Abstract
Background
The aim of this study was to investigate the pathogenicity of vancomycin-resistant Enterococcus faecalis (VREs) to human colon cells in vitro.
Methods
Three E. faecalis isolates (2 VREs and E. faecalis ATCC 29212) were cocultured with NCM460, HT-29 and HCT116 cells. Changes in cell morphology and bacterial adhesion were assessed at different time points. Interleukin-8 (IL-8) and vascular endothelial growth factor A (VEGFA) expression were measured via RT-qPCR and enzyme-linked immunosorbent assay (ELISA), respectively. Cell migration and human umbilical vein endothelial cells (HUVECs) tube formation assays were used for angiogenesis studies. The activity of PI3K/AKT/mTOR signaling pathway was measured by Western blotting.
Results
The growth and adhesion of E. faecalis at a multiplicity of infection (MOI) of 1:1 were greater than those at a MOI of 100:1(p < 0.05). Compared to E. faecalis ATCC 29212, VREs showed less invasive effect on NCM460 and HT-29 cells. E. faecalis promoted angiogenesis by secreting IL-8 and VEGFA in colon cells, and the cells infected with VREs produced more than those infected with the standard strain (p < 0.05). Additionally, the PI3K/AKT/mTOR signaling pathway was activated in E. faecalis infected cells, with VREs demonstrating a greater activation compared to E. faecalis ATCC 29212 (p < 0.05).
Conclusion
VREs contribute to the occurrence and development of CRC by promoting angiogenesis and activating the PI3K/AKT/mTOR signaling pathway.
Similar content being viewed by others
Introduction
Enterococcus faecalis is a facultative anaerobic commensal bacterium of the oral cavity and the gastrointestinal tract [1]. However, in susceptible hosts, E. faecalis can cause urinary tract infections, infective endocarditis, or transplant infections [2]. Notably, E. faecalis has become one of the most common pathogens that causes hospital-acquired infections [3]. Furthermore, the emergence of the vancomycin-resistant E. faecalis (VREs) has limited the choice of treatments and has increasingly become a public health threat for hospitals worldwide [4]. VREs infections may lead to significant mortality [5, 6].
Globally, colorectal cancer (CRC) is the third most diagnosed malignancy and the second leading cause of cancer death [7]. Previous studies have demonstrated that the gut microbiota has an essential role in the initiation and promotion of CRC [8]. An imbalance in the intestinal microbiota can affect or impair the integrity of the intestinal epithelium, resulting in inflammation, tumor formation or metastasis progression. Currently, multiple studies have confirmed that the abundance of E. faecalis in the faecal microbiota of CRC patients is significantly greater than that in healthy individuals and patients with intestinal polyps [9,10,11]. E. faecalis can polarize macrophages to produce a bystander effect that causes double-stranded DNA breaks, tetraploidy and chromosomal instability (CIN) in target cells and induces inflammation and CRC in interleukin-10 (IL-10) knockout mice [12]. Additionally, E. faecalis can generate reactive oxygen species (ROS) and extracellular superoxide, thereby triggering genomic instability and inducing mutations that lead to the development of tumor [13]. In addition, the metalloprotease produced by E faecalis, contributes to the development of chronic intestinal inflammation by impairing epithelial barrier integrity [14, 15]. However, most current studies have mainly focused on its function as "driver bacteria" in the occurrence and development of CRC [16]. With the increasing prevalence of VREs, the pathogenicity and underlying mechanisms of VREs in colonic cells have not been determined, and further research is needed on the other roles of VREs in CRC to explore potential treatment targets. Therefore, we explored the pathogenicity of VREs to colonic cells in different stages in vitro.
Materials and methods
Bacterial strains
A total of 2 VREs (4942, 12022) were isolated from clinical specimens for diagnosis and frozen at − 80 ℃ in our laboratory. The details of included isolates were described in our previously published article [17]. E. faecalis ATCC 29212 was used as a control standard strain. The isolates were inoculated on Mueller–Hinton II agar (MHA) for 24 h at 37 ℃.
Cell culture
Two commonly used CRC cell lines (HT-29, HCT116) and one human normal colonic epithelial cell line NCM460 were obtained from the American Type Culture Collection (ATCC, Manassas, VA, USA). HT-29 was highly differentiated, and HCT116 was CRC cell line in situ. The human umbilical vein endothelial cells (HUVECs) were also obtained from ATCC. HT-29 cells were routinely cultured in McCoy’s 5A medium (Gibco, Carlsbad, CA, USA), NCM 460 were grown in RPMI 1640 medium (Gibco, Carlsbad, CA, USA), and the other two cell lines were cultured in Dulbecco’s Modified Eagle’s Medium (DMEM) (Gibco, Carlsbad, CA, USA), both of which contained 10% foetal bovine serum (FBS). All the cells were maintained at 37 ℃ in a humidified 5% CO2 incubator.
Bacterial growth and adhesion assay
An invading bacteria solution with a multiplicity of infection (MOI) of 100:1 or 1:1 was prepared with complete cell culture medium to infect the NCM460 and HT-29 cell lines. The cocultures were incubated at 37 ℃ for 2, 4, 6, 8, 12 and 24 h respectively. The cell morphology was observed using an electron microscope. After incubation, the cell culture medium was recovered by centrifugation at 7000 × g for 6 min, after which the cells were washed twice with sterile phosphate-buffered saline (PBS) (Gibco, Carlsbad, CA, USA). Moreover, non-adhered bacteria were removed by washing with PBS. Cells with adhered bacteria were treated with 250 μl of trypsin–EDTA (Gibco, Carlsbad, CA, USA) followed by the addition of 250 μl of culture medium containing FBS. Serial tenfold dilutions were prepared in PBS for both the cell supernatant and cells and plated onto Mueller–Hinton agar at 37 ℃ for 24 h. The growth and adhesion were expressed as a percentage of the number of bacteria in the supernatant and cells to the initial number of bacteria.
Quantitative real-time PCR
Total RNA was extracted from cells using commercial kit (Yishan Biotech, Shanghai, China) according to the manufacturer’s instructions. The RNA concentration was measured using NanoDrop One Spectrophotometer (Thermo Scientific, USA). Subsequently, 1 μg of total RNA from each sample was reverse transcribed to synthesize complementary DNA (cDNA) using a cDNA synthesis kit (Takara Bio Inc., Japan). The synthesized cDNA was subsequently subjected to real time-PCR on a StepOnePlus™ real-time PCR instrument (Applied Biosystems, Foster, CA, USA) to evaluate the gene expression of IL-8 and VEGFA. GAPDH was used as an internal control. The sequences of primer used were as follows: IL-8 forward, 5’- ACATACTCCAAACCTTTCCACC-3′ and reverse, 5’-AAAACTTCTCCACAACCCTCTG-3′; GAPDH forward, 5’-CTGGGCTACACTGAGCACC-3′ and reverse, 5’-AAGTGGTCGTTGAGGGCAATG-3′. VEGFA forward, 5’-ATGAACTTTCTGCTGTCTTGG-3′ and reverse, 5’- TCACCGCCTCGGCTTGTCACA-3; Each experiment was performed independently three times. The expression of IL-8 and VEGFA genes was normalized to GAPDH and calculated based on the 2−△△CT method.
Bacterial conditioned medium
Prepared the invading bacteria solution with the MOI of 100:1 and 1:1 with complete cell culture medium to infect NCM460, HT-29 and HCT116 cell lines. The co-incubated isolates and cells were cultured continuously for 6 h at 37 ℃. The bacteria culture medium was subsequently centrifuged at 6000 × g for 10 min and filtered through a 0.22 mm pore-size filter to obtain the conditioned medium.
Cell migration assay
Cell Migration Assay Kit (BD Biosciences, NJ, USA) was used to evaluate the migration of HUVECs. Briefly, 250 μl serum-free medium containing 2.0 × 104 HUVECs was added to the upper chamber of an 8-μm pore in a 24-well plate, and 750 μl of conditioned supernatant was added to the lower chamber. Subsequently, the cells were incubated in this system for 24 h at 37 ℃. After removing non-invading cells with cotton swabs, the migrated cells were fixed with 4% paraformaldehyde and stained with 0.1% crystal violet solution (Sigma, St. Louis, MO). Finally, stained cells were counted in at least three randomly selected fields at 100X magnification under a microscope to minimize bias.
Endothelial tube formation assay
HUVECs (2 × 104) were plated in 96-well plates coated with 50 μl Matrigel (BD Biosciences, Bedford, MA) and cultured in conditioned culture medium for 6 h at 37 °C with 5% CO2. Tubules were photographed with a microscope and evaluated by Image-Pro Plus software.
Enzyme-linked immunosorbent assay (ELISA)
The protein levels of IL-8 and VEGFA in the bacterial conditioned supernatant were measured with ELISA kits (Proteintech Group, Wuhan, China, #KE00006 for IL-8; RayBiotech, Inc. Georgia, GA, USA, #ELH-VEGF-1 for VEGFA) according to the manufacturer’s instructions.
Western blot analysis
Total protein was extracted using radio immunoprecipitation assay (RIPA) lysis buffer (Beyotime Institute of Biotechnology, Shanghai, China) buffer containing phosphatase and protease inhibitors. The proteins were quantified using bicinchoninic acid (BCA) assay, separated via 10% SDS-PAGE and subsequently transferred to a polyvinylidene fluoride (PVDF) membrane (Beyotime Institute of Biotechnology, Shanghai, China). The membrane was blocked with 5% BSA for 1 h and then according to the molecular weight, the membrane was cut and incubated overnight with the corresponding primary antibody, including anti-Actin mouse antibody (66009–1-Ig, Proteintech Group, 1:5000), anti-PI3K mouse antibody (60225–1-Ig, Proteintech Group, 1:5000), anti-AKT mouse antibody (60203–2-Ig, Proteintech Group, 1:2000), anti-mTOR rabbit antibody (2972S, Cell Signaling Technology, 1:1000), anti-p-PI3K rabbit antibody (AF3242, Affinity Biosciences, 1:1000), anti-p-AKT mouse antibody (66444–1-Ig, Proteintech Group, 1:2000), anti-p-mTOR rabbit antibody (5536 T, Cell signaling Technology, 1:1000). After washing with Tris-buffered saline plus Tween®20 (TBST), the membranes were incubated with secondary antibody (1:5000) for 1 h, and chemiluminescence was used to visualize the protein bands with X-ray film. The intensity was analyzed by Image J software.
Statistical analysis
All the data analyses in our study were performed using GraphPad Prism 8 (GraphPad, USA). All the experiments were performed in three or more replicates. The data are presented as the mean ± standard deviation (SD). Analysis of variance (ANOVA) was used to compare differences among multiple groups. Comparisons between two groups were performed using Mann–Whitney U-test. p-values < 0.05 indicated statistical significance.
Results
Cell morphology in bacteria adhesion assay
All the included isolates were suspended at concentrations of 100:1 and 1:1 in cell culture medium. With the extension of coculture time, we observed that the bacteria continuously reproduced, while the cells gradually swelled, ruptured and died. Moreover, compared to E. faecalis ATCC 29212, VREs were found to be less invasive to NCM460 and HT-29. Treatment with E. faecalis ATCC 29212 resulted in cell death at 6 h, while VREs caused the release of cell secretions at 8 h (Fig. 1 and Supplementary Figure S1).
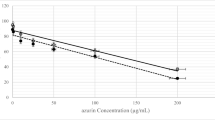
Bacterial growth and adhesiveness
As shown in Fig. 2(A-F), the proliferation and adhesion of E. faecalis were significantly increased at the low MOI. At the time point of 12 h, the proliferation ability and the adhesion capacity of E. faecalis under the low MOI were more than 1.3 times that of high MOI (p < 0.05).
The growth and adhesion assay of two VREs (4942, 12022) and E. faecalis ATCC 29212. A, B, C, D, E, F The solid lines indicated multiplicity of infection (MOI) 100:1 and the dotted lines indicated MOI 1:1. The orange line represents the bacterial growth curve (GC) and the blue line represents the adhesion curve (AC). The left panel represents NCM460, and the right panel represents HT-29. G The adhesion of E. faecalis to two cell lines after coculturing for 12 h. The orange bars represent MOI 100:1 and the blue bars represent MOI 1:1. Results are presented as mean ± SD (n = 3)
In addition, after coculture for 12 h, the adhesion of E. faecalis to the CRC cell line HT-29 was stronger than that to the normal colonic epithelial cell NCM460 (Fig. 2G).
Furthermore, we compared the proliferation and adhesion of the three strains at the MOI of 1:1. It was found that E. faecalis ATCC 29212 was markedly more abundant than VREs (Fig. 3) (p ≤ 0.0481), which was also consistent with earlier observations regarding the cell death time after infection. And after coculturing for 12 h, the proliferation and adhesion of E. faecalis ATCC 29212 were 1.2 times more than VREs.
The comparison of growth and adhesion ability between three E. faecalis strains at the MOI of 1:1. A, B The bacterial growth curve. C, D The bacterial adhesion curve. The red line represents VREs 4942; the green line represents VREs 12022; The blue line represents E. faecalis ATCC 29212. Results are presented as mean ± SD (n = 3)
VREs promoted the expression of IL-8 and VEGFA in colon cell lines cells
The mRNA expression of IL-8 and VEGFA were significantly upregulated in all the three cells cocultured with E. faecalis (Fig. 4A-B). Specifically, the expression of IL-8 and VEGFA in the experimental groups were more than twice that of the control group, with IL-8 exceeding 60 times and VEGFA exceeding 10 times (p < 0.0001).
VREs promoted the expression of IL-8 and VEGFA in colonic cell lines. A, B The expression of IL-8 and VEGFA were detected by RT-qPCR in NCM460, HCT116 and HT-29 cells cocultured with E. faecalis (4942, 12022 and E. faecalis ATCC 29212). Results are expressed as fold increase of control. C, D The concentration of IL-8 and VEGFA in the culture supernatant were examined by Elisa. Data are mean ± SD (n = 3)
In addition, ELISA assays demonstrated that E. faecalis significantly increased the extracellular secretion of IL-8 and VEGFA compared to normal control, and the highest values exceeded 13 times and 3 times, respectively(p < 0.0001). Furthermore, cells infected with VREs produced more than twice as much IL-8 and VEGFA as cells infected with E. faecalis ATCC 29212(p ≤ 0.0186) (Fig. 4C-D).
VREs promotes angiogenesis in vitro
Endothelial cell migration is critical for angiogenesis. Therefore, we evaluated the potential role of E. faecalis on angiogenesis in vitro through the migration and tube formation of HUVECs. As with IL-8 and VEGFA secretion, VREs conditioned medium significantly promoted HUVECs migration(p = 0.0003) (Fig. 5A) and tube formation ability of HUVECs (Fig. 5B) (p = 0.0006). These results confirmed the important effect of VREs on angiogenesis in HUVECs.
VREs stimulated endothelial cell migration and tube formation. A Cell migration in HUVECs were examined by transwell assays after HUVECs were plated and cocultured with the bacterial conditioned medium. One representative image from three reproducible experiments is shown. Scale bar, 100 μm. The increasing folds of migrated HUVEC numbers are shown in the bar graph. B HUVECs tube formation were shown in representative images after co-incubating with the bacterial conditioned medium. Scale bar, 200 μm. The increasing folds of tube formation is shown in the bar graph
Activation of the PI3K/AKT/mTOR pathway in cells infected with VREs
Since VREs had a stronger stimulating effect on colon cell lines at the MOI of 100:1, we extracted proteins from infected cells at this concentration. The PI3K/AKT/mTOR signaling pathway was activated in E. faecalis infected cells, and consistent with the secretion of IL-8 and VEGFA, the expression level of phosphorylated proteins induced by VREs were more than twice that of E. faecalis ATCC 29212 (p ≤ 0.0299) (Fig. 6).
The expression of PI3K/AKT/mTOR pathway members were detected by western blot in the three colonic cell lines treated with or without E. faecalis (VREs 4942, 12022 and E. faecalis ATCC 29212).
Discussion
In recent years, E. faecalis has been shown to cause the occurrence and development of CRC through oxidative stress and chromosomal instability [18]. In this study, E. faecalis increased the expression and secretion of IL-8 and VEGFA, and activated the PI3K/AKT/mTOR signaling pathway. In addition, the pathogenicity of VREs was striking.
Our findings showed that E. faecalis with low MOI had stronger adhesion to infected cells. This difference may be related to the living space of bacteria. Competition for space is ubiquitous in the ecology of both micro-organisms and macro-organisms [19]. To survive and thrive under a variety of biotic and abiotic pressures, bacteria must communicate, cooperate, and compete with the surrounding community [20, 21]. As previously reported, bacteria can deliver toxins through Type VI secretion systems (T6SS) and contact-dependent-inhibition (CDI) systems to influence competitors and interact antagonistically to obtain additional living space [22,23,24,25]. T3SS were identified in VREs. Therefore, E. faecalis with low MOI have more space for sustainable growth, which is more conducive to bacterial proliferation and adhesion. In addition, in our study, we demonstrated that E. faecalis has different adhesion abilities to different cells. Compared with the normal colon epithelial cell NCM460, E. faecalis showed stronger adhesion to colon cancer cell HT-29. The expression of some receptors on the surface of colon cancer cells or changes in cancer cell morphology may be related to increased adhesion of bacteria [26].
Overexpression of the PI3K/AKT/mTOR signaling pathway has been reported in different forms of CRC [27, 28]. The activation of PI3K/AKT/mTOR signaling pathway could promote the production of IL-8 [29, 30]. IL-8 has been demonstrated to be a critical cytokine that is involved in CRC progression. IL-8 can promote CRC metastasis by inducing the epithelial-mesenchymal transition (EMT), inhibiting apoptosis and increasing tumor angiogenesis [31]. Furthermore, an increase in the level of IL-8 is associated with poor prognosis and drug resistance in many cancers [32, 33]. Angiogenesis is an essential process for the growth and proliferation of solid tumors [34], and VEGFA is the main mediator of angiogenesis [35, 36]. Current evidence has shown that VEGFA levels and VEGF receptor activity are associated with poor prognosis in CRC patients [37]. Our results indicated that E. faecalis exposure resulted in significant increases in the expression of IL-8 and VEGFA in normal colonic cell and CRC cells. In addition, E. faecalis promoted the migration and tube formation of HUVECs in vitro, suggesting that E. faecalis may be involved in angiogenesis during the development of colorectal cancer. However, further researches are needed to confirm these findings.
Interestingly, compared with those in the standard strain (E. faecalis ATCC 29212), the effects of VREs on the activation of signaling pathway and the secretion of IL-8 and VEGFA in colonic cell lines were significantly greater. However, the invasive effect of VREs was weak in the growth and adhesion experiments. Geraldes et al. [38] suggested that VREs play a leading role in enterococcal infections and considered the primary species in terms of nosocomial infections. The virulence factors of enterococcus can be roughly divided into two distinct groups: those that are secreted and those that are present in the surface of bacterial cells [39]. Cytolysin is one of the earliest secreted virulence factors that was identified in enterococci [40], which can damage host cell membranes and facilitate infection. Other types of cell surface protein virulence factors, such as microbial surface components recognizing adhesive matrix molecules (MSCRAMMs), Esp, aggregation substances (Asp1, Asp10 and Asa1) and Pili (EBP, BEE, PGC1-4), which have been found to be important for a range of different bacterial defense mechanisms, including biofilm formation and protection of the host immune system [41,42,43]. In our previous study, we demonstrated that VREs exhibited high-level resistance but only harbor virulence genes related to cytolysin and the biofilm forming ability of VREs was weaker than that of standard strains [17]. Therefore, due to the fewer cell surface virulence factors of VREs, it is possible that these strains exhibit weaker adhesion to colonic cells, leading to a more lasting and stronger activation in coculture systems.
Although this study is exploratory in nature, there were several limitations. First, the sample sizes of the experimental strains and cells were small. Second, animal experiments were not performed. Further animal studies or clinical trials are warranted to validate these findings.
Conclusion
In conclusion, our findings showed that VREs may promote the secretion of IL-8 and VEGFA and activate the PI3K/AKT/mTOR signaling pathway, resulting in an angiogenic phenotype that stimulates the progression of CRC. This study advanced our understanding of the pathogenicity of E. faecalis, especially drug-resistant strain in CRC. Additional in vivo studies and validation with clinical samples are worth further investigation to explore the molecular mechanism of this microorganism in CRC, in order to expand the relationship between the microbial community and CRC.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Garcia-Solache M, Rice LB. The Enterococcus: a Model of Adaptability to Its Environment. Clin Microbiol Rev. 2019;32(2):e00058-18.
Rosselli Del Turco E, Bartoletti M, Dahl A, Cervera C, Pericas JM. How do I manage a patient with enterococcal bacteraemia? Clin Microbiol Infect. 2021;27(3):364–71.
Ch’ng JH, Chong KKL, Lam LN, Wong JJ, Kline KA. Biofilm-associated infection by enterococci. Nat Rev Microbiol. 2019;17(2):82–94.
Miller WR, Murray BE, Rice LB, Arias CA. Vancomycin-resistant enterococci: therapeutic challenges in the 21st Century. Infect Dis Clin North Am. 2016;30(2):415–39.
Brinkwirth S, Ayobami O, Eckmanns T, Markwart R. Hospital-acquired infections caused by enterococci: a systematic review and meta-analysis, WHO European Region, 1 January 2010 to 4 February 2020. Euro Surveill. 2021;26(45):2001628.
Cairns KA, Udy AA, Peel TN, Abbott IJ, Dooley MJ, Peleg AY. Therapeutics for Vancomycin-Resistant Enterococcal Bloodstream Infections. Clin Microbiol Rev. 2023;36(2):e0005922.
Keum N, Giovannucci E. Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat Rev Gastroenterol Hepatol. 2019;16(12):713–32.
Gu M, Yin W, Zhang J, Yin J, Tang X, Ling J, et al. Role of gut microbiota and bacterial metabolites in mucins of colorectal cancer. Front Cell Infect Microbiol. 2023;13:1119992.
D’Asheesh TA, Hussen BM, Al-Marzoqi AH, Ghasemian A. Assessment of oncogenic role of intestinal microbiota in colorectal cancer patients. J Gastrointest Cancer. 2021;52(3):1016–21.
Geravand M, Fallah P, Yaghoobi MH, Soleimanifar F, Farid M, Zinatizadeh N, et al. Investigation of enterococcus faecalis population in patients with polyp and colorectal cancer in comparison of healthy individuals. Arq Gastroenterol. 2019;56(2):141–5.
Khodaverdi N, Zeighami H, Jalilvand A, Haghi F, Hesami N. High frequency of enterotoxigenic Bacteroides fragilis and Enterococcus faecalis in the paraffin-embedded tissues of Iranian colorectal cancer patients. BMC Cancer. 2021;21(1):1353.
Wang X, Yang Y, Huycke MM. Commensal bacteria drive endogenous transformation and tumour stem cell marker expression through a bystander effect. Gut. 2015;64(3):459–68.
de Almeida CV, Taddei A, Amedei A. The controversial role of Enterococcus faecalis in colorectal cancer. Therap Adv Gastroenterol. 2018;11:1756284818783606.
Steck N, Hoffmann M, Sava IG, Kim SC, Hahne H, Tonkonogy SL, et al. Enterococcus faecalis metalloprotease compromises epithelial barrier and contributes to intestinal inflammation. Gastroenterology. 2011;141(3):959–71.
Shogan BD, Belogortseva N, Luong PM, Zaborin A, Lax S, Bethel C, et al. Collagen degradation and MMP9 activation by Enterococcus faecalis contribute to intestinal anastomotic leak. Sci Transl Med. 2015;7(286):286ra68.
Tjalsma H, Boleij A, Marchesi JR, Dutilh BE. A bacterial driver-passenger model for colorectal cancer: beyond the usual suspects. Nat Rev Microbiol. 2012;10(8):575–82.
Tong J, Jiang Y, Xu H, Jin X, Zhang L, Ying S, et al. In vitro antimicrobial activity of fosfomycin, rifampin, vancomycin, daptomycin alone and in combination against vancomycin-resistant enterococci. Drug Des Devel Ther. 2021;15:3049–55.
Karpinski TM, Ozarowski M, Stasiewicz M. Carcinogenic microbiota and its role in colorectal cancer development. Semin Cancer Biol. 2022;86(Pt 3):420–30.
Lloyd DP, Allen RJ. Competition for space during bacterial colonization of a surface. J R Soc Interface. 2015;12(110):0608.
Nadell CD, Drescher K, Foster KR. Spatial structure, cooperation and competition in biofilms. Nat Rev Microbiol. 2016;14(9):589–600.
Flemming HC, Wingender J, Szewzyk U, Steinberg P, Rice SA, Kjelleberg S. Biofilms: an emergent form of bacterial life. Nat Rev Microbiol. 2016;14(9):563–75.
Russell AB, Peterson SB, Mougous JD. Type VI secretion system effectors: poisons with a purpose. Nat Rev Microbiol. 2014;12(2):137–48.
Trunk K, Peltier J, Liu YC, Dill BD, Walker L, Gow NAR, et al. The type VI secretion system deploys antifungal effectors against microbial competitors. Nat Microbiol. 2018;3(8):920–31.
Aoki SK, Pamma R, Hernday AD, Bickham JE, Braaten BA, Low DA. Contact-dependent inhibition of growth in Escherichia coli. Science. 2005;309(5738):1245–8.
Ruhe ZC, Low DA, Hayes CS. Bacterial contact-dependent growth inhibition. Trends Microbiol. 2013;21(5):230–7.
Long X, Wong CC, Tong L, Chu ESH, Ho Szeto C, Go MYY, et al. Peptostreptococcus anaerobius promotes colorectal carcinogenesis and modulates tumour immunity. Nat Microbiol. 2019;4(12):2319–30.
Luo C, Cen SY, Ding GJ, Wu W. Mucinous colorectal adenocarcinoma: clinical pathology and treatment options. Cancer Commun. 2019;39(1):13.
Silva VR, Santos LD, Dias RB, Quadros CA, Bezerra DP. Emerging agents that target signaling pathways to eradicate colorectal cancer stem cells. Cancer Commun. 2021;41(12):1275–313.
Kahraman DC, Kahraman T, Cetin-Atalay R. Targeting PI3K/Akt/mTOR pathway identifies differential expression and functional role of IL8 in Liver Cancer Stem Cell Enrichment. Mol Cancer Ther. 2019;18(11):2146–57.
Lin J, He Y, Wang B, Xun Z, Chen S, Zeng Z, et al. Blocking of YY1 reduce neutrophil infiltration by inhibiting IL-8 production via the PI3K-Akt-mTOR signaling pathway in rheumatoid arthritis. Clin Exp Immunol. 2019;195(2):226–36.
Liu Q, Li A, Tian Y, Wu JD, Liu Y, Li T, et al. The CXCL8-CXCR1/2 pathways in cancer. Cytokine Growth Factor Rev. 2016;31:61–71.
Cheng Y, Ma XL, Wei YQ, Wei XW. Potential roles and targeted therapy of the CXCLs/CXCR2 axis in cancer and inflammatory diseases. Biochim Biophys Acta Rev Cancer. 2019;1871(2):289–312.
Fousek K, Horn LA, Palena C. Interleukin-8: A chemokine at the intersection of cancer plasticity, angiogenesis, and immune suppression. Pharmacol Therapeut. 2021;219:107692.
Folkman J. Angiogenesis. Annu Rev Med. 2006;57:1–18.
Apte RS, Chen DS, Ferrara N. VEGF in signaling and disease: beyond discovery and development. Cell. 2019;176(6):1248–64.
Lugano R, Ramachandran M, Dimberg A. Tumor angiogenesis: causes, consequences, challenges and opportunities. Cell Mol Life Sci. 2020;77(9):1745–70.
Lopez A, Harada K, Vasilakopoulou M, Shanbhag N, Ajani JA. Targeting angiogenesis in colorectal carcinoma. Drugs. 2019;79(1):63–74.
Geraldes C, Tavares L, Gil S, Oliveira M. Enterococcus Virulence and Resistant Traits Associated with Its Permanence in the Hospital Environment. Antibiotics (Basel). 2022;11(7):857.
Gao W, Howden BP, Stinear TP. Evolution of virulence in Enterococcus faecium, a hospital-adapted opportunistic pathogen. Curr Opin Microbiol. 2018;41:76–82.
Jett BD, Huycke MM, Gilmore MS. Virulence of Enterococci. Clin Microbiol Rev. 1994;7(4):462–0.
Fabretti F, Theilacker C, Baldassarri L, Kaczynski Z, Kropec A, Holst O, et al. Alanine esters of enterococcal lipoteichoic acid play a role in biofilm formation and resistance to antimicrobial peptides. Infect Immun. 2006;74(7):4164–71.
Geiss-Liebisch S, Rooijakkers SHM, Beczala A, Sanchez-Carballo P, Kruszynska K, Repp C, et al. Secondary Cell Wall Polymers of Are Critical for Resistance to Complement Activation via Mannose-binding Lectin. J Biol Chem. 2012;287(45):37769–77.
Hendrickx APA, Willems RJL, Bonten MJM, van Schaik W. LPxTG surface proteins of enterococci. Trends Microbiol. 2009;17(9):423–30.
Funding
This research was supported by Department of Health of Zhejiang province [2020KY409].
Author information
Authors and Affiliations
Contributions
Li Zhang and Jing Liu performed the experiments. Jiajie Zhang and Mingxia Deng analyzed the data. Li Zhang and Wei Yu wrote the paper. Fangyu Wang and Wei Yu conceptualized the idea and reviewed the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
In our study, we did not perform any experiments with animals or higher invertebrates, neither performed experiments on humans nor the use of human tissue samples. Therefore, our research was exempt from ethics approval.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, L., Deng, M., Liu, J. et al. The pathogenicity of vancomycin-resistant Enterococcus faecalis to colon cancer cells. BMC Infect Dis 24, 230 (2024). https://doi.org/10.1186/s12879-024-09133-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09133-2