Abstract
Background
Hospital admission outcomes for people living with HIV (PLHIV) in resource-limited settings are understudied. We describe in-hospital mortality and associated clinical-demographic factors among PLHIV admitted at a tertiary-level public hospital in Uganda.
Methods
We performed a cross-sectional analysis of routinely collected data for PLHIV admitted at Kiruddu National Referral Hospital between March 2020 and March 2023. We estimated the proportion of PLHIV who had died during hospitalization and performed logistic regression modelling to identify predictors of mortality.
Results
Of the 5,827 hospitalized PLHIV, the median age was 39 years (interquartile range [IQR] 31–49) and 3,293 (56.51%) were female. The median CD4 + cell count was 109 cells/µL (IQR 25–343). At admission, 3,710 (63.67%) were active on antiretroviral therapy (ART); 1,144 (19.63%) had interrupted ART > 3 months and 973 (16.70%) were ART naïve. In-hospital mortality was 26% (1,524) with a median time-to-death of 3 days (IQR 1–7). Factors associated with mortality (with adjusted odds ratios) included ART interruption, 1.33, 95% confidence intervals (CI) 1.13–1.57, p 0.001; CD4 + counts ≤ 200 cells/µL 1.59, 95%CI 1.33–1.91, p < 0.001; undocumented CD4 + cell count status 2.08, 95%CI 1.73–2.50, p < 0.001; impaired function status 7.35, 95%CI 6.42–8.41, p < 0.001; COVID-19 1.70, 95%CI 1.22–2.37, p 0.002; liver disease 1.77, 95%CI 1.36–2.30, p < 0.001; co-infections 1.53, 95%CI 1.32–1.78, p < 0.001; home address > 20 km from hospital 1.23, 95%CI 1.04–1.46, p 0.014; hospital readmission 0.7, 95%CI 0.56–0.88, p 0.002; chronic lung disease 0.62, 95%CI 0.41–0.92, p 0.019; and neurologic disease 0.46, 95%CI 0.32–0.68, p < 0.001.
Conclusion
One in four admitted PLHIV die during hospitalization. Identification of risk factors (such as ART interruption, function impairment, low/undocumented CD4 + cell count), early diagnosis and treatment of co-infections and liver disease could improve outcomes.
Similar content being viewed by others
Introduction
Access to antiretroviral therapy (ART) has significantly decreased the global deaths associated with the Human Immunodeficiency virus (HIV) infection. More than 29 million people living with HIV (PLHIV) were on ART by 2022, with HIV-associated deaths averted by up to 69% since the peak in 2004 [1]. Despite the improved access to ART, 630,000 global HIV-associated deaths were reported in 2022 with three in five deaths occurring in the African region [1]. HIV-associated mortality amongst hospitalized PLHIV in Africa is high, ranging between 13.6 and 38% [2,3,4,5]. Factors such as undiagnosed HIV status [6], low CD4 + cell counts [7, 8], tuberculosis [9], and co-infections [2,3,4] are among the common predictors of mortality among hospitalized PLHIV.
Uganda has made significant strides towards achieving the 95-95-95 HIV care cascade targets with more than 90% of PLHIV aware of their HIV status and 85% accessing ART [10]. However, despite these gains, an estimated 54,000 new HIV infections and 17,000 HIV-associated deaths were reported in 2022 [10]. There is a paucity of data on the factors associated with mortality among hospitalized PLHIV in Uganda. A recent study found that HIV disease was one of the leading causes of mortality among patients admitted at a major tertiary hospital in Uganda but did not explore the factors that predicted mortality in the HIV subpopulation [11]. An earlier study done before the test-and-treat era found an association between opportunistic infections and mortality among hospitalized PLHIV [12].
In March 2020, Makerere University Joint AIDS Program (MJAP) and Kiruddu National Referral Hospital (KNRH) partnered with the Infectious Diseases Institute (IDI) to establish a pilot program to support care for hospitalized PLHIV at KNRH. This was part of the Kampala HIV project run by the IDI with funding from the President’s Emergency Plan for AIDS Relief (PEPFAR), through the Centres for Disease Control and Prevention (CDC) [13]. The program aimed to reduce HIV-associated morbidity and mortality through the provision of extended support services for hospitalized PLHIV. The services offered included targeted HIV screening at the emergency department, diagnosis and treatment of opportunistic infections (OIs) and comorbidities, ART initiation and support counselling services, post-discharge counselling, and post-discharge linkage to care, as well as training of KNRH healthcare providers in managing HIV disease. These activities were based on the 2020 Ugandan National HIV Care and Treatment guidelines [14] and were integrated into the routine hospital procedures of KNRH. We analyzed the in-hospital mortality rate and predicting clinical and demographic factors among PLHIV admitted to KNRH between March 2020 and March 2023.
Methods
Study design and setting
This cross-sectional study was conducted at KNRH, a national referral hospital with a bed capacity of 200 and serves more than 100,000 patients annually [15] The hospital offers a range of medical and diagnostic services to the catchment population and established the first elaborate support program for hospitalized PLHIV in the country [13, 15].
Study population
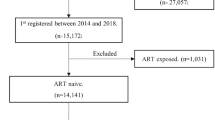
The study population included all identified PLHIV aged ≥ 12 years who were hospitalized at KNRH between March 2020 and March 2023.
Sampling methods
All identified PLHIV admitted at KNRH between March 2020 and March 2023 were included in the study.
Study procedure
We extracted, cleaned and entered de-identified data of patient health records into a password protected backed-up electronic Excel database. The clinical endpoint was the patient’s vital status “Alive” or “Dead” outcome at discharge/transfer from KNRH. Data on independent social-demographic variables included age, sex and distance of patients’ home addresses from KNRH estimated in kilometres (km) using arbitrary cut-offs of < 10 km, 10–20 km and > 20 km. clinical data variables included CD4 + cell counts, viral load, ART history (naïve or experienced at admission, adherence counselling), clinical diagnoses and function assessment scores (using the Eastern Cooperative Oncology Group (ECOG) score). ECOG scores of 3–4 were categorized as “poor function status”, indicating severe function impairment, while ECOG scores of 1–2 were categorized as “good function status” indicating mild to moderate function impairment).
Clinical diagnoses were categorized as “opportunistic infections” or “comorbidities.” The opportunistic infections (OIs) included TB, Cryptococcal disease, candidiasis, toxoplasmosis, and Kaposi sarcoma. The comorbidities included cardiovascular diseases, diabetes mellitus, kidney disease, liver disease, neurologic disorders, chronic lung diseases, cancers, anaemia and other co-infections (excluding OIs). Table 1 summarizes the definitions and categorization of the clinical diagnoses.
ART status at admission was categorized as “Active,” “Interrupted” or “Naïve” as guided by the 2020 National treatment guidelines. Patients who had never received ART (whether newly diagnosed or previously known HIV) were categorized as “ART Naïve” while a patient who interrupted ART ≥ three months before the current hospital admission was considered to have “Interrupted ART”. Patients were considered “Active on ART” if they or their attendants reported consistent use of ART regardless of duration at admission or if they had interrupted ART for a period < three months before admission.
Statistical analysis
The primary outcome, mortality, was determined as the number of PLHIV who died divided by the total number of PLHIV that were admitted. Univariate analysis was performed to summarize the baseline characteristics of the study participants. For bivariate analysis, we used the Pearson chi-square test to determine the association between mortality and patients’ baseline characteristics. Variables with a p value greater than an arbitrary value of 0.25 were excluded from the multivariate analysis.
At multivariate analysis, adjusted odds ratios (AOR) from a multivariate binary logistic regression model were used with two-sided p values < 0.05 considered statistically significant. We performed analysis of variance between independent variables and excluded all variables which were highly correlated with each other, to control for type II errors. Multicollinearity was assessed using the Variance Inflation Factor (VIF) of dummy variables and the mean VIF was 1.36. Goodness of fit was performed after running the binary logistic regression model and was found to be correctly specified at a p value of 0.045. The model assumed characteristics of independence of independent variables, and non-inflated standard errors. Data analysis was done using Stata/MP 14 (Stata Corp LLC, Texas, USA).
Ethical approval
Ethical approval was obtained from the Makerere University, College of Health Sciences, School of Public Health, research ethics committee under Reference MakSPH-REC710 and reference HS553ES under the Uganda National Council for Science and Technology. A waiver for informed consent was obtained since we sought to use only already existing routinely collected, de-identified program data requiring no contact with participants.
Results
Baseline characteristics
Of the 30,537 persons admitted at KNRH from March 2020 to March 2023, 5,827 (19.1%) PLHIV were identified, of whom 3,293 (56.5%) were females. The median age was 39 years (IQR 31–49 years), and the median duration of hospitalization was 5 days (IQR 2–10 days). CD4 + cell count was documented among 3,715 (63.8%) hospitalized PLHIV of whom 2,271 (38.97%) had CD4 + cell count ≤ 200 cells/µL. The median CD4 + cell count was 109 cells/µL (IQR 25–343 cells/µl).
A total of 4,854 (83.3%) PLHIV had initiated ART before admission of whom 3,710 (63.7%) were active on their treatment while 1,144 (19.6%) had interrupted ART longer than three months; 973 (16.7%) were ART naïve. A poor ECOG function assessment (ECOG score 3–4) was observed in 2,225 (38.2%) of hospitalized PLHIV. Table 2 summarizes the baseline characteristics of the patients at admission.
Co-infections and comorbidities
The OIs included TB (1954, 33.53%), Cryptococcal disease (739, 12.68%), candidiasis (443, 7.6%), toxoplasmosis (142, 2.44%) and Kaposi sarcoma (124, 2.13%). Other comorbid diagnoses included co-infections (1,367, 23.46%), cardiovascular disease (975, 16.7%), severe malnutrition (807, 13.9%), anaemia (646, 11.1%) and kidney disease (514, 8.82%). (Table 2).
In-Hospital mortality
A total of 4,303 (73.85%) PLHIV were discharged from the hospital with a median duration of hospitalization of 6 days (IQR 3–11 days), while 1,524 (26.15%) died with a median time to death of 3 days (IQR 1–7 days).
Factors Associated with HIV Mortality
At bivariate analysis, the factors that had a statistically significant association with mortality included age, sex, distance between home address and KNRH, readmission status, ART status, CD4 + cell counts, function assessment, COVID-19, cardiovascular disease, kidney disease, liver disease, anaemia, co-infections, malnutrition, diabetes mellitus, neurologic disorders and chronic lung disease (Table 2).
At multivariate analysis, factors that predicted mortality included function impairment, CD4 + count ≤ 200 cells/µL, undocumented CD4 + status, address > 20 km from hospital, ART interruption, COVID-19, liver disease and co-infections. Factors that were protective of mortality included hospital readmission, chronic lung disease and neurologic disorders (Table 3). Malnutrition, kidney disease, cardiovascular disease, anaemia and age were excluded from the multivariate analysis due to high multicollinearity.
Discussion
In this study, we assessed in-hospital mortality and associated factors among hospitalized PLHIV in Uganda. In this young population with a median age of 39 years, the in-hospital mortality was 26%. Almost two-fifths of the hospitalized PLHIV had advanced HIV disease (CD4 + cell count ≤ 200 cells/µL) and more than a third were not on ART at the time of admission. Factors which predicted in-hospital mortality included ART interruption, CD4 + cell counts ≤ 200 cells/µL, undocumented CD4 + cell counts, function impairment, co-infections, liver disease and long distance from the hospital.
The high mortality observed in our study is of significant concern as over a quarter of the hospitalized PLHIV succumbed to their illness in an era of Universal Test and Treat [16]. This observation is similar to the high in-hospital mortality reported in previous studies, ranging between 14 and 38% across various African settings [2,3,4]. Notably, we observed that most of the deaths occurred within a week of hospitalization which echoes findings from a study in Sierra Leone [3]. Our study site being a tertiary-level health facility raises concerns over patient-related or health system-related factors that contribute to poor healthcare-seeking behaviour and late hospital presentation. The high proportion of hospitalized PLHIV presenting with advanced HIV disease (39%) and significant function impairment (38%) in our study suggests a delayed or late presentation for healthcare [17,18,19]. Health system barriers such as long distance to the hospital could be another contributing factor to poor outcomes among hospitalized PLHIV. We observed that PLHIV who lived > 20 km from the hospital had higher odds of death compared to those who stayed < 10 km from the hospital. This observation agrees with other studies that identified long distance to a health facility as a barrier to accessing healthcare, potentially increasing the risk of mortality [20]. Use of patient-centred differentiated care approaches that take HIV services closer to the PLHIV may help address such barriers [21]. Encouraging early health-seeking behaviour among PLHIV could also improve hospital outcomes.
Of note, more than a third of the hospitalized PLHIV in our study were not on ART (Naïve or interrupted) at the time of admission. We observed that those who had interrupted their ART had 1.3 times the odds of dying during hospitalization compared to those who were active on ART. Our observations agree with other community-based studies that showed that up to a third of PLHIV who disengaged from HIV care were at a higher risk of mortality [22,23,24,25]. Since suboptimal ART coverage is associated with poor survival outcomes, there is an urgent need to understand and address the factors that contribute to patient disengagement from HIV care. Examples of factors that propagate patient disengagement from care include transportation costs [20], food insecurity [26] and the professional behaviour of health workers [27]. Efforts to retain PLHIV at risk of attrition from lifelong ART must be prioritized to optimize outcomes [28].
PLHIV who had poor function status at admission had more than seven times the odds of dying during hospitalization compared to those with good function status. Studies from Uganda and Ethiopia using different function assessment tools also revealed associations between poor function status and mortality among hospitalized PLHIV [12, 29]. In other studies, poor function status predicted late presentation of HIV disease [18, 19]. This evidence suggests that assessing functional status among hospitalized PLHIV is crucial for predicting mortality, allowing for identification of high-risk patients who may benefit from rapid interventions to improve outcomes.
PLHIV who had low CD4 + cell counts ≤ 200 cells/µL had 1.68 times the odds of dying during hospitalization compared to those with higher CD4 cell counts. These findings agree with studies from various settings emphasizing the increased risk of mortality associated with low CD4 + cell counts [7, 8], thus underscoring the importance of enhanced CD4 + screening among hospitalized PLHIV. In addition, PLHIV who did not have a documented CD4 + cell count had double the odds of death during hospitalization compared to those with high CD4 + cell counts. While reasons for this observation are not immediately clear, we postulate that increased mortality is linked to the missed opportunities to screen and diagnose important OIs. A recent national survey found suboptimal levels of CD4 + testing among PLHIV, which translated into a missed opportunity to screen 80% of potential TB and Cryptococcal disease patients [30]. Thus, screening and documentation of CD4 + cell counts could be useful amongst hospitalized PLHIV to improve hospital outcomes.
Tuberculosis, Cryptococcal disease and co-infections were highly prevalent in our study. However, both TB and Cryptococcal disease did not predict mortality despite being known predictors of mortality among hospitalized HIV patients [2, 3, 31, 32]. Plausible explanations for this observation might be due to, (a) the declining incidence of these infections underscoring the vast experience gained in investigations and treatment of OIs [5]; (b) the availability of improved rapid diagnostics such as the lateral flow antigen tests which facilitate early diagnosis and treatment of these infections [33,34,35] or (c) the protective effect of prophylactic treatment such as isoniazid to reduce the incidence of opportunistic infections [36, 37]. These findings re-emphasize the importance of screening, prevention and treatment of opportunistic infections to optimize outcomes among hospitalized PLHIV.
Unlike opportunistic infections, PLHIV who were diagnosed with co-infections or COVID-19 had increased odds of mortality during hospitalization. Several studies agree with these observations where co-infections [3, 4] and COVID-19 infection [38] were associated with increased risk of mortality amongst the hospitalized PLHIV. These findings suggest that co-infections remain an important cause of mortality among hospitalized PLHIV, emphasizing the need for enhanced screening and treatment of such among hospitalized PLHIV.
Hospitalized PLHIV who were diagnosed with liver disease in our study had 1.77 times the odds of dying compared to those without liver disease. These findings agree with other studies that reveal a growing burden of liver disease that predisposes to increased risk of mortality among PLHIV [39,40,41]. Among the common presentations of liver disease among African PLHIV include drug induced liver injury from anti-TB or ART [42, 43], chronic viral infections [44, 45], liver fibrosis [46, 47], and alcoholic liver disease [46, 47]. Screening measures should be enhanced to enable early detection and treatment of high-risk PLHIV who develop liver disease manifestations particularly those on anti-TB medications (due to risk of drug-induced liver injury) or those with viral hepatitis co-infections.
Hospitalized PLHIV who were diagnosed with chronic lung disease had reduced odds of mortality. While we interpret this finding with a degree of uncertainty, existing literature suggests an increasing burden of chronic lung diseases associated with HIV disease such as post-TB lung disease [48,49,50,51], chronic obstructive airway disease [52,53,54], bronchiectasis [55, 56], asthma exacerbations [57] and altered respiratory microbiome predisposing to chronic airway inflammation [58, 59]. However, data on the survival outcomes of PLHIV diagnosed with chronic lung diseases is scarce, with some studies suggesting an increased risk of mortality with HIV disease [57, 59, 60], contrary to our study findings. Further research to better understand the interaction between HIV disease and chronic lung diseases is warranted.
Likewise, hospitalized PLHIV who were diagnosed with neurologic disorders also had reduced odds of mortality in our study. This observation is also not fully understood but one plausible explanation is the fact that such patients are often transferred to another hospital that provides specialized care for neurologic and mental disorders. These masked the true interactions between HIV disease and the comorbidities observed in our study site. Furthermore, the low prevalence of neurologic disorders in our study could have contributed to the masked interaction with HIV disease. Neurologic disorders have varied manifestations in HIV disease such as HIV-associated cognitive disorders [61, 62], seizure disorders [63] and major depressive disorders [64]. Some studies suggest an increased risk of mortality associated with neurologic disorders amongst PLHIV [65]. These complexities highlight the challenges in the care for PLHIV diagnosed with neurologic disorders in resource poor settings but warrant further research to understand the magnitude and interaction with HIV disease.
PLHIV who were readmitted to hospital also had reduced odds of mortality compared to the new admissions. About one in ten PLHIV in our study were readmitted in our study, a finding slightly lower than recent estimates of 18.8% [66]. The protective effect of hospital readmission in our study is not fully understood and equally warrants further research into understanding this interaction.
Study limitations
In this large single site study, we identified factors that predicted in-hospital mortality among hospitalized PLHIV in Uganda. However, we acknowledge a few limitations inherent to the study. One, we lacked autopsy reports to confirm the causes of death among the patients, thus potentially missing some key clinical diagnoses [67]. The causes of death were inferred from the clinical diagnoses since autopsies are not routinely done at the hospital due to multiple reasons such as refusal by family members [68, 69]. Secondly, the lack of a control group (e.g. HIV negative subpopulation) limited further analysis and interpretation of the results. Data from an in-hospital HIV support program was used to inform the study findings. Thirdly, the retrospective nature of the study meant some variables could not be assessed such as cognitive function in neurologic disorders. In addition, some variables demonstrated high correlation with others further complicating interpretation of the findings. High multicollinearity was overcome by excluding such variables at multivariate analysis. Fourthly, the lack of a standardized categorization system for clinical diagnoses meant some variables could have been misdiagnosed or misclassified especially for those with similar presentations such as immune reconstitution inflammatory syndromes and infections. Lastly, our findings are limited to a single tertiary-level hospital which may be skewed towards patients requiring super-specialized healthcare services. The findings may not be generalized to the majority who access healthcare from lower-level health facilities [70]. Despite these limitations, the study findings provide valuable lessons for improving outcomes for hospitalized PLHIV.
Conclusion
One in every four PLHIV is at risk of dying following hospitalization in Uganda. The factors that predicted mortality amongst the hospitalized PLHIV were interruption of antiretroviral therapy, low CD4 + cell counts ≤ 200 cells/µL, unknown CD4 + cell count status, function impairment, co-infections, COVID-19 and liver disease.
There is a need for targeted multisectoral interventions to optimize the care and treatment of hospitalized PLHIV. At an individual level, enhanced HIV testing, early initiation and retention on ART should be prioritized to leverage the benefits of lifelong ART, as well as addressing barriers that hinder timely access to healthcare. At the hospital level, strengthening screening protocols to identify most-at-risk PLHIV such as those with advanced HIV disease or unknown CD4 + cell counts, or function impairment could improve survival through timely interventions such as screening and treatment of co-infections and comorbidities. Patient education on disease prevention particularly regarding the non-communicable diseases such as liver disease, may also help avert poor outcomes following hospitalization. Standardizing health information systems by use of standardized classification tools for clinical diagnoses could improve accurate data interpretation and sharing with relevant stakeholders and health policymakers to better understand disease trends and appropriately allocate resources to respond to emerging healthcare threats.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to the privacy and confidentiality of hospital records but are available from the corresponding author on reasonable request.
Abbreviations
- AOR:
-
Adjusted odds ratio
- ART:
-
Antiretroviral therapy
- CD4+:
-
Cluster of differentiation four positive
- CDC:
-
Centre for Disease Prevention and Control
- CNS:
-
Central nervous system
- COVID:
-
19–Coronavirus disease 2019
- CRAG:
-
Cryptococcal Antigen
- ECOG:
-
Eastern Cooperative Oncology Group
- HIV:
-
Human immunodeficiency virus
- IQR:
-
Inter quartile range
- KNRH:
-
Kiruddu National Referral Hospital
- KM:
-
Kilometers
- LAM:
-
Lipoarabinomannan antigen
- MJAP:
-
Makerere University Joint AIDS Program
- MOH:
-
Ministry of Health Uganda
- OI:
-
Opportunistic Infections
- PEPFAR:
-
President’s Emergency Plan for AIDS Relief
- PLHIV:
-
People living with HIV
- TB:
-
Tuberculosis
References
UNAIDS, Global HIV. & AIDS statistics — Fact sheet| UNAIDS [Internet]. 2022 [cited 2022 Oct 21]. Available from: https://www.unaids.org/en/resources/fact-sheet.
Laher AE, Paruk F, Venter WDF, Ayeni OA, Richards GA. Predictors of in-hospital mortality among HIV-positive patients presenting with an acute illness to the emergency department. HIV Med. 2021;22(7):557–66.
Lakoh S, Jiba DF, Kanu JE, Poveda E, Salgado-Barreira A, Sahr F et al. Causes of hospitalization and predictors of HIV-associated mortality at the main referral hospital in Sierra Leone: a prospective study. BMC Public Health. 2019;19(1).
Lewden C, Drabo YJ, Zannou DM, Maiga MY, Minta DK, Sow PS et al. Disease patterns and causes of death of hospitalized HIV-positive adults in West Africa: a multicountry survey in the antiretroviral treatment era. J Int AIDS Soc. 2014;17(1).
Barak T, Neo DT, Tapela N, Mophuthegi P, Zash R, Kalenga K et al. HIV-associated morbidity and mortality in a setting of high ART coverage: prospective surveillance results from a district hospital in Botswana. J Int AIDS Soc. 2019;22(12).
Moodley Y. The impact of an unknown HIV serostatus on inpatient mortality. Pan Afr Med J [Internet]. 2017 Nov 30 [cited 2021 Dec 31];28. Available from: https://pubmed.ncbi.nlm.nih.gov/29942417/.
Hogg RS, Yip B, Chan KJ, Wood E, Craib KJP, O’Shaughnessy MV et al. Rates of disease progression by baseline CD4 cell count and viral load after initiating triple-drug therapy. JAMA [Internet]. 2001 Nov 28 [cited 2022 May 14];286(20):2568–77. Available from: https://pubmed.ncbi.nlm.nih.gov/11722271/.
Gunda DW, Nkandala I, Kilonzo SB, Kilangi BB, Mpondo BC. Prevalence and risk factors of mortality among adult HIV patients initiating ART in Rural setting of HIV Care and Treatment Services in North Western Tanzania: a retrospective cohort study. J Sex Transm Dis. 2017;2017:1–8.
Ford N, Matteelli A, Shubber Z, Hermans S, Meintjes G, Grinsztejn B et al. TB as a cause of hospitalization and in-hospital mortality among people living with HIV worldwide: a systematic review and meta-analysis. J Int AIDS Soc [Internet]. 2016 Jan 12 [cited 2021 Dec 31];19(1). Available from: https://pubmed.ncbi.nlm.nih.gov/26765347/.
UNAIDS. Uganda| UNAIDS [Internet]. 2022 [cited 2022 Oct 21]. Available from: https://www.unaids.org/en/regionscountries/countries/uganda.
Kalyesubula Id R, Id TR, Andia-Biraro I, Alupo P, Kimuli I, Nabirye S et al. Trends of admissions and case fatality rates among medical in-patients at a tertiary hospital in Uganda; A four-year retrospective study. 2019; https://doi.org/10.1371/journal.pone.0216060.
Namutebi AMN, Kamya MRK, Byakika-Kibwika P. Causes and outcome of hospitalization among HIV-infected adults receiving antiretroviral therapy in Mulago hospital, Uganda. Afr Health Sci [Internet]. 2014 Jan 30 [cited 2022 Jan 19];13(4):977–85. Available from: https://www.ajol.info/index.php/ahs/article/view/100392.
Makerere University Joint AIDS Program. Welcome To Makerere Joint Aids Program [Internet]. 2022 [cited 2022 Jan 1]. Available from: https://mjap.mak.ac.ug/.
Ministry of Health Uganda; MINISTRY OF HEALTH CONSOLIDATED GUIDELINES FOR THE PREVENTION AND TREATMENT OF HIV AND AIDS IN UGANDA 2020 [Internet]. 2020. Available from: https://differentiatedservicedelivery.org/Portals/0/adam/Content/HvpzRP5yUUSdpCe2m0KMdQ/File/Uganda_Consolidated HIV and AIDS Guidelines 2020 June 30th.pdf.
Ministry of Health Uganda; Kiruddu Referral Hospital [Internet]. 2022 [cited 2022 Jan 1]. Available from: https://www.kiruddu.hosp.go.ug/.
World Health Organization.; Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: recommendations for a public health approach. 2021 [cited 2022 Jan 19];131. Available from: https://www.who.int/publications/i/item/9789240031593.
Haas AD, Radin E, Birhanu S, Low AJ, Saito S, Sachathep K et al. Prevalence of and factors associated with late diagnosis of HIV in Malawi, Zambia, and Zimbabwe: Results from population-based nationally representative surveys. PLOS global public health [Internet]. 2022 Feb 22 [cited 2023 Jul 23];2(2):e0000080. Available from: https://pubmed.ncbi.nlm.nih.gov/36962254/.
Gesesew H, Tsehaineh B, Massa D, Tesfay A, Kahsay H, Mwanri L. The prevalence and associated factors for delayed presentation for HIV care among tuberculosis/HIV co-infected patients in Southwest Ethiopia: a retrospective observational cohort. Infect Dis Poverty [Internet]. 2016 Nov 2 [cited 2022 Oct 25];5(1). Available from: https://pubmed.ncbi.nlm.nih.gov/27802839/.
Assen A, Molla F, Wondimu A, Abrha S, Melkam W, Tadesse E et al. Late presentation for diagnosis of HIV infection among HIV positive patients in South Tigray Zone, Ethiopia. BMC Public Health [Internet]. 2016 Jul 12 [cited 2022 Oct 25];16(1). Available from: https://pubmed.ncbi.nlm.nih.gov/27405542/.
Tuller DM, Bangsberg DR, Senkungu J, Ware NC, Emenyonu N, Weiser SD. Transportation costs impede sustained adherence and access to HAART in a clinic population in southwestern Uganda: a qualitative study. AIDS Behav [Internet]. 2010 Aug [cited 2023 Oct 27];14(4):778–84. Available from: https://pubmed.ncbi.nlm.nih.gov/19283464/.
Zakumumpa H, Kwiringira J, Katureebe C, Spicer N. Understanding Uganda’s early adoption of novel differentiated HIV treatment services: a qualitative exploration of drivers of policy uptake. BMC Health Serv Res [Internet]. 2023 Dec 1 [cited 2024 Jan 17];23(1):1–14. Available from: https://bmchealthservres.biomedcentral.com/articles/https://doi.org/10.1186/s12913-023-09313-x.
Anderegg N, Hector J, Jefferys LF, Burgos-Soto J, Hobbins MA, Ehmer J, et al. Loss to follow-up correction increased mortality estimates in HIV-positive people on antiretroviral therapy in Mozambique. J Clin Epidemiol. 2020;128:83–92.
Tymejczyk O, Vo Q, Kulkarni SG, Antelman G, Boshe J, Reidy W, et al. Tracing-corrected estimates of disengagement from HIV care and mortality among patients enrolling in HIV care without overt immunosuppression in Tanzania. AIDS Care. 2021;33(1):47–53.
Wekesa P, McLigeyo A, Owuor K, Mwangi J, Nganga E, Masamaro K. Factors associated with 36-month loss to follow-up and mortality outcomes among HIV-infected adults on antiretroviral therapy in Central Kenya. BMC Public Health. 2020;20(1).
Burkey MD, Weiser SD, Fehmie D, Alamo-Talisuna S, Sunday P, Nannyunja J, et al. Socioeconomic determinants of mortality in HIV: evidence from a clinical cohort in Uganda. J Acquir Immune Defic Syndr. 2014;66(1):41–7.
Hardon AP, Akurut D, Comoro C, Ekezie C, Irunde HF, Gerrits T et al. Hunger, waiting time and transport costs: time to confront challenges to ART adherence in Africa. AIDS Care [Internet]. 2007 [cited 2023 Oct 27];19(5):658–65. Available from: https://pubmed.ncbi.nlm.nih.gov/17505927/.
Ware NC, Wyatt MA, Geng EH, Kaaya SF, Agbaji OO, Muyindike WR et al. Toward an Understanding of Disengagement from HIV Treatment and Care in Sub-Saharan Africa: A Qualitative Study. PLoS Med [Internet]. 2013 Jan [cited 2023 Oct 27];10(1). Available from: /pmc/articles/PMC3541407/.
UNAIDS. 2020. [cited 2022 Jan 19]. 2025 AIDS TARGETS - UNAIDS. Available from: https://aidstargets2025.unaids.org/.
Kebede A, Tessema F, Bekele G, Kura Z, Merga H. Epidemiology of survival pattern and its predictors among HIV positive patients on highly active antiretroviral therapy in Southern Ethiopia public health facilities: a retrospective cohort study. AIDS Res Ther [Internet]. 2020 Aug 5 [cited 2022 Oct 25];17(1). Available from: https://pubmed.ncbi.nlm.nih.gov/32758247/.
Meya DB, Tugume L, Nabitaka V, Namuwenge P, Phiri S, Oladele R et al. Establishing targets for advanced HIV disease: a call to action. South Afr J HIV Med. 2021;22(1).
Ford N, Matteelli A, Shubber Z, Hermans S, Meintjes G, Grinsztejn B et al. TB as a cause of hospitalization and in-hospital mortality among people living with HIV worldwide: a systematic review and meta-analysis. J Int AIDS Soc. 2016;19(1).
Saavedra A, Campinha-Bacote N, Hajjar M, Kenu E, Gillani FS, Obo-Akwa A et al. Causes of death and factors associated with early mortality of HIV-infected adults admitted to Korle-Bu Teaching Hospital. Pan Afr Med J. 2017;27.
Nathavitharana RR, Lederer P, Chaplin M, Bjerrum S, Steingart KR, Shah M. Impact of diagnostic strategies for tuberculosis using lateral flow urine lipoarabinomannan assay in people living with HIV. Cochrane Database Syst Rev. 2021;8(8).
Ricks S, Denkinger CM, Schumacher SG, Hallett TB, Arinaminpathy N. The potential impact of urine-LAM diagnostics on tuberculosis incidence and mortality: a modelling analysis. PLoS Med. 2020;17(12).
Gupta-Wright A, Corbett EL, Wilson D, Van Oosterhout JJ, Dheda K, Huerga H et al. Risk score for predicting mortality including urine lipoarabinomannan detection in hospital inpatients with HIV-associated tuberculosis in sub-Saharan Africa: Derivation and external validation cohort study. PLoS Med [Internet]. 2019 [cited 2023 Oct 28];16(4). Available from: https://pubmed.ncbi.nlm.nih.gov/30951533/.
Zar HJ, Cotton MF, Strauss S, Karpakis J, Hussey G, Schaaf S et al. Effect of isoniazid prophylaxis on mortality and incidence of tuberculosis in children with HIV: randomised controlled trial. BMJ [Internet]. 2007 Jan 20 [cited 2023 Oct 27];334(7585):136–9. Available from: https://pubmed.ncbi.nlm.nih.gov/17085459/.
Briggs MA, Emerson C, Modi S, Taylor NK, Date A. Use of isoniazid preventive therapy for tuberculosis prophylaxis among people living with HIV/AIDS: a review of the literature. J Acquir Immune Defic Syndr [Internet]. 2015 Apr 15 [cited 2023 Oct 27];68 Suppl 3(Suppl 3):S297–305. Available from: https://pubmed.ncbi.nlm.nih.gov/25768869/.
Risk Factors for Coronavirus Disease. 2019 (COVID-19) Death in a Population Cohort Study from the Western Cape Province, South Africa. Clin Infect Dis. 2021;73(7):e2005–15.
Puoti M, Spinetti A, Ghezzi A, Donato F, Zaltron S, Putzolu V et al. Mortality for liver disease in patients with HIV infection: a cohort study. J Acquir Immune Defic Syndr [Internet]. 2000 Jul 1 [cited 2022 Jan 25];24(3):211–7. Available from: https://pubmed.ncbi.nlm.nih.gov/10969344/.
Smith CJ, Ryom L, Weber R, Morlat P, Pradier C, Reiss P et al. Trends in underlying causes of death in people with HIV from 1999 to 2011 (D:A:D): a multicohort collaboration. Lancet [Internet]. 2014 [cited 2022 Jan 25];384(9939):241–8. Available from: https://pubmed.ncbi.nlm.nih.gov/25042234/.
Lieveld FI, Smit C, Richter C, van Erpecum KJ, Spanier BWM, Gisolf EH et al. Liver decompensation in HIV/Hepatitis B coinfection in the combination antiretroviral therapy era does not seem increased compared to hepatitis B mono-infection. Liver Int [Internet]. 2019 Mar 1 [cited 2022 Jan 25];39(3):470–83. Available from: https://pubmed.ncbi.nlm.nih.gov/30411848/.
Cainelli F, Vento S. Liver disease in patients with HIV in sub-Saharan Africa. Lancet HIV [Internet]. 2015 Oct 1 [cited 2022 Jan 21];2(10):e412–3. Available from: http://www.thelancet.com/article/S2352301815001794/fulltext.
Schutz C, Ismail Z, Proxenos CJ, Marais S, Burton R, Kenyon C et al. Burden of antituberculosis and antiretroviral drug-induced liver injury at a secondary hospital in South Africa. S Afr Med J [Internet]. 2012 [cited 2022 Jan 25];102(6):506–11. Available from: https://pubmed.ncbi.nlm.nih.gov/22668951/.
Feld JJ, Ocama P, Ronald A. The liver in HIV in Africa. Antivir Ther [Internet]. 2005 [cited 2022 Jan 21];10(8):953–65. Available from: https://pubmed.ncbi.nlm.nih.gov/16430201/.
Stabinski L, O’Connor S, Barnhart M, Kahn RJ, Hamm TE. Prevalence of HIV and hepatitis B virus co-infection in sub-Saharan Africa and the potential impact and program feasibility of hepatitis B surface antigen screening in resource-limited settings. J Acquir Immune Defic Syndr [Internet]. 2015 Apr 15 [cited 2022 Jan 25];68 Suppl 3:S274–85. Available from: https://pubmed.ncbi.nlm.nih.gov/25768867/.
Stabinski L, Reynolds SJ, Ocama P, Laeyendecker O, Ndyanabo A, Kiggundu V et al. High prevalence of liver fibrosis associated with HIV infection: a study in rural Rakai, Uganda. Antivir Ther [Internet]. 2011 [cited 2024 Jan 13];16(3):405–11. Available from: https://pubmed.ncbi.nlm.nih.gov/21555823/.
Jaquet A, Wandeler G, Nouaman M, Ekouevi DK, Tine J, Patassi A et al. Alcohol use, viral hepatitis and liver fibrosis among HIV-positive persons in West Africa: a cross-sectional study. J Int AIDS Soc [Internet]. 2017 Feb 17 [cited 2022 Jan 21];19(1). Available from: https://pubmed.ncbi.nlm.nih.gov/28362065/.
Tomeny EM, Nightingale R, Chinoko B, Nikolaidis GF, Madan JJ, Worrall E et al. TB morbidity estimates overlook the contribution of post-TB disability: evidence from urban Malawi. BMJ Glob Health [Internet]. 2022 May 3 [cited 2023 Oct 28];7(5). Available from: https://pubmed.ncbi.nlm.nih.gov/35606014/.
Mkoko P, Naidoo S, Mbanga LC, Nomvete F, Muloiwa R, Dlamini S. Chronic lung disease and a history of tuberculosis (post-tuberculosis lung disease): Clinical features and in-hospital outcomes in a resource-limited setting with a high HIV burden. S Afr Med J [Internet]. 2019 Mar 1 [cited 2023 Oct 28];109(3):169–73. Available from: https://pubmed.ncbi.nlm.nih.gov/30834873/.
Menzies NA, Quaife M, Allwood BW, Byrne AL, Coussens AK, Harries AD et al. Lifetime burden of disease due to incident tuberculosis: a global reappraisal including post-tuberculosis sequelae. Lancet Glob Health [Internet]. 2021 Dec 1 [cited 2023 Oct 28];9(12):e1679–87. Available from: https://pubmed.ncbi.nlm.nih.gov/34798027/.
Meghji J, Lesosky M, Joekes E, Banda P, Rylance J, Gordon S et al. Patient outcomes associated with post-tuberculosis lung damage in Malawi: a prospective cohort study. Thorax [Internet]. 2020 Mar 1 [cited 2023 Oct 28];75(3):269–78. Available from: https://pubmed.ncbi.nlm.nih.gov/32102951/.
Ddungu A, Semitala FC, Castelnuovo B, Sekaggya-Wiltshire C, Worodria W, Kirenga BJ. Chronic obstructive pulmonary disease prevalence and associated factors in an urban HIV clinic in a low income country. PLoS One [Internet]. 2021 Aug 1 [cited 2023 Oct 28];16(8). Available from: https://pubmed.ncbi.nlm.nih.gov/34388209/.
Drummond MB, Kunisaki KM, Huang L. Obstructive Lung Diseases in HIV: A Clinical Review and Identification of Key Future Research Needs. Semin Respir Crit Care Med [Internet]. 2016 Apr 1 [cited 2023 Oct 28];37(2):277–88. Available from: https://pubmed.ncbi.nlm.nih.gov/26974304/.
Kayongo A, Wosu AC, Naz T, Nassali F, Kalyesubula R, Kirenga B et al. Chronic obstructive pulmonary disease prevalence and associated factors in a setting of well-controlled HIV, a cross-sectional study. COPD [Internet]. 2020 May 3 [cited 2023 Oct 28];17(3):297. Available from: /pmc/articles/PMC8126339/.
Konstantinidis I, Crothers K, Kunisaki KM, Drummond MB, Benfield T, Zar HJ et al. HIV-associated lung disease. Nat Rev Dis Primers [Internet]. 2023 Dec 1 [cited 2023 Oct 28];9(1). Available from: https://pubmed.ncbi.nlm.nih.gov/37500684/.
Attia EF, Miller RF, Ferrand RA. Bronchiectasis and other chronic lung diseases in adolescents living with HIV. Curr Opin Infect Dis [Internet]. 2017 [cited 2023 Oct 28];30(1):21–30. Available from: https://pubmed.ncbi.nlm.nih.gov/27753690/.
Ibrahim AO, Aremu SK, Afolabi BA, Ajani GO, Kolawole FT, Oguntoye OA. Acute severe asthma and its predictors of mortality in rural Southwestern Nigeria: a-five year retrospective observational study. Chron Respir Dis [Internet]. 2023 Jan 1 [cited 2023 Oct 28];20. Available from: https://pubmed.ncbi.nlm.nih.gov/36652901/.
Kayongo A, Bartolomaeus TUP, Birkner T, Markó L, Löber U, Kigozi E et al. Sputum Microbiome and Chronic Obstructive Pulmonary Disease in a Rural Ugandan Cohort of Well-Controlled HIV Infection. Microbiol Spectr [Internet]. 2023 Apr 13 [cited 2023 Oct 28];11(2). Available from: /pmc/articles/PMC10100697/.
Chalmers JD, Goeminne P, Aliberti S, McDonnell MJ, Lonni S, Davidson J et al. The bronchiectasis severity index. An international derivation and validation study. Am J Respir Crit Care Med [Internet]. 2014 Mar 1 [cited 2023 Oct 28];189(5):576–85. Available from: https://pubmed.ncbi.nlm.nih.gov/24328736/.
Jones RC, Donaldson GC, Chavannes NH, Kida K, Dickson-Spillmann M, Harding S et al. Derivation and validation of a composite index of severity in chronic obstructive pulmonary disease: the DOSE Index. Am J Respir Crit Care Med [Internet]. 2009 Dec 15 [cited 2023 Oct 28];180(12):1189–95. Available from: https://pubmed.ncbi.nlm.nih.gov/19797160/.
Howlett WP. Neurological disorders in HIV in Africa: a review. Afr Health Sci [Internet]. 2019 [cited 2023 Oct 28];19(2):1953. Available from: /pmc/articles/PMC6794503/.
Mekuriaw B, Belayneh Z, Teshome W, Akalu Y. Prevalence and variability of HIV/AIDS-associated neurocognitive impairments in Africa: a systematic review and meta-analysis. BMC Public Health [Internet]. 2023 Dec 1 [cited 2023 Oct 28];23(1):1–16. Available from: https://bmcpublichealth.biomedcentral.com/articles/https://doi.org/10.1186/s12889-023-15935-x.
Elafros MA, Johnson BA, Siddiqi OK, Okulicz JF, Sikazwe I, Bositis CM et al. Mortality & recurrent seizure risk after new-onset seizure in HIV-positive Zambian adults. BMC Neurol [Internet]. 2018 Dec 7 [cited 2023 Oct 28];18(1). Available from: https://pubmed.ncbi.nlm.nih.gov/30522451/.
Lawler K, Mosepele M, Ratcliffe S, Seloilwe E, Steele K, Nthobatsang R et al. Neurocognitive impairment among HIV-positive individuals in Botswana: a pilot study. J Int AIDS Soc [Internet]. 2010 [cited 2023 Oct 28];13(1). Available from: https://pubmed.ncbi.nlm.nih.gov/20406460/.
Haas AD, Ruffieux Y, van den Heuvel LL, Lund C, Boulle A, Euvrard J et al. Excess mortality associated with mental illness in people living with HIV in Cape Town, South Africa: a cohort study using linked electronic health records. Lancet Glob Health [Internet]. 2020 Oct 1 [cited 2023 Oct 28];8(10):e1326–34. Available from: https://pubmed.ncbi.nlm.nih.gov/32971055/.
Ford N, Patten G, Rangaraj A, Davies MA, Meintjes G, Ellman T. Outcomes of people living with HIV after hospital discharge: a systematic review and meta-analysis. Lancet HIV [Internet]. 2022 Mar 1 [cited 2023 Oct 28];9(3):e150–9. Available from: https://pubmed.ncbi.nlm.nih.gov/35245507/.
Cox JA, Lukande RL, Nelson AM, Mayanja-Kizza H, Colebunders R, van Marck E, et al. An autopsy study describing causes of death and comparing clinico-pathological findings among hospitalized patients in Kampala, Uganda. PLoS ONE. 2012;7(3):e33685.
Namuju OC, Kwizera R, Lukande R, Pastick KA, Taylor JM, Nicol MR et al. Rates of refusal of clinical autopsies among HIV-positive decedents and an overview of autopsies in Uganda. Wellcome Open Res. 2022;6.
Cox JA, Lukande RL, Kateregga A, Mayanja-Kizza H, Manabe YC, Colebunders R. Autopsy acceptance rate and reasons for decline in Mulago Hospital, Kampala, Uganda. Trop Med Int Health. 2011;16(8):1015–8.
Turyamureba M, Yawe B, Oryema JB, Tanzania Journal of Health Research. 2023 [cited 2024 Jan 15]. Health Care Delivery System in Uganda: a review| Tanzania Journal of Health Research. Available from: https://www.ajol.info/index.php/thrb/article/view/231882.
Acknowledgements
Sincere appreciation is extended to the administration and staff of Kiruddu National Referral Hospital and Makerere University Joint AIDS Program for implementing the pilot HIV care program to improve the outcomes of hospitalized people living with HIV. Special appreciation and recognition are extended to Atine Edgar, Namugenyi Christabellah, Nabatanzi Cecilia, Kasirye Esther, Kakande Amina, Kabira Deborah, and Adong Florence among others in supporting the program.
Funding
The President’s Emergency Plan has supported this research for AIDS Relief (PEPFAR) through the Centre for Diseases Control and Prevention (CDC), under the terms of GH002022.
Author information
Authors and Affiliations
Contributions
DO, DSN, MM, CK and FCS conceptualized the project. DO, DSN and PA implemented the project and collected the data. DO & PA analysed the data. RK, SW, MM, SK, CK, NK and FCS supervised the implementation of the project and provided a critical review of the manuscript. All authors were major contributors to writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval was obtained from the Makerere University, College of Health Sciences, School of Public Health research ethics committee under Reference MakSPH-REC 710 and registered the study with the Uganda National Council for Science and Technology under reference HS553ES. The need for informed consent was waived by the Makerere University, College of Health Sciences, School of Public Health research ethics committee since routinely collected program data was used for analysis. Patient identifier information was anonymized to protect patient confidentiality.
Consent for publication
Not Applicable.
Competing interests
The authors DO, PA, DSN, RK, SW, MM, SK, NK, CK and FCS receive financial remuneration from CDC/PEPFAR as part of employee remuneration benefits. DO & CK have received remuneration benefits from the Government of Uganda. However, the findings and conclusions in this report are those of the authors and do not represent the official position of PEPFAR, CDC Uganda or the Government of Uganda.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Owachi, D., Akatukunda, P., Nanyanzi, D.S. et al. Mortality and associated factors among people living with HIV admitted at a tertiary-care hospital in Uganda: a cross-sectional study. BMC Infect Dis 24, 239 (2024). https://doi.org/10.1186/s12879-024-09112-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09112-7