Abstract
Background
BK polyomavirus (BKPyV) infection after kidney transplantation can lead to serious complications such as BKPyV-associated nephropathy (BKPyVAN) and graft loss. The aim of this study was to investigate the incidence of BKPyVAN after implementing a BKPyV screening program, to map the distribution of BKPyV genotypes and subtypes in the Uppsala-Örebro region and to identify host and viral risk factors for clinically significant events.
Methods
This single-center prospective cohort study included kidney transplant patients aged ≥ 18 years at the Uppsala University Hospital in Sweden between 2016 and 2018. BKPyV DNA was analyzed in plasma and urine every 3 months until 18 months after transplantation. Also genotype and subtype were determined. A logistic regression model was used to analyze selected risk factors including recipient sex and age, AB0 incompatibility and rejection treatment prior to BKPyVAN or high-level BKPyV DNAemia.
Results
In total, 205 patients were included. Of these, 151 (73.7%) followed the screening protocol with 6 plasma samples, while184 (89.8%) were sampled at least 5 times. Ten (4.9%) patients developed biopsy confirmed BKPyVAN and 33 (16.1%) patients met criteria for high-level BKPyV DNAemia. Male sex (OR 2.85, p = 0.025) and age (OR 1.03 per year, p = 0.020) were identified as significant risk factors for developing BKPyVAN or high-level BKPyV DNAemia. BKPyVAN was associated with increased viral load at 3 months post transplantation (82,000 vs. < 400 copies/mL; p = 0.0029) and with transient, high-level DNAemia (n = 7 (27%); p < 0.0001). The most common genotypes were subtype Ib2 (n = 50 (65.8%)) and IVc2 (n = 20 (26.3%)).
Conclusions
Male sex and increasing age are related to an increased risk of BKPyVAN or high-level BKPyV DNAemia. BKPyVAN is associated with transient, high-level DNAemia but no differences related to viral genotype were detected.
Similar content being viewed by others
Background
BK polyomavirus (BKPyV) often causes asymptomatic infection during childhood [1]. The seroprevalence has been examined in different populations using various approaches [2] and recent studies in healthy adults and recipients of organ transplants estimate a seroprevalence above 90% [3,4,5,6]. After primary infection, BKPyV persists mainly in the urothelium and renal tubular cells in the reno-urinary tract causing minimal clinical implications [7]. However, in immunocompromised hosts BKPyV may reactivate with detectable BKPyV DNA in urine and plasma and cause serious complications such as BKPyV-associated nephropathy (BKPyVAN) in 1–10% of kidney transplant recipients [1, 8,9,10,11]. Besides BKPyV DNAemia, several other risk factors have been identified, including male sex, older age, concurrent cytomegalovirus (CMV) infection, HLA mismatch, AB0 incompatibility, rejection treatment and deceased donor [12,13,14,15].
BKPyV is classified into four genotypes labelled I-IV [2, 16]. Genotype I is the most common variant (80%) and is prevalent worldwide. Genotype IV is less frequent (15%) and is mostly found in Europe and Asia, whereas genotypes II and III are rare [17, 18]. Based on variations in the BKPyV VP1 gene, four genotype I subtypes (Ia, Ib1, Ib2, and Ic) and six genotype IV subtypes (IVa1, IVa2, IVb1, IVb2, IVc1, and IVc2) have been identified [18, 19]. Subtype Ia is highly prevalent in Africa, Ib and Ic in Southeast and Northeast Asia respectively and Ib2 is highly prevalent in Europe [18, 20]. Subtypes belonging to genotype IV are predominantly observed in Asia, except for IVc2, which is more prevalent in Europe [19, 21]. Based on in vitro experiments, BKPyV genotype I replicates more efficiently than genotype IV in human renal epithelial cells in vitro [22] and therefore could be more capable to cause clinically relevant BKPyV infection. Some studies have shown that genotype IV is associated with higher DNAemia and BKPyVAN [23] while others have not been able to verify this observation [24] and a clear correlation between genotype and clinical outcome of BKPyV infection has not yet been established.
In a previous retrospective study of 928 renal transplants, we found that male sex was the only statistically significant predictor for BKPyVAN [25]. In 2015, a screening program for BKPyV was introduced at our center. In this study we evaluated the incidence of BKPyVAN after implementation of the program. We also investigated selected pre-transplant risk factors for BKPyVAN and levels of BKPyV DNAemia as well as post-transplant variables such as DNA levels and BKPyV genotypes that were only related to BKPyVAN.
Methods
Study design
This was a single-center prospective cohort study. The study included females and males aged ≥ 18 years who underwent kidney transplantation or simultaneous pancreas and kidney transplantation at the Uppsala University Hospital in Sweden from 12th of May 2016 until the 24th of September 2018 and signed the informed consent (inclusion criteria). Patients who did not understand sufficient Swedish, refused, had psychiatric problems or failed to follow-up were not able to participate (exclusion criteria). The study was approved by the Regional ethical review board in Uppsala (No. 2015/488). Data were collected from electronic health records and the local transplantation database at the Uppsala University Hospital.
Local BKPyV screening program
A screening program for BKPyV was implemented at our center during 2015 including analyses for BKPyV DNA in blood samples drawn approximately three months after transplantation and then approximately every third month until 18 months after transplantation. In addition, blood samples could also be taken for BKPyV DNA analysis in case of increased creatinine levels and/or suspected BKPyV infection. If BKPyV levels were elevated in plasma the patient was monitored with more frequent sampling. The study protocol included analysis of plasma samples close to all six time points (+/- 6 weeks). In addition to the mandatory study protocol, urine samples were taken up to 6 times, at the same time points as the plasma samples.
Diagnosis of BKPyV and BKPyVAN
BKPyV was analyzed in plasma and urine samples from the patients using a modified variant of a previously described quantitative TaqMan real time polymerase chain reaction (qPCR) procedure, where the primers and probe were designed to give representative detection of all major genotypes [26] (Supplementary Table 1). Briefly, BKPyV DNA was extracted from 200 µL plasma or urine using the automatic NucliSens easyMAG robot (BioMérieux, Marcy l’Etoile, France). BKPyV DNA was then amplified from 5 µl out of 60 µl elution volume using TaqMan Universal PCR Master Mix (Thermo Fisher, Stockholm, Sweden) and the Qiagen Rotor-Gene Q thermo cycler (Qiagen, Hilden, Germany). The assay has a linear range of 400 to 1 × 109 copies/mL and its proficiency was verified using external quality assessment programs from Instand and QCMD.
The locally applied indication for a transplant biopsy was, in general, an unexplained increase in serum creatinine of at least ten per cent. BKPyVAN was examined by pathological evaluation of kidney allograft biopsies taken at any time after transplantation and defined as positive immunohistochemical staining for Simian virus 40 large T antigen and a positive BKPyV DNAemia (≥400 copies/mL).
Determination of BKPyV genotype
BKPyV genotypes were determined by targeting the variable region of the VP1 gene using Sanger sequencing and gene analysis in MEGA X [27]. The sequences were aligned using Clustal W and a maximum-likelihood phylogenetic tree was constructed based on the Tamura-Nei substitution model using default parameters. Viral DNA from plasma and urine samples was amplified using a nested PCR covering nucleotides 1528–2270 (Dunlop numbering) of the BKPyV genome (Supplementary Table 1), in a Veriti 96 well thermal cycler (Applied Biosystems) by Taq PCR master mix (QIAGEN).
Immunosuppressive regimens
With few exceptions, patients received the local standard immunosuppressive regimen used during the study period; consisting of induction therapy with anti-IL-2 receptor antibodies (basiliximab) and methylprednisolone or methylprednisolone alone which was considered standard of care (SOC) in Uppsala at the time of the study. The maintenance immunosuppression consisted of daily tacrolimus and prednisolone in tapering doses. In addition, most patients received mycophenolate mofetil (MMF).
Enhanced induction was defined as treatment with thymoglobulin, rituximab and/or eculizumab, often in combination with IVIg (intravenous immunoglobulin) and immunoadsorption and/or plasmapheresis/apheresis. Enhanced induction was given on certain occasions such as HLA-incompatibility, AB0 incompatibility, simultaneous pancreas and kidney transplantation and other higher risk immunological scenarios such as previous transplantations. The standard of care induction for AB0 incompatibility was rituximab and glycosorb treatment or in some cases immunoadsorption and/or plasmapheresis. Rejection treatment included methylprednisolone, anti-thymocyte immunoglobulin, rituximab, eculizumab, IVIg and/or plasmapheresis.
The locally applied recommendation in case of BKPyV DNAemia detection with levels < 10,000 copies/mL was to increase follow-up to monthly plasma DNA analysis and make minor adjustments of the immunosuppressive treatment. If high-level DNAemia was detected, follow-up was increased and the MMF dose was reduced by 50%. If reduction of the MMF dose was inefficient MMF was discontinued. In most cases the tacrolimus dose was also reduced.
Statistical analysis
The primary analysis was the incidence of BKPyVAN after implementation of a screening program. The secondary analysis was on predictors for BKPyVAN or high-level BKPyV DNAemia. The preselected risk factors in the multivariable analysis were male sex, age, AB0 incompability and rejection treatment, which were selected on the basis of previous findings and biological rationale rather than univariate analysis, in line with the recommendations by Heinze et al. [28]. As an exploratory analysis, the impact of BKPyV genotypes and virologic course on clinical outcome was investigated.
Quantitatively determinable levels of BKPyV DNA were categorized into the following groups: (a) High-level BKPyV DNAemia defined as levels of BKPyV DNA ≥10,000 copies/mL, which is considered to be a clinically relevant level to develop BKPyVAN [29, 30]; (b) Low-level DNAemia 400 − 10,000 copies/mL; (c) Positive in urine only.
A logistic regression model, with Firth’s method to handle the sparsity in the data, was used for evaluating the primary endpoint in relation to the risk factors. Comparisons of subgroups were performed using Fisher’s exact test, with multiplicity correction using the false discovery rate (FDR) method or by multiple Mann-Whitney U tests with Holm-Sidak correction.
Kidney function was evaluated with a mixed-effects model.
Continuous data were presented as median with ranges. Statistical analyses were conducted in R version 3.5.1 using package survival version 2.42-3 or GraphPad Prism version 9.5.1. P-values below 0.05 were considered significant.
Results
Study subjects
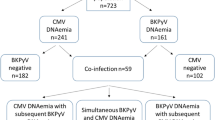
In total, 259 patients were planned for transplantation during the study period, whereof 248 were assessed for eligibility. Of these, 37 patients were excluded due to not being expected to understand the spoken and written information (n = 21), psychiatric reasons (n = 5), being minors (n = 3), declined to participate (n = 2) or other reasons (n = 6). Hence 211 patients were included in the study of which 6 patients were later excluded because they were lost to follow-up (n = 4) or because the transplantation was not performed (n = 2). For a summary of the clinical setup, see Fig. 1.
The final cohort of 205 patients was defined as the full analysis set (FAS) and included all transplanted patients with any number of plasma samples taken. Of these, 159 patients followed the study per protocol (PP) with six plasma samples taken approximately every third month until the end of the observation period or until they met the primary endpoint, lost their graft or died within 18 months (±2 months) from the transplantation. Whereas 151 (73.7%) of the FAS subjects followed the screening program as intended with 6 plasma samples, 5 plasma samples were drawn from 33 patients, resulting in 184 (89.8%) with at least 5 samples. Patient characteristics are presented in Table 1.
Immunosuppressive treatment
Induction therapy
In the FAS, a total of 200 patients (97.6%) received methylprednisolone and basiliximab as induction therapy. The remaining 5 patients (2.4%) received methylprednisolone alone. Also, 31 patients received enhanced induction, mostly in addition to SOC. Of these, 21 were AB0 incompatible.
Maintenance therapy
Calcineurin inhibitor (tacrolimus) were given as maintenance immunosuppression to 202 out of all 205 patients (98.5%) while belatacept was given to 3 patients (1.5%). In addition, 202 patients (98.5%) received MMF. All patients (100%) received prednisolone in tapering doses.
BKPyVAN and BKPyV DNAemia
In total, 10 patients developed biopsy confirmed BKPyVAN resulting in an incidence of 4.9%. Median time to BKPyVAN was 2.7 months (1.6–14.9 months). All but one (90.0%) were diagnosed within one year of transplantation. Thirty-three out of 205 (16.1%) patients met criteria for high-level BKPyV DNAemia, including 8 of the patients with BKPyVAN. Nineteen patients were positive in plasma, but at a low level, and 28 patients were positive only in urine (Table 2).
In four of the patients with high-level BKPyV DNAemia a biopsy was performed but BKPyVAN diagnostics was negative. In the remaining patients, renal function improved after reduction of immunosuppressants before a biopsy was considered necessary. Altogether, 35 (17.1%) developed BKPyVAN or high-level BKPyV DNAemia. The median time until diagnosis was 3.1 months (1.6–17.7) and 31 patients (88.6%) were diagnosed within one year of transplantation. Serum creatinine levels were significantly higher in the BKPyVAN or high level BKPyV DNAemia group, already from start of follow-up (Fig. 2).
Risk factors for BKPyVAN or high-level BKPyV DNAemia
In the multivariable logistic regression model for the FAS, male sex was identified as a significant risk factor for developing BKPyVAN or high-level BKPyV DNAemia (OR 2.85, p = 0.025) along with age (OR 1.03 per year, p = 0.020). However, when limiting the analysis to the PP subset, only male sex remained statistically significant. Neither AB0 incompatibility nor rejection treatment was recognized as statistically significant risk factors for development of BKPyVAN or high-level of BKPyV DNA in plasma (Table 3).
Genotypes
Samples from 76 of the 80 patients that were DNA positive in plasma and/or urine were successfully genotyped. Of these, the most common subtypes were Ib2 and IVc2, in 65.8% and 26.3% patients respectively. Other subtypes identified included Ia (1.3%), Ib1 (3.9%) and 1c (2.6%). Restricting the analysis to patients who were positive in plasma yielded a similar result, with 74.0% genotype I samples and 26.0% genotype IV samples in the FAS. Twenty-eight patients tested positive solely in urine, of whom 26 could be genotyped. Of these, the majority belonged to subtype Ib2 (69.2%) or IVc2 (26.9%). The genotypes and subtypes are presented in Table 4.
The data available do not indicate any substantial differences in subtype distribution in relation to BKPyVAN diagnosis or viral load.
Virological course and outcome of BKPyVAN
All ten subjects with BKPyVAN tested positive for BKPyV DNA in their plasma and there was an overall difference in virologic course between BKPyVAN and non-BKPyVAN subjects (p < 0.001). The correlation of the virological course and BKPyVAN diagnosis was explored by several approaches. First, we compared the incidence of BKPyVAN with non-BKPyVAN using the six pre-specified screening points taken every three months following transplantation. Whereas BKPyV DNA was significantly higher three months post transplantation in both the FAS and PP cohorts, no such correlation was found at any of the following screening points (Fig. 3A-B). To further examine the viral kinetics, the BKPyV-positive patients with high-level DNAemia, in the FAS cohort, were classified based on whether this condition lasted for more than three months or not (Fig. 3C-E). Whereas some cases of BKPyVAN were found in the categories of persistent high-level DNAemia (1/7 patients) and low-level DNAemia (2/19 patients), the majority of BKPyVAN cases were found in the category of transient high-level DNAemia (7/26 patients; Table 5). No cases of BKPyVAN were found in BKPyV negative patients or with BKPyV DNA in urine only. Analysis of the maximum levels of BKPyV DNA also showed that peak DNAemia occurred considerably earlier for patients with transient high DNAemia and BKPyVAN (Fig. 3F).
BKPyV DNA levels in plasma for viremic patients. A. BKPyV DNA levels at six prescheduled time points in the FAS cohort, where non-BKPyVAN (n = 42, blue) and BKPyVAN (n = 10, red) are indicated. B. BKPyV DNA levels at six prescheduled time points in the PP cohort, where non-BKPyVAN (n = 34, blue) and BKPyVAN (n = 10, red) are indicated. C. Virological course of seven patients with high-level of BKPyV DNAemia for > 3 months. D. Virological course of 26 patients with high-level of BKPyV DNAemia for < 3 months. E. Virological course of 19 patients with low-level of BKPyV DNAemia. F. Time when peak BKPyV DNAemia occurred for the virological courses and endpoint diagnosis. Abbreviations: High-level DNAemia (HL), Lowest Level of Quantitative Determination (LLQD) and Limit of Detection (LoD) are indicated by dotted lines, whereas median values are indicated by black lines. Statistical significance was determined by multiple Mann-Whitney U tests with Holm-Sidak correction and is indicated on top when observed
A comparison of each category against all the others combined revealed a significant difference for transient, high-level DNAemia and BKPyV negative patients (p < 0.0001, Table 5). No significant difference was seen for the groups persistent, high-level DNAemia, low-level DNAemia or patients positive only in urine.
Differences in virological course in relation to BKPyVAN diagnosis was investigated further by pair-wise comparison of the sub-groups (Table 6).
Transient DNAemia was statistically associated with BKPyVAN compared to both DNA negative patients and patients with DNA in urine only.
Discussion
The incidence of BKPyVAN in this study was 4.9%, of which 4.4% presented within 12 months, which is in line with other studies where BKPyV screening has been applied [31, 32]. In comparison, the 12-month cumulative incidence in a previous retrospective study, from the time before the introduction of screening, at our center was 3.7% [25]. The apparently limited effect of the screening program might be due to previous under-diagnosis of BKPyVAN and delayed diagnosis of BKPyV-related adverse outcomes after transplantation. In the analysis of risk factors, male sex and older age were significantly associated with our composite endpoint of BKPyVAN and/or high level BKPyV DNAemia, but not AB0 incompability or rejection treatment. Male sex has previously been shown to be a risk factor for BKPyV DNAemia and BKPyVAN [12, 25, 33,34,35]. Although the mechanism for this effect is not known, several explanations have been suggested, including anatomical, pharmacokinetical/pharmacodynamical and genetic factors [25].
The distribution of genotypes with 73.7% of genotype I and 26.3% of genotype IV is consistent with what would be expected in a European setting, with a slightly higher proportion of genotype IV in the northern and eastern parts of Europe [20]. Our findings are in line with previous work by Wunderink et al. who did not find any association between BKPyV genotype and risk of BKPyV DNAemia or BKPyVAN [24]. In contrast to earlier studies [23, 36] analysis of BKPyV genotypes did not give any significant association with clinically relevant BKPyV infection in our study. Since earlier PCR-detection methods for BKPyV DNA directed against genotype I have been found to selectively underestimate the levels of genotype IV DNA [26, 37] the clinical interpretation of earlier findings might have been skewed against this genotype at lower loads of viral DNA and thus overestimate its pathogenicity in case of high DNAemia [38].
Analysis of the viral kinetics via time-dependent analysis revealed that BKPyVAN was associated with an early and transient DNAemia characterized by high-levels already at the earliest time point. Although the point estimate indicated a potential overrepresentation also of persistent DNAemia in the BKPyVAN group, hypothesis testing in this small sub-group of patients failed to show statistical significance. During the 18-month follow-up period, only one patient with sustained levels of high DNAemia developed BKPyVAN (Fig. 3C), this patient had impaired humoral immunity and low B cell counts. At the time we began our screening program of renal transplant recipients, the recommended interval for BKPyV surveillance was plasma sampling every 3 months after transplantation [39]. However, according to the present guidelines from the American Society of Transplantation (AST) all KT recipients should be screened for BKPyV DNAemia monthly until month 9, and then every 3 months until 2 years after transplantation [14]. It is therefore advisable to start screening earlier and current guidelines have been adapted accordingly. Alternatively, the threshold for the risk of developing clinically relevant BKPyV reactivation, 10,000 copies/mL in plasma, might be too high. In line with this, Hassan S et al. have previously demonstrated that a threshold of ≥10,000 copies/mL underestimates BKPyVAN cases [40]. Due to similar observations, as well as the fact that 10–30% of biopsies are false negative, AST has revised its current recommendations, and now advocates diagnosing probable or presumptive BKPyVAN entirely on DNAemia, with probable BKPyVAN at levels less than 10,000 copies/mL if they persist for more than 3 weeks [14]. Given the recent development of an international standard for quantitative detection of BKPyVAN DNA [41], future harmonization of the quantification techniques should contribute to further improvement of clinical intervention cut-off criteria.
The time-dependent association between BKPyV DNA levels, level and type of immunosuppression and risk of BKPyVAN remains to be fully entangled. Given that interventions are often initiated already at an early stage of plasma BKPyV reactivation, the onward DNA level dynamics could be biased in relation to the clinical outcome in a purely observational setting that might cause the apparent paradox in our dataset where patients with BKPyVAN diagnosis present with lower BKPyV DNA levels during the following months. Alternatively, since activation of cell mediated immunity is not only essential for controlling viral replication but also induces virus-induced pathology by direct and by-stander killing, it cannot be excluded that vigorous activation of cytotoxic T cells (CTL) upon withdrawal of immune suppressants also contributes to increased damage of the kidneys. To further elucidate this question, a randomized trial comparing different DNA level cut-offs for intervention using standardized PCR assay together with predefined time-points for biopsies and CTL responses would be highly informative.
The strength of our study is the prospective study design with frequent sampling at pre-selected time points that allows proper categorization based on viral kinetics and an unbiased collection of a representative data set. Limitations include a lack of BKPyV data at early time points less than three months post transplantation and the fact that the study was conducted in only one center with a relatively small sample size.
Conclusions
We found that male sex and increasing age, but not AB0 incompability and rejection treatment, are significant risk factors for developing BKPyVAN or BKPyV DNAemia. BKPyVAN is associated with increased viral load shortly after transplantation and with transient, high-level DNAemia but not with genotype. The introduction of a BKPyV screening program has not reduced the incidence but is likely to detect more cases and at earlier time points, which can hopefully reduce the risk of permanent allograft failure or even graft loss.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BKPyV:
-
BK Polyomavirus
- BKPyVAN:
-
BK Polyomavirus–associated nephropathy
- CTL:
-
Cytotoxic T cells
- FAS:
-
Full analysis set
- FDR:
-
False discovery rate
- IVIg:
-
Intravenous immunoglobulin
- MMF:
-
Mycophenolate mofetil
- PCR:
-
Polymerase chain reaction
- PP:
-
Per protocol
- SOC:
-
Standard of care
References
Hirsch HH, Steiger J, Polyomavirus BK. Lancet Infect Dis. 2003;3(10):611–23.
Knowles WA. Discovery and epidemiology of the human polyomaviruses BK virus (BKV) and JC virus (JCV). Adv Exp Med Biol. 2006;577:19–45.
Kean JM, Rao S, Wang M, Garcea RL. Seroepidemiology of human polyomaviruses. PLoS Pathog. 2009;5(3):e1000363.
Antonsson A, Green AC, Mallitt KA, O’Rourke PK, Pawlita M, Waterboer T, Neale RE. Prevalence and stability of antibodies to the BK and JC polyomaviruses: a long-term longitudinal study of australians. J Gen Virol. 2010;91(Pt 7):1849–53.
Antonsson A, Pawlita M, Feltkamp MC, Bouwes Bavinck JN, Euvrard S, Harwood CA, et al. Longitudinal study of seroprevalence and serostability of the human polyomaviruses JCV and BKV in organ transplant recipients. J Med Virol. 2013;85(2):327–35.
Laine HK, Waterboer T, Syrjänen K, Grenman S, Louvanto K, Syrjänen S. Seroprevalence of polyomaviruses BK and JC in Finnish women and their spouses followed-up for three years. Sci Rep. 2023;13(1):879.
Chesters PM, Heritage J, McCance DJ. Persistence of DNA sequences of BK virus and JC virus in normal human tissues and in diseased tissues. J Infect Dis. 1983;147(4):676–84.
Rinaldo CH, Tylden GD, Sharma BN. The human polyomavirus BK (BKPyV): virological background and clinical implications. Apmis. 2013;121(8):728–45.
Binet I, Nickeleit V, Hirsch HH, Prince O, Dalquen P, Gudat F, et al. Polyomavirus disease under new immunosuppressive drugs: a cause of renal graft dysfunction and graft loss. Transplantation. 1999;67(6):918–22.
Hirsch HH, Knowles W, Dickenmann M, Passweg J, Klimkait T, Mihatsch MJ, Steiger J. Prospective study of polyomavirus type BK replication and nephropathy in renal-transplant recipients. N Engl J Med. 2002;347(7):488–96.
Ramos E, Drachenberg CB, Portocarrero M, Wali R, Klassen DK, Fink JC et al. BK virus nephropathy diagnosis and treatment: experience at the University of Maryland Renal Transplant Program. Clin Transpl. 2002:143– 53.
Schold JD, Rehman S, Kayle LK, Magliocca J, Srinivas TR, Meier-Kriesche HU. Treatment for BK virus: incidence, risk factors and outcomes for kidney transplant recipients in the United States. Transpl International: Official J Eur Soc Organ Transplantation. 2009;22(6):626–34.
Sharif A, Alachkar N, Bagnasco S, Geetha D, Gupta G, Womer K, et al. Incidence and outcomes of BK virus allograft nephropathy among ABO- and HLA-incompatible kidney transplant recipients. Clin J Am Soc Nephrol. 2012;7(8):1320–7.
Hirsch HH, Randhawa PS. BK Polyomavirus in solid organ transplantation-guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019;33(9):e13528.
Herrera S, Bernal-Maurandi J, Cofan F, Ventura P, Marcos MA, Linares L et al. BK Virus and Cytomegalovirus coinfections in kidney transplantation and their impact on allograft loss. J Clin Med. 2021;10(17).
Knowles WA, Gibson PE, Gardner SD. Serological typing scheme for BK-like isolates of human polyomavirus. J Med Virol. 1989;28(2):118–23.
Krumbholz A, Bininda-Emonds OR, Wutzler P, Zell R. Evolution of four BK virus subtypes. Infect Genet Evol. 2008;8(5):632–43.
Morel V, Martin E, François C, Helle F, Faucher J, Mourez T, et al. A simple and Reliable Strategy for BK Virus Subtyping and Subgrouping. J Clin Microbiol. 2017;55(4):1177–85.
Nishimoto Y, Zheng HY, Zhong S, Ikegaya H, Chen Q, Sugimoto C, et al. An Asian origin for subtype IV BK virus based on phylogenetic analysis. J Mol Evol. 2007;65(1):103–11.
Zheng HY, Nishimoto Y, Chen Q, Hasegawa M, Zhong S, Ikegaya H, et al. Relationships between BK virus lineages and human populations. Microbes Infect. 2007;9(2):204–13.
Ikegaya H, Saukko PJ, Tertti R, Metsärinne KP, Carr MJ, Crowley B, et al. Identification of a genomic subgroup of BK Polyomavirus spread in European populations. J Gen Virol. 2006;87(Pt 11):3201–8.
Nukuzuma S, Takasaka T, Zheng HY, Zhong S, Chen Q, Kitamura T, Yogo Y. Subtype I BK polyomavirus strains grow more efficiently in human renal epithelial cells than subtype IV strains. J Gen Virol. 2006;87(Pt 7):1893–901.
Schwarz A, Linnenweber-Held S, Heim A, Framke T, Haller H, Schmitt C. Viral origin, clinical course, and renal outcomes in patients with BK Virus infection after living-donor renal transplantation. Transplantation. 2016;100(4):844–53.
Wunderink HF, De Brouwer CS, Gard L, De Fijter JW, Kroes ACM, Rotmans JI, Feltkamp MCW. Source and relevance of the BK Polyomavirus genotype for infection after kidney transplantation. Open Forum Infect Dis. 2019;6(3):ofz078.
Lorant C, Westman G, Bergqvist A, von Zur-Mühlen B, Eriksson BM. Risk factors for developing BK Virus-Associated Nephropathy: a single-center retrospective cohort study of kidney transplant recipients. Ann Transpl. 2022;27:e934738.
Hoffman NG, Cook L, Atienza EE, Limaye AP, Jerome KR. Marked variability of BK virus load measurement using quantitative real-time PCR among commonly used assays. J Clin Microbiol. 2008;46(8):2671–80.
Kumar S, Stecher G, Li M, Knyaz C, Tamura K. MEGA X: Molecular Evolutionary Genetics Analysis across Computing platforms. Mol Biol Evol. 2018;35(6):1547–9.
Heinze G, Dunkler D. Five myths about variable selection. Transpl International: Official J Eur Soc Organ Transplantation. 2017;30(1):6–10.
Chung BH, Hong YA, Kim HG, Sun IO, Choi SR, Park HS, et al. Clinical usefulness of BK virus plasma quantitative PCR to prevent BK virus associated nephropathy. Transpl International: Official J Eur Soc Organ Transplantation. 2012;25(6):687–95.
Hirsch HH, Randhawa P. BK virus in solid organ transplant recipients. Am J Transplantation: Official J Am Soc Transplantation Am Soc Transpl Surg. 2009;9(Suppl 4):S136–46.
Theodoropoulos N, Wang E, Penugonda S, Ladner DP, Stosor V, Leventhal J, et al. BK virus replication and nephropathy after alemtuzumab-induced kidney transplantation. Am J Transplantation: Official J Am Soc Transplantation Am Soc Transpl Surg. 2013;13(1):197–206.
Smith JM, Dharnidharka VR, Talley L, Martz K, McDonald RA. BK virus nephropathy in pediatric renal transplant recipients: an analysis of the North American Pediatric renal trials and collaborative studies (NAPRTCS) registry. Clin J Am Soc Nephrol. 2007;2(5):1037–42.
Demey B, Tinez C, Francois C, Helle F, Choukroun G, Duverlie G, et al. Risk factors for BK virus viremia and nephropathy after kidney transplantation: a systematic review. J Clin Virol. 2018;109:6–12.
Masutani K, Ninomiya T, Randhawa P. HLA-A2, HLA-B44 and HLA-DR15 are associated with lower risk of BK Viremia. Nephrol Dial Transpl. 2013;28(12):3119–26.
Hirsch HH, Vincenti F, Friman S, Tuncer M, Citterio F, Wiecek A, et al. Polyomavirus BK replication in de novo kidney transplant patients receiving tacrolimus or cyclosporine: a prospective, randomized, multicenter study. Am J Transplantation: Official J Am Soc Transplantation Am Soc Transpl Surg. 2013;13(1):136–45.
Matsuda Y, Qazi Y, Iwaki Y. A rapid and efficient method BK Polyomavirus genotyping by high-resolution melting analysis. J Med Virol. 2011;83(12):2128–34.
Randhawa P, Kant J, Shapiro R, Tan H, Basu A, Luo C. Impact of genomic sequence variability on quantitative PCR assays for diagnosis of polyomavirus BK infection. J Clin Microbiol. 2011;49(12):4072–6.
Kant S, Dasgupta A, Bagnasco S, Brennan DC. BK Virus Nephropathy in kidney transplantation: a state-of-the-art review. Viruses. 2022;14(8).
Hirsch HH, Randhawa P. BK Polyomavirus in solid organ transplantation. Am J Transplantation: Official J Am Soc Transplantation Am Soc Transpl Surg. 2013;13(Suppl 4):179–88.
Hassan S, Mittal C, Amer S, Khalid F, Patel A, Delbusto R, et al. Currently recommended BK virus (BKV) plasma viral load cutoff of ≥ 4 log10/mL underestimates the diagnosis of BKV-associated nephropathy: a single transplant center experience. Transpl Infect Dis. 2014;16(1):55–60.
Govind S, Hockley J, Morris C, Almond N. The development and establishment of the 1st WHO BKV International Standard for nucleic acid based techniques. Biologicals. 2019;60:75–84.
Acknowledgements
The authors would like to thank Åsa Aringskog for administrative handling of the local transplantation follow-up database at the Uppsala University Hospital. The authors would also like to thank Mia Elofsson, Anna Högvall, Maria Svenaeus Lundgren, Carolina Leopoldson, Malin Dackborn for assistance with patient inclusion. The authors would like to thank Johan Lindbäck for discussion about the statistical analyses. Finally, the authors would like to thank Mahesh Anagandula for technical assistance with the experimental work as well as nurses and doctors in the region who have participated in the follow-up of the patients.
Funding
This work was supported by grants from the Regional Research Council Mid Sweden (RFR-560871, RFR-651591 and RFR-740101), The Swedish Kidney Foundation (F2020-0030, F2022-0087) and Targeted R&D funds from Region Uppsala.
Open access funding provided by Uppsala University.
Author information
Authors and Affiliations
Contributions
CL: conceptualization, methodology, validation, formal analysis, investigation, resources, writing– original draft preparation, visualization, supervision, project administration and funding acquisition. JZ: validation, formal analysis, investigation and visualization. NA: validation and investigation. UB, MT and BvZM: resources. BME: conceptualization, methodology, supervision, project administration and funding acquisition. AB: methodology, validation, formal analysis, resources, writing– original draft preparation, visualization and funding acquisition. GW: conceptualization, formal analysis and writing– original draft preparation. AB and GW contributed equally and should both be considered senior authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study included females and males aged ≥ 18 years who underwent kidney transplantation or simultaneous pancreas and kidney transplantation at the Uppsala University Hospital in Sweden from 12th of May 2016 until the 24th of September 2018 and signed the informed consent (inclusion criteria). The study was approved by the Regional ethical review board in Uppsala (No. 2015/488).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lorant, C., Zigmantaviciute, J., Ali, N. et al. The risk factors associated with post-transplantation BKPyV nephropathy and BKPyV DNAemia: a prospective study in kidney transplant recipients. BMC Infect Dis 24, 245 (2024). https://doi.org/10.1186/s12879-024-09093-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09093-7