Abstract
Background
The early identification of sepsis presenting a high risk of deterioration is a daily challenge to optimise patient pathway. This is all the most crucial in the prehospital setting to optimize triage and admission into the appropriate unit: emergency department (ED) or intensive care unit (ICU). We report the association between the prehospital National Early Warning Score 2 (NEWS-2) and in-hospital, 30 and 90-day mortality of SS patients cared for in the pre-hospital setting by a mobile ICU (MICU).
Methods
Septic shock (SS) patients cared for by a MICU between 2016, April 6th and 2021 December 31st were included in this retrospective cohort study. The NEWS-2 is based on 6 physiological variables (blood pressure, heart rate, respiratory rate, temperature, oxygen saturation prior oxygen supplementation, and level of consciousness) and ranges from 0 to 20. The Inverse Probability Treatment Weighting (IPTW) propensity method was applied to assess the association with in-hospital, 30 and 90-day mortality. A NEWS-2 ≥ 7 threshold was chosen for increased clinical deterioration risk definition and usefulness in clinical practice based on previous reports.
Results
Data from 530 SS patients requiring MICU intervention in the pre-hospital setting were analysed. The mean age was 69 ± 15 years and presumed origin of sepsis was pulmonary (43%), digestive (25%) or urinary (17%) infection. In-hospital mortality rate was 33%, 30 and 90-day mortality were respectively 31% and 35%. A prehospital NEWS-2 ≥ 7 is associated with an increase in-hospital, 30 and 90-day mortality with respective RRa = 2.34 [1.39–3.95], 2.08 [1.33–3.25] and 2.22 [1.38–3.59]. Calibration statistic values for in-hospital mortality, 30-day and 90-day mortality were 0.54; 0.55 and 0.53 respectively.
Conclusion
A prehospital NEWS-2 ≥ 7 is associated with an increase in in-hospital, 30 and 90-day mortality of septic shock patients cared for by a MICU in the prehospital setting. Prospective studies are needed to confirm the usefulness of NEWS-2 to improve the prehospital triage and orientation to the adequate facility of sepsis.
Similar content being viewed by others
Introduction
During the last twenty years, despite research on prevention and treatments, the mortality and the morbidity rates of sepsis remain stable [1, 2]. To date, whatever the initial stage of sepsis, this latter one is responsible of 20% of all deaths worldwide, approximately 11 million deaths ever year [3]. Sepsis is also a major cause of death among hospitalized patients, especially in intensive care unit (ICU) [4, 5] where mortality and morbidity rates are estimated of 37.3% and 10.4% [6].
On 2017 the World Health Assembly and the World Health Organization defined that prevention, diagnosis, and sepsis management are the main priorities to decrease morbidity and mortality [7]. It was underpinned that sepsis outcome depends on early identification and treatment implementation with hemodynamic optimization and antibiotic therapy (ABT) administration [8, 9] both included in a bundle of care [10].
In and, out-of-hospital sepsis diagnosis and severity evaluation are the bundle of care first steps aiming to determine the appropriate level of care. Because 70% of sepsis occurs outside a hospital environment, a special attention is needed to help physician for sepsis diagnosis and severity assessment to optimize triaging between ambulatory treatment, ward, emergency department (ED) or ICU admission [11]. Outside hospital setting, severity assessment is mainly based on clinical signs due to the absence of biomarker availability [12,13,14]. Different sepsis severity assessment scores have been developed, to enhance clinical diagnostic performance, despite to date no score was prospectively validated for pre-hospital use [15, 16].
In 2012, the Royal College of Physicians launched the National Early Warning Score (NEWS) to improve the outcomes of patients suffering from acute illness [17]. The NEWS score aims to triggering a rapid and effective clinical response, in time, person and place because the triad: early detection, timeliness of response and competency of the clinical response directly impact the outcome [18,19,20,21,22,23,24,25].
This study aims to describe the association between the prehospital National Early Warning Score 2 (NEWS-2) and in-hospital, 30 and 90-day mortality of SS patients cared for in the pre-hospital setting by a mobile ICU (MICU).
Methods
Population
As previously reported, in France, pre-hospital emergency system (PEMS) relies on the Service d’Aide Médicale d’Urgence (SAMU) [12, 13, 15, 26, 27]. Briefly, SAMU is composed of dispatch operators and emergency physicians [28] with a unique national phone number, the “15”. After a telephone discussion with the patient, or a relative, or a witness, the physician, based on patient’s medical history and reported symptoms, in case of life-threatening emergencies, may decide to dispatch a mobile intensive care unit (MICU) team to the scene. The MICU team, a driver, a nurse and an emergency physician, is equipped to face initial management of major organ failures [28].
All adults patients aged ≥ 18 years, cared for by a MICU from SAMU 75 Necker - Enfants Malades Hospital, SAMU 75 Lariboisière Hospital, SAMU 75 Pitié Salpêtrière Hospital, SAMU 75 Hôtel Dieu Hospital, Paris, Assistance Publique - Hôpitaux de Paris, Paris– France; Paris Fire Brigade Emergency Medical Service, Paris– France; SAMU 972 Fort de France University Hospital, La Martinique– France; SAMU 31 University Toulouse Hospital, Toulouse– France and SAMU 31 Castres Hospital, Castres– France, between 2016, April 6th, and 2021, December 31st, were included in this retrospective study based on 2012 sepsis-2 conference septic shock definition [29]. Eligible patients were identified using electronic research using septic shock or severe sepsis keywords. No exclusion criteria were used in this study.
Ethical considerations
The French Society of Anaesthesiology and Intensive Care ethics committee (Reference: IRB00010254-2017-026, 2017/12/12), the Ethics Committee for Behavioural and Health Research (CERCES Reference 2018-04, 2018/01/16) and the National Heart Agency (2017-A02335-48–2017/07/30) approved the trial protocol waiving patient consent for this retrospective study.
Data collection
A standardized data collection template was used in order to minimize data abstraction bias [30].
Patients’ demographic characteristics (age, weight, height, calculated body mass index (BMI) and gender), prehospital supposed origin of sepsis, initial prehospital vital signs values (systolic (SBP), diastolic (DBP) and mean blood (MBP) pressure, heart rate (HR), pulse oximetry (SpO2), respiratory rate (RR), body core temperature and Glasgow coma scale (GCS)), skin mottling score (SMS from 0 to 5), capillary refill time (CRT) (seconds), duration of prehospital care, prehospital treatments delivered (antibiotic therapy (ABT) type and dose, fluid volume expansion type and dose, catecholamine type and dose) were collected from MICU pre-hospital medical records. Comorbidities: hypertension, coronary heart disease (CHD), chronic cardiac failure (CCF), chronic renal failure (CRF), chronic obstructive pulmonary disease (COPD), diabetes mellitus and history of cancer, were also collected from pre and in-hospital medical reports. Length of stay in the ICU, length of stay in the hospital, 30 and 90-day mortality were retrieved from in-hospital medical records. In France, the hospital patient monitoring software enables to know the vital status even if the patient is no longer hospitalised. Thus, the vital status “alive” or “dead” on day-90 was available for each analysed patient.
Simplified acute physiology score (SAPS2) [31] was calculated 24 h after hospital admission.
Statistical analysis
A mean with standard deviation was used to express quantitative parameters with a gaussian distribution, median with interquartile range [Q1-Q3] for quantitative parameters with a non-normal distribution and absolute values and percentages for qualitative parameters.
The main outcomes were in-hospital, 30 and 90-day mortality of septic shock patients initially cared for by a MICU in the pre-hospital setting.
The NEWS-2 was calculated based on the sum of the worst value of the 6 following physiological variables: blood pressure, heart rate, respiratory rate, temperature, oxygen saturation prior oxygen supplementation, and level of consciousness according to the 2017 Royal College of Physicians.
guidelines [17]. The NEWS-2 ranges from 0 to 20.
A NEWS-2 ≥ 7 threshold was chosen for increased clinical deterioration risk definition and usefulness in clinical practice based on previous report [17].
The relationship between each covariate and in-hospital, 30-day and 90-day mortality rates were assessed by bivariate and multivariate analyses. The NEWS-2 was analysed, as a continuous variable and as a binary variable using a threshold of NEWS ≥ 7 because its association with increased clinical deterioration risk. Results are expressed by an Odd Ratio (OR) and adjusted Odd Ratio (aOR) with a 95% confidence interval [95 CI].
A log binomial regression weighted with the inverse probability of treatment (IPTW) propensity score method was computed taking into potential cofounders. The propensity score aims to decrease bias due to non-randomized treatment allocation [32]. Cofounders included in the IPTW propensity analysis were: age, cancer history, CRF, COPD, CHD, diabetes mellitus, CCF, SAPS2, prehospital ABT administration, prehospital fluid volume expansion and prehospital catecholamine infusion. The selection of variables included in the multivariable analysis was done a priori guided by previous knowledge of factors known to influence septic shock survival. Results were expressed as adjusted risk ratio (RR) [95 CI].
All tests were 2-sided with a statistically significant p-value considered as < 0 0.05.
All analyses were performed using R 3.4.2 (http://www.R-project.org; the R Foundation for Statistical Computing, Vienna, Austria).
Results
Population characteristics
Between 2021, April 6th, and 2021, December 31st, 530 patients requiring pre-hospital MICU intervention for septic shock were analysed. The missing data rate was lower than 1%; these data were deleted for the statistical analysis.
Of the 7 participating centres, 165 patients (31%) were included by the Paris Fire Brigade Emergency Medical Service, 104 patients (20%) by SAMU 31 Toulouse, 77 patients (15%) by SAMU 75 Necker, 71 patients (13%) by SAMU Castres, 51 patients (10%) by SAMU 972 La Martinique, 31 patients (6%) by SAMU 75 Lariboisière, 14 patients (3%) by SAMU 75 Hôtel Dieu and 17 patients (3%) by SAMU 75 Pitié Salpétrière.
The overall population mean age was 69 ± 15 years and 341 patients (64%) were male gender.
One hundred eighty (34%) patients died during hospital stay, 164 (31%) patients had died by day-30, and 184 (35%) had died by day-90.
Table 1 summarise the populations’ demographic and clinical characteristics (Table 1).
Presumed origin of septic shock was mainly pulmonary (43%), digestive (25%) or urinary (17%) (Table 2).
Prehospital setting
The mean duration of prehospital care was 71 ± 34 min, pre-hospital fluid expansion consisted on crystalloids (100%) with a mean volume of 932 ± 573 ml and 155 (29%) patients received norepinephrine infusion with a median dose of 1.0 [0.5–2.0] mg.h− 1.
Prehospital ABT was administered in 132 patients (25%) and no significant difference was observed between patients surviving or dying, at hospital, at 30 or 90 day (Table 1). The antibiotics were principally 3rd generation cephalosporins (n = 98, 75%).
Hospital stays
The median length of stay in the ICU was 4 [2–8] days and the median in-hospital length of stay was 10 [5–18] days.
The mean SAPS2 score was 60 ± 21 with significant difference between patients surviving or dying in hospital, at day-30 and day-90 (Table 1).
Prehospital NEWS-2
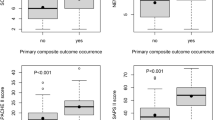
The mean overall prehospital NEWS-2 was 9 ± 3, with 406 patients (77%) patients having a prehospital NEWS-2 ≥ 7.
Bivariate logistic analysis revealed a significant association between prehospital NEWS (continuous variable) and in-hospital mortality (OR = 2.14 [1.19–3.83], p = 0.01), 28-day mortality (OR = 2.41 [1.33–4.36], p = 0.003) and 90-day mortality (OR = 1.88 [1.05–3.35], p = 0.03).
Using a threshold of a prehospital NEWS-2 ≥ 7, the association remains significant for in-hospital mortality (OR = 1.62 [1.04–2.58], p = 0.04), 28-day mortality (OR = 1.94 [1.22–3.18], p = 0.01) but not for 90-day mortality (OR = 1.43 [0.93–2.24], p = 0.11).
Propensity IPTW analyses
The log binomial regression weighted with the IPTW observed an association between a prehospital NEWS-2 ≥ 7 and in-hospital mortality: RRa = 2.34 [1.39–3.95], 30-day mortality: RR = 2.08 [1.33–3.25] and 90-day mortality: RRa = 2.22 [1.38–3.59].
Initial lactate was missing for 218 patients (41%) and initial skin mottling score missing for 220 patients (42%); both covariables were not included in the model.
The calibration statistic values were: 0.54; 0.55 and 0.53 respectively for in-hospital mortality, 30-day mortality and 90-day mortality.
Discussion
Here we report a positive association between in-hospital, 30 and 90-day mortality and (i) the prehospital NEWS-2, (ii) prehospital NEWS-2 ≥ 7 and among septic shock patients cared for in the pre-hospital setting by a mobile intensive care unit.
Previous reports underpinned that around one-third of potentially preventable deaths in the United Kingdom were related to poor clinical monitoring and/or inadequate response to clinical deterioration supporting that patients should be addressed to the most appropriate setting for clinical care [33], justifying NEWS-2 widespread deployment [17]. It is all the most true for sepsis for which diagnosis, severity assessment and treatment initiation does not suffer from any delay [14, 34, 35]. Beyond out- and in-hospital care aiming to improve sepsis outcome, early diagnosis and severity are cornerstones to decrease sepsis related mortality by initiation of the sepsis survival chain [36]. Early diagnosis is also recognised as an essential leverage arm to prevent potentially preventable deaths as it allows early initiation of treatment. Daily, PEMS are faced to a challenge aiming to, as quickly as possible, establish a right diagnosis and assess severity to adequately guide the patient towards the optimal care pathway for his or her disease. To establish a diagnosis and a clinical monitoring, simple and objective clinical tools usable at any time and reproduced by different caregivers are necessary. This is all the more important when diagnostic certainty is uncertain and/or urgent, even when combining both clinical and paraclinical, for example biological, variables, in the grey zone decision making [37]. Some clinical parameters, e.g., SMS, CRT [12, 13], are subjective and may be caught out in some situation, for example hypothermia.
Because of the lack of specificity of a single clinical sign [14], scoring system was developed to improve sensitivity and sensibility. For sepsis, the most known scores are which SOFA [38], Mortality in Emergency Department Sepsis (MEDS) [39], Predisposition, Infection, Response and Organ dysfunction (PIRO) [40] and q-SOFA since 2016 [14]. Although the latter does not require biological results and is recommended because of its simplicity outside ICU [41], q-SOFA validity remains under debate [13, 15, 16, 40, 42,43,44]. To date, in the prehospital setting, no score is validated, thus, sepsis severity assessment and prognostication still remain on clinical evaluation [45].
The score has several advantages, including: its ease of establishment since all the variables are accessible in the pre-hospital setting, its inter-observer reproducibility, and the possibility of being repeated over time in order to evaluate the treatment effect. However, one of the weakness is that NEWS-2 does not include age and major comorbidities, both reflecting frailty [46, 47] and associated with poor sepsis outcome [48,49,50].
Limitations
The current study suffers from limitations. Because of the retrospective study design, we cannot exclude that a potential selection bias affects the results validity. In addition, we are unable to conclude on a causal link between the NEWS-2 and mortality related to septic shock and sepsis. We cannot exclude unknown or missed confounders during the analysis. The NEWS-2 performance and external validation need to be confirmed by prospective studies, although the inclusion of centres of varying size and geography (a large city - Paris, one medium-sized city - Toulouse and one rural city– Castres) seems promising and represents a study strength. The study population was only adults; consequently, results extrapolation to sepsis and to paediatric population is not possible. We should keep in mind that some NEWS-2 variables may be influenced by patient previous medications, e.g., beta-blocker therapy, restricting their contribution to the NEWS-2.
Beyond all these limitations, the NEWS-2 seems to be an adequate tool for pre-hospital sepsis screening of a high risk of poor evolution and should be considered as an aid to clinical decision making, not a barrier or alternative to skilled clinical judgement.
Conclusion
Among sepsis patient requiring prehospital mobile intensive care unit intervention, a prehospital NEWS-2 ≥ 7 is associated with an increase in in-hospital, 30 and 90-day mortality. However, prospective studies are needed to confirm the usefulness of NEWS-2 to improve the prehospital triage, patient orientation to the optimal pathway and sepsis related mortality.
Data availability
The dataset analyzed during the current study are not publicly available because their containing information that could compromise the privacy of research participants but are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body mass index
- MICU:
-
Mobile intensive care unit
- aHR:
-
Adjusted hazard ratio
- ED:
-
Emergency department
- ICU:
-
Intensive care unit
- SAMU:
-
Urgent Medical Aid Service
- ABT:
-
Antibiotic therapy
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- MBP:
-
Mean blood pressure
- HR:
-
Heart rate
- SpO2:
-
Pulse oximetry
- RR:
-
Respiratory rate
- GCS:
-
Glasgow coma scale
- SMS:
-
Skin mottling score
- CRT:
-
Capillary refill time
- SOFA:
-
Sequential Organ Failure Assessment
- qSOFA:
-
Quick Sequential Organ Failure Assessment
- SAPS-2:
-
Simplified Acute Physiology Score
- PEMS:
-
Prehospital emergency medical service
- RRa:
-
Adjusted risk ratio
- ORa:
-
Adjusted odd ratio
- CHD:
-
Coronary heart disease
- CCF:
-
Chronic cardiac failure
- CRF:
-
Chronic renal failure
- COPD:
-
Chronic obstructive pulmonary disease
- IPTW:
-
Inverse Probability Treatment Weighting
- NEWS-2:
-
National Early Warning Score 2
References
Ferrer R, Artigas A, Levy MM, Blanco J, Gonzalez-Diaz G, Garnacho-Montero J, et al. Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain. JAMA. 2008;299(19):2294–303.
Nguyen HB, Van Ginkel C, Batech M, Banta J, Corbett SW. Comparison of predisposition, Insult/Infection, response, and organ dysfunction, Acute Physiology and Chronic Health evaluation II, and Mortality in Emergency Department Sepsis in patients meeting criteria for early goal-directed therapy and the severe sepsis resuscitation bundle. J Crit Care. 2012;27(4):362–9.
Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the global burden of Disease Study. Lancet. 2020;395(10219):200–11.
Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–54.
Weng L, Zeng XY, Yin P, Wang LJ, Wang CY, Jiang W, et al. Sepsis-related mortality in China: a descriptive analysis. Intensive Care Med. 2018;44(7):1071–80.
Vincent JL, Jones G, David S, Olariu E, Cadwell KK. Frequency and mortality of septic shock in Europe and North America: a systematic review and meta-analysis. Crit Care. 2019;23(1):196.
ASSEMBLY SWH. Improving the prevention, diagnosis and clinical management of sepsis. 2017.
Epstein L, Dantes R, Magill S, Fiore A. Varying estimates of Sepsis Mortality using death certificates and administrative codes–United States, 1999–2014. MMWR Morb Mortal Wkly Rep. 2016;65(13):342–5.
Medicine SoCC. Surviving sepsis campaign: updated bundles in response to new evidence. Mount Prospect, IL. Surviving Sepsis Campaign;. 2015(Apr).
Leisman DE, Doerfler ME, Ward MF, Masick KD, Wie BJ, Gribben JL, et al. Survival benefit and cost savings from compliance with a simplified 3-Hour Sepsis bundle in a series of prospective, multisite, observational cohorts. Crit Care Med. 2017;45(3):395–406.
Esteban A, Frutos-Vivar F, Ferguson ND, Penuelas O, Lorente JA, Gordo F, et al. Sepsis incidence and outcome: contrasting the intensive care unit with the hospital ward. Crit Care Med. 2007;35(5):1284–9.
Jouffroy R, Pierre Tourtier J, Gueye P, Bloch-Laine E, Bounes V, Debaty G et al. Prehospital shock index to assess 28-day mortality for septic shock. Am J Emerg Med. 2019.
Jouffroy R, Saade A, Tourtier JP, Gueye P, Bloch-Laine E, Ecollan P, et al. Skin mottling score and capillary refill time to assess mortality of septic shock since pre-hospital setting. Am J Emerg Med. 2019;37(4):664–71.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus definitions for Sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–10.
Jouffroy R, Saade A, Carpentier A, Ellouze S, Philippe P, Idialisoa R, et al. Triage of septic patients using qSOFA criteria at the SAMU Regulation: a retrospective analysis. Prehosp Emerg Care. 2018;22(1):84–90.
Jouffroy R, Saade A, Ellouze S, Carpentier A, Michaloux M, Carli P, et al. Prehospital triage of septic patients at the SAMU regulation: comparison of qSOFA, MRST, MEWS and PRESEP scores. Am J Emerg Med. 2018;36(5):820–4.
Physicians RCo. National Early Warning Score (NEWS) 2. Standardising the assessment of acute-illnessseverity in the NHS. 2017.
Smith GB, Prytherch DR, Jarvis S, Kovacs C, Meredith P, Schmidt PE, et al. A comparison of the ability of the Physiologic Components of Medical Emergency Team Criteria and the U.K. National Early warning score to discriminate patients at risk of a range of adverse clinical outcomes. Crit Care Med. 2016;44(12):2171–81.
Smith GB, Prytherch DR, Schmidt P, Featherstone PI, Knight D, Clements G, et al. Hospital-wide physiological surveillance-a new approach to the early identification and management of the sick patient. Resuscitation. 2006;71(1):19–28.
Albur M, Hamilton F, MacGowan AP. Early warning score: a dynamic marker of severity and prognosis in patients with Gram-negative bacteraemia and sepsis. Ann Clin Microbiol Antimicrob. 2016;15:23.
Gao H, McDonnell A, Harrison DA, Moore T, Adam S, Daly K, et al. Systematic review and evaluation of physiological track and trigger warning systems for identifying at-risk patients on the ward. Intensive Care Med. 2007;33(4):667–79.
Keep JW, Messmer AS, Sladden R, Burrell N, Pinate R, Tunnicliff M, et al. National early warning score at Emergency Department triage may allow earlier identification of patients with severe sepsis and septic shock: a retrospective observational study. Emerg Med J. 2016;33(1):37–41.
Silcock DJ, Corfield AR, Gowens PA, Rooney KD. Validation of the National Early warning score in the prehospital setting. Resuscitation. 2015;89:31–5.
Shaw J, Fothergill RT, Clark S, Moore F. Can the prehospital national early warning score identify patients most at risk from subsequent deterioration? Emerg Med J. 2017;34(8):533–7.
Badriyah T, Briggs JS, Meredith P, Jarvis SW, Schmidt PE, Featherstone PI, et al. Decision-tree early warning score (DTEWS) validates the design of the National Early warning score (NEWS). Resuscitation. 2014;85(3):418–23.
Jouffroy R, Saade A, Muret A, Philippe P, Michaloux M, Carli P, et al. Fluid resuscitation in pre-hospital management of septic shock. Am J Emerg Med. 2018;36(10):1754–8.
Jouffroy R, Gilbert B, Tourtier JP, Bloch-Laine E, Ecollan P, Boularan J, et al. Prehospital Bundle of Care based on antibiotic therapy and hemodynamic optimization is Associated with a 30-Day mortality decrease in patients with septic shock. Crit Care Med. 2022;50(10):1440–8.
Adnet F, Lapostolle F. International EMS systems: France. Resuscitation. 2004;63(1):7–9.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580–637.
Gearing RE, Mian IA, Barber J, Ickowicz A. A methodology for conducting retrospective chart review research in child and adolescent psychiatry. J Can Acad Child Adolesc Psychiatry. 2006;15(3):126–34.
Le Gall JR, Lemeshow S, Saulnier F. A new simplified Acute Physiology score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270(24):2957–63.
Robins JM, Hernan MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11(5):550–60.
Hogan H, Healey F, Neale G, Thomson R, Vincent C, Black N. Preventable deaths due to problems in care in English acute hospitals: a retrospective case record review study. BMJ Qual Saf. 2012;21(9):737–45.
Chen AX, Simpson SQ, Pallin DJ. Sepsis guidelines. N Engl J Med. 2019;380(14):1369–71.
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving Sepsis Campaign: International guidelines for Management of Sepsis and Septic Shock 2021. Crit Care Med. 2021;49(11):e1063–e143.
Jouffroy R, Gueye P. Intensive care unit versus high-dependency care unit admission on mortality in patients with septic shock: let’s think to the survival chain concept for septic shock. J Intensive Care. 2022;10(1):52.
Cannesson M, Le Manach Y, Hofer CK, Goarin JP, Lehot JJ, Vallet B, et al. Assessing the diagnostic accuracy of pulse pressure variations for the prediction of fluid responsiveness: a gray zone approach. Anesthesiology. 2011;115(2):231–41.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, et al. The SOFA (Sepsis-related Organ failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-related problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–10.
Shapiro NI, Wolfe RE, Moore RB, Smith E, Burdick E, Bates DW. Mortality in Emergency Department Sepsis (MEDS) score: a prospectively derived and validated clinical prediction rule. Crit Care Med. 2003;31(3):670–5.
Marshall JC. The PIRO (predisposition, insult, response, organ dysfunction) model: toward a staging system for acute illness. Virulence. 2014;5(1):27–35.
Freund Y, Lemachatti N, Krastinova E, Van Laer M, Claessens YE, Avondo A, et al. Prognostic accuracy of Sepsis-3 criteria for In-Hospital mortality among patients with suspected infection presenting to the Emergency Department. JAMA. 2017;317(3):301–8.
Vafaei A, Heydari K, Hashemi-Nazari SS, Izadi N, Hassan Zadeh H. PIRO, SOFA and MEDS scores in Predicting one-Month Mortality of Sepsis patients; a diagnostic accuracy study. Arch Acad Emerg Med. 2019;7(1):e59.
Askim A, Moser F, Gustad LT, Stene H, Gundersen M, Asvold BO, et al. Poor performance of quick-SOFA (qSOFA) score in predicting severe sepsis and mortality - a prospective study of patients admitted with infection to the emergency department. Scand J Trauma Resusc Emerg Med. 2017;25(1):56.
Finkelsztein EJ, Jones DS, Ma KC, Pabon MA, Delgado T, Nakahira K, et al. Comparison of qSOFA and SIRS for predicting adverse outcomes of patients with suspicion of sepsis outside the intensive care unit. Crit Care. 2017;21(1):73.
Guirgis FW, Jones L, Esma R, Weiss A, McCurdy K, Ferreira J, et al. Managing sepsis: electronic recognition, rapid response teams, and standardized care save lives. J Crit Care. 2017;40:296–302.
Diaconu K, Falconer J, Vidal N, O’May F, Azasi E, Elimian K, et al. Understanding fragility: implications for global health research and practice. Health Policy Plan. 2020;35(2):235–43.
Xue QL. The frailty syndrome: definition and natural history. Clin Geriatr Med. 2011;27(1):1–15.
Blot S, Cankurtaran M, Petrovic M, Vandijck D, Lizy C, Decruyenaere J, et al. Epidemiology and outcome of nosocomial bloodstream infection in elderly critically ill patients: a comparison between middle-aged, old, and very old patients. Crit Care Med. 2009;37(5):1634–41.
Martin GS, Mannino DM, Moss M. The effect of age on the development and outcome of adult sepsis. Crit Care Med. 2006;34(1):15–21.
Muscedere J, Waters B, Varambally A, Bagshaw SM, Boyd JG, Maslove D, et al. The impact of frailty on intensive care unit outcomes: a systematic review and meta-analysis. Intensive Care Med. 2017;43(8):1105–22.
Acknowledgements
None.
Funding
none.
Author information
Authors and Affiliations
Contributions
Conceptualization: RJ, PG. Methodology: RJ. Data curation: RJ, FN, JL, BG, ST, EBL, PE, VB, JB, BV, PG. Writing- Original draft preparation: RJ, FN, JL, BG, PG. Investigation: RJ, PG. Supervision: RJ, PG. Validation: RJ, PG. Writing- Reviewing and Editing: RJ, FN, JL, BG, ST, EBL, PE, VB, JB, BV, PG.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the French Society of Anaesthesia and Intensive Care ethics committee on December 12th, 2017 (Ref number: IRB 00010254-2017-026). The French Society of Anaesthesia and Intensive Care ethics committee waived the patient informed consent for participation in this retrospective study. All experiments were performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jouffroy, R., Négrello, F., Limery, J. et al. The prehospital NEW score to assess septic shock in-hospital, 30-day and 90-day mortality. BMC Infect Dis 24, 213 (2024). https://doi.org/10.1186/s12879-024-09104-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09104-7