minor criteria included the following: (1) respiratory rate ≧ 30 breaths/min; (2) PaO2/FiO2 ratio ≦ 250; (3) Multilobar infiltrates; (4) Confusion/disorientation; (5) Uremia (blood urea nitrogen level ≧ 20 mg/dl ); (6) Leukopenia (WBC count < 4,000 cells/ul ); (7) Thrombocytopenia ( platelet count < 100,000/ul); (8) Hypothermia ( core temperature < 36℃); (9) Hypotention requiring aggressive fluid resuscitation.
Cardiovascular events were define as defined as one or more of the following [11]: (1) blood levels of cardiac biomarkers (TNI or CKMB) above the 99th percentile upper reference limit; (2) new abnormalities in electrocardiography, including supraventricular tachycardia, ventricular tachycardia, atrial fibrillation, ventricular fibrillation, bundle branch block, ST-segment elevation/depression, T-wave flattening/inversion, and QT interval prolongation; (3) new abnormalities in echocardiography, including decreased EF value (EF < 50%), regional/global ventricular wall motion abnormalities, the presence of pericardial effusion, and pulmonary arterial hypertension (PAH).
Statistical methods
All normally distributed continuous data are presented as mean ± standard deviation. Non-normally distributed continuous data are presented as medians and interquartiles. The unpaired student t-test was used to analyze normally distributed continuous data, whereas the Mann– Whitney U-test was used to compare non-normally distributed data. Categorical variables are expressed as numbers and percentages. Differences between groups were assessed using the chi-squared test. The incidence of hospital-acquired respiratory infection was determined by dividing the number of cases by the total number of hospitalized patients during the same period (incidence of hospital-acquired respiratory infection = number of cases/total number of hospitalized patients × 100%). Binary logistics regression analysis (enter) was performed to explore risk factors for mortality of hospital-acquired respiratory infections. In logistics regression analysis, we included variables with statistical significance (P < 0.05) in the univariate analysis and those with clinical importance, such as whether they were admitted during the COVID-19 pandemic. In univariate analysis, severe pneumonia was a significant variable; however, it was arguably on the causal pathway from pneumonia to death. As such we did not add this variable to the logistic regression models. Hypothesis testing of the multivariate model was performed using the log-likelihood ratio test, and the Hosmerr–Lemeshow test was used to assess the goodness of fit of the statistical model. For those variables with less than 25% missing data, median/mode interpolation was performed. For continuous quantitative data, we used median interpolation. Mode interpolation was used for discrete quantitative data. All statistical analyses were performed using the SPSS program Statistical Package for the Social Sciences program (version 26.0, SPSS Inc., Chicago, IL, United States). Two-tailed P < 0.05 was considered significant.
Results
Patients
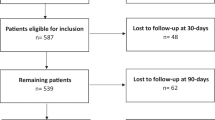
A total of 5569 patients from October to December 2019 and 3632 patients from October to December 2020 were admitted to our hospital. Patients who were readmitted within 48 h were considered as one admission. Furthermore, patients who underwent chemotherapy or immunosuppression therapy within the last three months were excluded from the study. Consequently, 2,211 patients from 2019 to 2,921 patients from 2020 were included in the study, forming the cohort for analysis. (refer to Fig. 1).
Among the 2019 cohort, 359 out of 2,211 patients (16.2%) met the criterion for screening for hospital-acquired respiratory infections. In the 2020 cohort, a lower proportion of 261 out of 2,921 patients (8.9%) met the criteria for screening for hospital-acquired respiratory infections; however, the difference was statistically non-significant (P = 0.13).
Prevalence of hospital-acquired respiratory infections
Ultimately, 105 out of 2,211 patients (4.7%) patients were diagnosed with hospital-acquired respiratory infections in 2019 (pre-COVID-19 pandemic), whereas in 2020 (during the COVID-19 pandemic), 86 out of 2921 (2.9%) received the same diagnosis. The incidence of hospital-acquired respiratory infections was 1.61 times higher in 2019 than that in 2020 (OR: 0.61, 95% CI: 0.46–0.81, P = 0.001; Table 2). The median age of patients in 2019 was 86 years, and 38.1% patients were males. In 2020, the median age was 85 years, and males accounted for the larger proportion (59.3%); however, there was no significant difference between the 2019 and 2020 periods (P > 0.05). There was no difference in terms of comorbidities (except for chronic kidney disease, CKD), nasal feeding, gastrointestinal hemorrhage, cardiovascular events, severe pneumonia, cases with sputum culture, and length of stay in hospital (P > 0.05; Table 1). More patients in 2019 had CKD and used antibiotics during the last three months. Additionally, fewer patients were bedridden in 2019. In 2019, fewer patients had experienced at least one type of cardiovascular event; however, there was no significant difference compared to patients in 2020 (81.9% versus 83.7%, P >0.05). Sputum culture testing was performed in 77.1% of patients in 2019 and 80.2% of patients in 2020 (P > 0.05). Among those tested, 45 (55.6%) cases experienced positive cultures in 2019, and 31 (44.9%) cases exhibited positive cultures in 2020, without significant differences (P = 0.19). More samples in 2019 experienced positive sputum cultures than in 2020 (48.52% versus 31.74%, P < 0.05). The most common bacteria identified were Pseudomonas aeruginosa, Klebsiella pneumoniae, Staphylococcus aureus, and Acinetobacter baumannii.
Risk factors for in-hospital mortality in patients with hospital-acquired respiratory infections
In 2019 and 2020, 65 patients with hospital-acquired respiratory infections passed away during their hospital stay, while 126 patients survived. The mortality rate during hospitalization was 30.5% in 2019 and 38.4% in 2020; however, there was no significant difference, (OR: 1.42, 95%CI: 0.78–2.59, P = 0.25; Table 3). Upon analyzing the characteristics of these groups, several notable differences emerged. In the mortality group, patients were older than those in the survival group (86 years versus 85 years, OR: 1.03, 95%CI: 1.00-1.05, P = 0.04). In the mortality group, a higher proportion of patients exhibited a history of malignant tumors (29.2% versus 15.9%, OR: 2.19, 95%CI: 1.07–4.48, P = 0.03) and cardiovascular diseases (69.2% versus 50.8%, OR: 2.18, 95%CI: 1.16–4.10, P = 0.02) compared to the survival group. Furthermore, a significant number of patients in the mortality group were diagnosed with severe pneumonia (63.1% versus 7.1%, OR: 22.21, 95%CI: 9.55–51.68, P = 0.00). Conversely, in the mortality group, fewer patients used antibiotics during the three months before admission (33.8% versus 54.8%, OR: 0.42, 95%CI: 0.23–0.79, P = 0.01), and these patients experienced a short hospital stay (25 days versus 45 days, OR: 0.97, 95%CI: 0.96–0.99, P = 0.00). In the mortality group, there was a higher incidence of gastrointestinal hemorrhage (23.1% versus 12.7%, OR: 2.06, 95%CI: 0.95–4.50, P = 0.07) and longer antibiotic usage (20 versus 18 days, OR: 0.99, 95% CI: 0.98–1.01, P = 0.57), although these differences were statistically non-significant. No significant differences were observed in gender, long-term bedridden status, or positive sputum culture between the two groups (Table 4). In the mortality group, 28 patients (43.1%) demonstrated positive sputum cultures. The most common pathogens identified were Pseudomonas aeruginosa, Klebsiella pneumoniae, Staphylococcus aureus, and Acinetobacter baumannii. Likewise, these pathogens were also prevalent in the survival group.
To identify independent factors associated with in-hospital mortality of hospital-acquired respiratory infections pre- and during the COVID-19 pandemic, a multivariate logistic regression analysis (enter) was conducted (Hosmer and Lemeshow test, P = 0.188; Table 5). The results revealed that a history of previous malignancy ( OR: 2.50, 95%CI: 1.16–5.35, P = 0.02) was an independent factor for in-hospital mortality. Age, cardiovascular disease and admission during the COVID-19 pandemic exhibited a higher risk of mortality; however, the differences were statistically non-significant.
Discussion
In this retrospective study, we compared the prevalence of hospital-acquired respiratory infections before and during the COVID-19 pandemic period. Notably, the incidence of hospital-acquired respiratory infections decreased from 4.2 to 2.9% (P = 0.001), possibly due to the implementation of various prevention and control measures, including reducing unnecessary hospital visits, limiting and designating caregivers, increasing hospital bed spacing to at least 1 m, closely monitoring compliance with hand hygiene protocols, and mandating the use of N95 masks.
The incidence of hospital-acquired respiratory infections observed in our study fell within the reported range of 1–4.7% from other countries [12,13,14]. Moreover, a 3-year surveillance study in China also revealed that the incidence of lower respiratory infections increased significantly with age, with rates of 0.85% and 2.05% in patients aged 60–69 years and ≥ 80 years, respectively [15]. Interestingly, the rate of patients ≥ 80 years in the surveillance study was consistent with our study, where the median age of patients was 85. However, the rate of hospital-acquired respiratory infections in our study was lower than in a multicenter study in China, where the incidence of hospital-acquired pneumonia (HAP) was 11.36% in patients ≥ 80 years old [16]. This may be owing to factors such as the higher incidence of intensive care unit (ICU) admission (47.88%), patients with impaired consciousness (49.29%), patients undergoing surgery under general anesthesia (24.56%), glucocorticosteroid use (31.27%) and use of ventilators (19.08%) in that study.
Respiratory tract infections remain one of the most common infection sites, leading to increased morbidity, mortality, and higher hospital costs. Despite adopting prevention measures, studies have revealed that hospital-acquired infections generally have decreased; however, the prevalence of hospital-acquired pneumonia has remained more or less the same [5]. Similarly, an analysis of data from the Medicare Patient Safety Monitoring System between 2005 and 2013 demonstrated that the percentage of patients with ventilator-associated pneumonia remained constant, at approximately 10% [17]. A randomized, parallel-group, controlled trial investigating the effectiveness of a multi-component intervention (involving reverse Trendelenburg position, dysphagia screening, oral care, and vaccinations) revealed that the incidence of hospital-acquired pneumonia among patients treated with this intervention was comparable to that of patients receiving standard of care [14].
The main prevention measures mentioned in the literature included hand hygiene, oral care, decolonization, decreased aspiration risk, droplet isolation, protective isolation, and contact precautions [18,19,20,21,22,23,24]. However, there are limited studies on hospital-acquired infection prevention concerning expanded bed space, reduced visiting and fixed caregivers. A simulation study highlighted the significance of social distancing and personal protective equipment (PPE) usage in reducing the transmission rate of SARS-CoV-2 in a laboratory setting, with the N95 mask proving to be the most effective protective measure [25]. A population-based retrospective cohort study over three years revealed that the risk of hospital-acquired pneumonia was approximately three times higher in patients who stayed in rooms with more than four beds than those in rooms with three or fewer beds [26]. Additionally, a meta-analysis demonstrated that using single-patient rooms instead of multiple-patient rooms reduced the hospital-associated colonization of multidrug-resistant (MDR) pathogens and bacteremia rates [27]. During the COVID-19 pandemic, our hospital implemented various measures to combat the pandemic’s spread. The measures included increasing the distance between beds to convert three-patient rooms into two-patient rooms. Each patient who required a caregiver was allocated one, and all caregivers received education on hand hygiene and were required to wear facial masks. The fear of COVID-19 among people led to high compliance with prevention and control measures, significantly reducing the risk of hospital-acquired respiratory infections. Consequently, the incidence of hospital-acquired respiratory infections in our study decreased from 4.2 to 2.9% compared to the pre-COVID-19 pandemic. As polices for COVID-19 prevention and control varied by country, this may have contributed to the variation in HAIs incidence. The incidence of hospital-acquired respiratory infections in our study was similar to the results of two studies conducted in China. The nosocomial infection rate reduced significantly during the COVID-19 pandemic, primarily observed in respiratory infections [7, 28]. These results suggest that the preventive and control measures during the COVID-19 pandemic might reduce the incidence of HAIs. However, another retrospective study in China demonstrated that the preventive and control measures provided benefits during the COVID-19 pandemic; however, their effects on hospitalized acquired respiratory infections were unclear. There were no significant differences in the percentage of lower respiratory tract HAIs from 2018 to 2020 [8]. More studies concerning both exogenous and endogenous factors for HAIs are needed.
The all-cause mortality rate of patients with hospital-acquired respiratory infections in our study was 34.03%, which was higher than previous studies, that reported rates ranging from 13–22.6% [29,30,31]. One possible reason for this discrepancy was the higher proportion of older patients and patients with comorbidities in our study, with 98.42% of patients having one or more comorbidities. Notably, we found that a history of previous malignancy was associated with a higher in-hospital mortality. Conversely, previous studies have identified various risk factors such as active immunosuppressant therapy, solid tumors, coma, clinical pulmonary infection score (CPIS) of 7 or higher, infections occurring in the ICU, age of 65 or older, tracheal cannula insertion, and the number of comorbidities [29,30,31]. The differences in the patient population, particularly the higher proportion of patients aged 65 or older with multiple comorbidities treated in non-ICU wards in our study, might explain the variation in the independent mortality risk factors observed compared with other studies. More large-sample, multicenter studies are needed in the future to explore the factors for mortality of hospital-acquired respiratory infections. In our study, admission during the COVID-19 pandemic exhibited no effect on the mortality of hospital-acquired respiratory infections. This might be due to China’s prevention and control policy for COVID-19 at that time. During the COVID-19 pandemic, patients who tested positive for COVID-19 were treated at an infectious disease specialist hospital. At the hospital where the study was conducted, inpatients with suspected respiratory infection symptoms were tested for COVID-19. Consequently, the transmission of coronavirus in hospitals was interrupted.
Limitations
First, we might underestimate the incidence of hospital-acquired respiratory infections as we only reviewed medical records with a diagnosis of hospital-acquired respiratory infections. We might have missed some hospital-acquired respiratory viral infections as we only tested for coronavirus 2019. Second, in 2020, fewer patients met the screening criterion compared with 2019 which resulted in a lower proportion of medical records being screened for hospital-acquired respiratory infections, potentially leading to the detection of fewer cases. However, a cross-table analysis indicated that there was no significant difference between these two periods. Third, due to the retrospective nature of the study, it was not possible to assess patients’ severity scores, detailed treatment data and the onset time of hospital-acquired respiratory infections. There were a large number of unqualified sputum samples in this study. In future studies, patients should be provided with education about how to produce sputum samples and other specimen types should be selected for patients who cannot cooperate with sputum excretion. Finally, it was a single-center study. Our findings cannot be generalized to all patients in China.
Conclusion
Our study revealed that the incidence of hospital-acquired respiratory infections was significantly decreased possibly due to the implementation of various prevention and control measures during the COVID-19 pandemic. However, admission during the COVID-19 pandemic demonstrated no effect on mortality of hospital-acquired respiratory infections. It may suggest the necessity for adopting infection prevention and control measures, such as reducing unnecessary visits, fixing caregivers, increasing bed space (at least 1 m), supervising the implantation of hand hygiene and wearing facial masks. Moreover, we should pay special attention to patients who were with a history of previous malignancy, as they exhibit higher in-hospital mortality.
Data availability
The raw data required to reproduce the above findings cannot be shared at this time due to legal/ethical reasons, but are available from the corresponding author on reasonable request.
Abbreviations
- CKD:
-
Chronic kidney disease
- COVID-19:
-
The coronavirus disease 2019
- CPIS:
-
Clinical pulmonary infection score
- HAIs:
-
Healthcare-associated infections
- HAP:
-
Hospital-acquired pneumonia
- HH:
-
Hand hygiene
- ICU:
-
Intensive care unit
- MDR:
-
Multiple Drug Resistance
- PPE:
-
Personal protective equipment
- VAP:
-
Ventilator associated pneumonia
References
Allegranzi B, Bagheri NS, Combescure C, Graafmans W, Attar H, Donaldson L, Pittet D. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet. 2011;377(9761):228–41.
Wang J, Liu F, Tartari E, Huang J, Harbarth S, Pittet D, Zingg W. The prevalence of healthcare-associated infections in Mainland China: a systematic review and meta-analysis. Infect Cont Hosp Ep. 2018;39(6):701–9.
Zhang Y, Du M, Johnston JM, Andres EB, Suo J, Yao H, Huo R, Liu Y, Fu Q. Incidence of healthcare-associated infections in a tertiary hospital in Beijing, China: results from a real-time surveillance system. Antimicrob Resist In. 2019;8:145.
Lyons PG, Kollef MH. Prevention of hospital-acquired pneumonia. Curr Opin Crit Care. 2018;24(5):370–8.
Magill SS, O’Leary E, Janelle SJ, Thompson DL, Dumyati G, Nadle J, Wilson LE, Kainer MA, Lynfield R, Greissman S, et al. Changes in prevalence of health care-associated infections in U.S. hospitals. New Engl J Med. 2018;379(18):1732–44.
Torres A. The new American Thoracic Society/Infectious Disease Society of North America guidelines for the management of hospital-acquired, ventilator-associated and healthcare-associated pneumonia: a current view and new complementary information. Curr Opin Crit Care. 2006;12(5):444–5.
Rong R, Lin L, Yang Y, Zhao S, Guo R, Ye J, Zhu X, Wen Q, Liu D. Trending prevalence of healthcare-associated infections in a tertiary hospital in China during the COVID-19 pandemic. BMC Infect Dis. 2023;23(1):41.
Chen C, Zhu P, Zhang Y, Liu B. Effect of the normalized epidemic prevention and control requirements on hospital-acquired and community-acquired infections in China. BMC Infect Dis. 2021;21(1):1178.
Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36(5):309–32.
Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF, File TJ, Musher DM, Niederman MS, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27–72.
Gao C, Wang Y, Gu X, Shen X, Zhou D, Zhou S, Huang JA, Cao B, Guo Q. Association between cardiac injury and mortality in hospitalized patients infected with avian influenza A (H7N9) virus. Crit Care Med. 2020;48(4):451–8.
Pezhman B, Fatemeh R, Amir R, Mahboobeh R, Mohammad F. Nosocomial infections in an Iranian educational hospital: an evaluation study of the Iranian nosocomial infection surveillance system. BMC Infect Dis. 2021;21(1):1256.
Giuliano KK, Baker D, Quinn B. The epidemiology of nonventilator hospital-acquired pneumonia in the United States. Am J Infect Control. 2018;46(3):322–7.
Rosario BH, Shafi H, Yii A, Tee LY, Ang A, Png GK, Ang W, Lee YQ, Tan PT, Sahu A, et al. Evaluation of multi-component interventions for prevention of nosocomial pneumonia in older adults: a randomized, controlled trial. Eur Geriatr Med. 2021;12(5):1045–55.
Zhao X, Wang L, Wei N, Zhang J, Ma W, Zhao H, Han X. Epidemiological and clinical characteristics of healthcare-associated infection in elderly patients in a large Chinese tertiary hospital: a 3-year surveillance study. BMC Infect Dis. 2020;20(1):121.
Jiao J, Yang XY, Li Z, Zhao YW, Cao J, Li FF, Liu Y, Liu G, Song BY, Jin JF, et al. Incidence and related factors for hospital-acquired pneumonia among older bedridden patients in China: a hospital-based multicenter registry data based study. Front Public Health. 2019;7:221.
Metersky ML, Wang Y, Klompas M, Eckenrode S, Bakullari A, Eldridge N. Trend in ventilator-associated pneumonia rates between 2005 and 2013. Jama-J Am Med Assoc. 2016;316(22):2427–9.
Fine LS. Non-ventilator health care-associated pneumonia (NV-HAP): pathogenesis and microbiology of NV-HAP. Am J Infect Control. 2020;48(5S):A7–9.
Han C, Song Q, Meng X, Lv Y, Hu D, Jiang X, Sun L. Effects of a 4-year intervention on hand hygiene compliance and incidence of healthcare associated infections: a longitudinal study. Infection. 2021;49(5):977–81.
Qin JJ, Xing YF, Ren JH, Chen YJ, Gan YF, Jiang YQ, Chen J, Li X. Mandatory mask-wearing and hand hygiene associated with decreased infectious diseases among patients undergoing regular hemodialysis: a historical-control study. Front Public Health. 2021;9:678738.
Liu C, Cao Y, Lin J, Ng L, Needleman I, Walsh T, Li C. Oral care measures for preventing nursing home-acquired pneumonia. Cochrane Db Syst Rev. 2018;9(9):D12416.
Kaneoka A, Pisegna JM, Miloro KV, Lo M, Saito H, Riquelme LF, LaValley MP, Langmore SE. Prevention of healthcare-associated pneumonia with oral care in individuals without mechanical ventilation: a systematic review and meta-analysis of randomized controlled trials. Infect Cont Hosp Ep. 2015;36(8):899–906.
Roquilly A, Marret E, Abraham E, Asehnoune K. Pneumonia prevention to decrease mortality in intensive care unit: a systematic review and meta-analysis. Clin Infect Dis. 2015;60(1):64–75.
Barasheed O, Almasri N, Badahdah AM, Heron L, Taylor J, McPhee K, Ridda I, Haworth E, Dwyer DE, Rashid H, et al. Pilot randomised controlled trial to test effectiveness of facemasks in preventing influenza-like illness transmission among Australian Hajj pilgrims in 2011. Infect Disord Drug Targets. 2014;14(2):110–6.
Lim CY, Bohn MK, Lippi G, Ferrari M, Loh TP, Yuen KY, Adeli K, Horvath AR. Staff rostering, split team arrangement, social distancing (physical distancing) and use of personal protective equipment to minimize risk of workplace transmission during the COVID-19 pandemic: a simulation study. Clin Biochem. 2020;86:15–22.
Kim BG, Kang M, Lim J, Lee J, Kang D, Kim M, Kim J, Park H, Min KH, Cho J, et al. Comprehensive risk assessment for hospital-acquired pneumonia: sociodemographic, clinical, and hospital environmental factors associated with the incidence of hospital-acquired pneumonia. BMC Pulm Med. 2022;22(1):21.
Stiller A, Salm F, Bischoff P, Gastmeier P. Relationship between hospital ward design and healthcare-associated infection rates: a systematic review and meta-analysis. Antimicrob Resist In. 2016;5:51.
Pan SJ, Hou Y, Yang YP, Wang GG, Chen XY, Qian WY, Tung TH, Hu XM. Relationship between nosocomial infections and coronavirus disease 2019 in the neurosurgery unit: clinical characteristics and outcomes from a Chinese tertiary-care hospital. BMC Infect Dis. 2022;22(1):836.
Yin Y, Zhao C, Li H, Jin L, Wang Q, Wang R, Zhang Y, Zhang J, Wang H. Clinical and microbiological characteristics of adults with hospital-acquired pneumonia: a 10-year prospective observational study in China. Eur J Clin Microbiol. 2021;40(4):683–90.
Zhao C, Chen H, Wang H, Liu W, Zhuo C, Chu Y, Zeng J, Jin Y, Hu Z, Zhang R, et al. Analysis of pathogen spectrum and resistance of clinical common organisms causing bloodstream infections, hospital-acquired pneumonia and intra-abdominal infections from thirteen teaching hospitals in 2013. Zhonghua Yi Xue Za Zhi. 2015;95(22):1739–46.
Jiao J, Li Z, Wu X, Cao J, Liu G, Liu Y, Li F, Zhu C, Song B, Jin J, et al. Risk factors for 3-month mortality in bedridden patients with hospital-acquired pneumonia: a multicentre prospective study. PLoS One. 2021;16(3):e249198.
Acknowledgements
The authors would like to thank the participating investigators of the study.
Funding
This study was funded by the Organization Department of the Beijing Xicheng District Party Committee.
Author information
Authors and Affiliations
Contributions
Q L: study design, data collation, statistical analysis, Article writing. LH Z: Determine the diagnosis of hospital-acquired respiratory infections, statistical analysis. J C: study design. S Q, XT N, RX Z: collation of the data. W H: Determine the diagnosis of hospital-acquired respiratory infections. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Research Ethic Board at Fuxing Hospital Affilicated to Capital Medical University, including a waiver of patient consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, Q., Zhao, L., Chen, J. et al. Decreased hospital-acquired respiratory infections among older inpatients during the COVID-19 pandemic: a retrospective observational study in a general hospital in China. BMC Infect Dis 24, 904 (2024). https://doi.org/10.1186/s12879-024-09779-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09779-y