Abstract
Background
So far, there have been more than 761 million confirmed cases of SARS-CoV-2 worldwide, with more than 6.8 million deaths. The most common direct causes of death for COVID-19 are diffuse alveolar injury and acute respiratory distress syndrome. Autopsy results have shown that 80-100% of COVID-19 patients have microthrombi which is 9 times higher than in patients with influenza. There are reported cases of fat embolism associated with Covid-19, but relevant epidemiological investigations and fatal cases of pulmonary fat embolism are lacking. In this report, we describe the first COVID-19 patient to die from pulmonary fat embolism.
Case presentation
A 54-year-old woman suddenly felt unwell while at work. She had difficulty breathing for 40 min and lost consciousness for 20 min before being taken to the hospital. On admission, her temperature was 36 ℃, but her respiration, heart rate, and blood pressure were undetectable. Laboratory examination revealed C-reactive protein, 26.55 mg/L; D-dimer, 11,400 µg/L; and procalcitonin, 0.21 ng/mL. She was declared clinically dead 2 h after admission due to ineffective rescue efforts. At autopsy, both lungs were highly oedematous with partial alveolar haemorrhage. The presence of microthrombi and pulmonary fat embolism in small interstitial pulmonary vessels was confirmed by phosphotungstic acid haematoxylin staining and oil red O staining. The immunohistochemical results of spike protein and nucleocapsid protein in laryngeal epithelial cells confirmed SARS-CoV-2 infection.
Conclusions
Pulmonary fat embolism may be another fatal complication of COVID-19 infection, and clinicians should pay more attention to it.
Similar content being viewed by others
Introduction
SARS-CoV-2 has rapidly spread around the world since it was first reported in December 2019. As of March 26, 2023, the World Health Organization reported more than 761 million confirmed cases and more than 6.8 million deaths [1]. Von Stillfried et al. [2]. reported 986 autopsy cases in a German multicentre study related to SARS-CoV-2 deaths, in which SARS-CoV-2 was the underlying cause of death in 86.2% of the cases. The most common direct causes of death are diffuse alveolar damage and acute respiratory distress syndrome. Only 4.0% of the deaths were due to pulmonary embolism. While fatal PFE was not mentioned in the study. Here, we report the first case of both fatal pulmonary microthromboembolism and PFE after infection with SARS-CoV-2. To our knowledge, there have been no reports of SARS-CoV-2-induced fatal PFE.
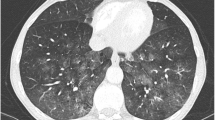
a: Diffuse pulmonary oedema, pulmonary haemorrhage and vacuole structure. (HE staining, arrows). b: Grade III fatal fat embolism in pulmonary interstitial small vessels. (ORO staining). c and d: Extensive microthrombus in pulmonary interstitial small vessels. (PTAH staining, arrows). e and f: Immunohistochemistry staining of S protein (E) and N protein (F)
Case report
A 54-year-old woman suddenly felt unwell while at work. She had difficulty breathing for 40 min and lost consciousness for 20 min before being taken to the hospital. On admission, her temperature was 36 ℃, but her respiration, heart rate, and blood pressure were undetectable. She was pale orally and had cold limbs. Her bilateral pupils were dilated, fixed and were approximately 5 mm in diameter, and her light reflexes had disappeared. She lost carotid pulsation and was in asystole. Doctors immediately performed ardiopulmonary resuscitation, tracheal intubation, establishment of venous channels, heart strengthening and other rescue measures. Laboratory examination: CRP, 26.55 mg/L; D-dimer, 11,400 µg/L; PCT, 0.21 ng/mL. The patient died 2 h after admission. The clinician suspected that the cause of death was sudden cardiac death.
External examination and autopsy
Forensic autopsy was performed 2 days after her death. External examination showed a well-nourished adult female, 145 cm in length, with no other fatal trauma other than rescue marks. A total of approximately 50 mL of light red fluid was seen in the bilateral thorax. Both lungs were congested and oedematous. The left lung weighed 600 g, and the right lung weighed 700 g. No lethal pathological changes were found in the other organs.
Histopathology examination
Haematoxylin and eosin (HE) staining showed no abnormalities in the nervous and cardiovascular systems. Both lungs showed severe pulmonary oedema and pulmonary haemorrhage (Fig. 1a). There were suspected microthrombi and vacuolar structures in the lumen of extensive small pulmonary interstitial vessels. PTAH staining and ORO staining were performed, and the results showed the PFE (Fig. 1b) and microthrombi (Fig. 1c-d). Immunohistochemistry of the spike protein (Cat. No. 99423, Cell Signaling Technology, Danvers, MA) and nucleocapsid protein (Cat. No. 26369, Cell Signaling Technology, Danvers, MA) were performed on the larynx, right ventricle, adrenal gland and thymus. Only the laryngeal epithelial cells were positive (Fig. 1e-f), and the other organs were negative (Supplementary Fig. 1a-f).
Discussion
Microthrombus embolism caused by SARS-CoV-2 has been a major threat of death. Ackermann et al. [3]. reported that the incidence of alveolar capillary microthrombi was 9 times higher in patients with COVID-19 than in patients with influenza. Autopsy results have shown that 80-100% of COVID-19 patients have microthrombi [4]. D-dimer is an important indicator indicating of thrombus formation. Fox et al. [5]. reported 10 autopsy cases of COVID-19 patients. Interestingly, six of these patients had significantly elevated D-dimers before death, and four were not tested. Their data suggested a correlation between elevated D-dimer levels and the outcome of fatal pulmonary embolism in COVID-19 patients. In this case, the patient is confirmed to be infected with SARS-CoV-2 by immunohistochemistry of the spike protein and nucleocapsids protein. The D-dimer level was much higher than the normal value, suggesting that the deceased was in a hypercoagulable state and most likely had thromboembolism. The results of HE and PTAH staining proved that she had microthrombus embolism. The current treatment guidelines related to COVID-19 worldwide mention the plan of anticoagulant therapy, which is the main reason why only 4% of the patients had pulmonary embolism cases occurred in the multicenter study of von Stillfried et al. [2].
Fat embolism is a pathological diagnosis of microvascular or capillary occlusion by lipid droplets in the lung or peripheral circulation. Since Zenker first described the presence of fat droplets in the lung of a railway worker who died of severe crush injury in the chest and abdomen in 1861, many scholars have explored the formation mechanism of fat embolism. The mechanical theory proposed by Guass [6] and the biochemical theory proposed by Lehman and Moore [7] have been accepted and applied by a large number of scholars.
On the basis of Lehman and Moore, Hulman et al. [8]. further confirmed the biochemical theory by conducting in vitro creaming tests on the serum of intensive care patients. Fat emboli are made up of chylomicron and very low density lipoprotein in the case of elevated plasma CRP and calcium dependency agglutination, forming a giant ball of fat with a diameter of 2–35 μm microns. CRP, an acute phase protein first described by Tillet and Francis, is a widely used biomarker of inflammation [9, 10]. Since early in the SARS-CoV-2 pandemic, high serum CRP concentrations, a good predictor of adverse outcome, have been associated with the severity and complications of COVID-19 patients [11]. To the best of our knowledge, there have been no reports of fatal PFE due to elevated CRP in patients with COVID-19. In this case, the CRP was as high as 26.55 mg/L before death, and the PCT was within the normal range, which could exclude the possibility of bacterial, fungal and parasitic infections. In the absence of other histopathological abnormalities, combined with the positive immunohistochemical results, it is reasonable to believe that the elevated CRP in this patient was caused by infection with SARS-CoV-2. According to the grading method of pulmonary fat embolism proposed by Falzi [12] and Sevitt [13], we evaluated the patient for grade III fatal PFE. Combined with the biochemical theory proposed by Lehman and Moore, we further believe that the patient was infected with SARS-CoV-2, which resulted in the formation of fatal PFE.
In addition to the widely accepted mechanical and biochemical theories, Cinti et al. [14]. proposed in 2020 that visceral fat necrosis and free fat droplet transfer into the vascular lumen in obese patients may be the key factors of SARS-CoV-2-induced pulmonary fat embolism. In 2022, Colleluori and Cinti et al. [15]. proved the authenticity of the conjecture by means of transmission electron microscopy and ORO staining. However, in this case, we did not find evidence of SARS-CoV-2 infection in the adipose tissue surrounding the right ventricle, adrenal gland and thymus (Supplementary Fig. 1a-f), so we cannot support this theory for the time being.
The clinical manifestations associated with fat embolism are known as fat embolism syndrome(FES). At present, the diagnostic criteria for FES mainly include Gurd’s criteria [16], Schonfeld’s criteria [17] and Lindeque’s criteria [18], but there is a lack of prospective studies with big data. In terms of laboratory diagnosis, in addition to the secondary criteria proposed by Gurd, IL-6 [19] and > 30% of macrophages in alveolar lavage fluid containing lipid droplets [20] are also considered as early diagnostic markers of FES. Imaging, as an auxiliary method, is characterized by interlobular septal thickening, ground glass opacity, diffuse nodules, and pulmonary consolidation [21]. However, these changes are still nonspecific. Yohsuke et al. [22]. detected fat in the right ventricle and pulmonary artery branches by computed tomography and magnetic resonance imaging of cadavers, providing an alternative method for the diagnosis of FE. In conclusion, a characteristic diagnosis of FES is still lacking and further studies are needed.
The treatment of FES is still at a supportive stage. Since the 1950s, people have tried a variety of drug treatments, including heparin, corticosteroids, albumin, aprotinin, hypertonic glucose, etc., but little effect has been achieved. The treatment of FES is still controversial and needs further research and exploration [23].
Conclusions
We report the first case of microthromboembolism in small pulmonary vessels and fatal PFE after infection with SARS-CoV-2. In addition to common complications, we should also pay attention to the possibility of PFE, both in the current infection with SARS-CoV-2 and long COVID.
Data Availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Abbreviations
- PFE:
-
Pulmonary fat embolism
- CRP:
-
C-reactive protein
- PCT:
-
Procalcitonin
- PTAH:
-
Phosphotungstic acid haematoxylin
- ORO:
-
Oil red O
- HE:
-
Haematoxylin and eosin
- FES:
-
Fat embolism sydrome
References
COVID-19 Weekly Epidemiological Update. In. World Health Organization. 2023. https://apps.who.int/iris/handle/10665/366680. Accessed 30 March 2023.
von Stillfried S, Bulow RD, Rohrig R, Boor P. First report from the german COVID-19 autopsy registry. Lancet Reg Health Eur. 2022;15:100330.
Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, Vanstapel A, Werlein C, Stark H, Tzankov A, et al. Pulmonary vascular endothelialitis, thrombosis, and Angiogenesis in Covid-19. NEW ENGL J MED. 2020;383(2):120–8.
McFadyen JD, Stevens H, Peter K. The emerging threat of (Micro)thrombosis in COVID-19 and its therapeutic implications. CIRC RES. 2020;127(4):571–87.
Fox SE, Akmatbekov A, Harbert JL, Li G, Quincy BJ, Vander HR. Pulmonary and cardiac pathology in african american patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med. 2020;8(7):681–6.
Gauss H. The pathology of fat embolism. Arch Surg. 1924;9(3):593–605.
Lehman EP, Moore RM. Fat embolism: Including experimental production without trauma. Arch Surg (Chicago. 1920) 1927, 14(3):621–62.
Hulman G, Fraser I, Pearson HJ, Bell PR. Agglutination of intralipid by sera of acutely ill patients. Lancet. 1982;2(8313):1426–7.
Tillett WS, Francis T, Serological reactions in pneumonia with a non-protein somatic fraction of pneumococcus. J Exp Med. 1930;52(4):561–71.
Morley JJ, Kushner I. Serum C-reactive protein levels in disease. Ann N Y Acad Sci. 1982;389:406–18.
Petrilli CM, Jones SA, Yang J, Rajagopalan H, O Donnell L, Chernyak Y, Tobin KA, Cerfolio RJ, Francois F, Horwitz LI. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ 2020:m1966.
Falzi G, Henn R. On pulmonary fat embolism after injuries with different periods of survival. Munch Med Wochenschr. 1964;106:978–81.
Sevitt S. The significance and pathology of fat embolism. Ann Clin Res. 1977;9(3):173–80.
Cinti S, Graciotti L, Giordano A, Valerio A, Nisoli E. COVID-19 and fat embolism: a hypothesis to explain the severe clinical outcome in people with obesity. INT J OBESITY. 2020;44(8):1800–2.
Colleluori G, Graciotti L, Pesaresi M, Di Vincenzo A, Perugini J, Di Mercurio E, Caucci S, Bagnarelli P, Zingaretti CM, Nisoli E, et al. Visceral fat inflammation and fat embolism are associated with lung’s lipidic hyaline membranes in subjects with COVID-19. INT J OBESITY. 2022;46(5):1009–17.
Gurd AR. Fat embolism: an aid to diagnosis. J Bone Joint Surg Br. 1970;52(4):732–7.
Schonfeld SA, Ploysongsang Y, DiLisio R, Crissman JD, Miller E, Hammerschmidt DE, Jacob HS. Fat embolism prophylaxis with corticosteroids. A prospective study in high-risk patients. Ann Intern Med. 1983;99(4):438–43.
Lindeque BG, Schoeman HS, Dommisse GF, Boeyens MC, Vlok AL. Fat embolism and the fat embolism syndrome. A double-blind therapeutic study. J Bone Joint Surg Br. 1987;69(1):128–31.
Prakash P, Sen RK, Tripathy SK, Sen IM, Sharma RR, Sharma S. Role of interleukin-6 as an early marker of fat embolism syndrome: a clinical study [published correction appears in Clin Orthop Relat Res. 2017;475(3):925]. Clin Orthop Relat Res. 2013;471(7):2340–6.
Karagiorga G, Nakos G, Galiatsou E, Lekka ME. Biochemical parameters of bronchoalveolar lavage fluid in fat embolism. Intensive Care Med. 2006;32(1):116–23.
Qi M, Zhou H, Yi Q, Wang M, Tang Y. Pulmonary CT imaging findings in fat embolism syndrome: case series and literature review. Clin Med (Lond). 2023;23(1):88–93.
Makino Y, Kojima M, Yoshida M, Motomura A, Inokuchi G, Chiba F, Torimitsu S, Hoshioka Y, Yamaguchi R, Saito N, et al. Postmortem CT and MRI findings of massive fat embolism. Int J Legal Med. 2020;134(2):669–78. https://doi.org/10.1007/s00414-019-02128-8.
Rothberg DL, Makarewich CA. Fat Embolism and Fat Embolism Syndrome. J Am Acad Orthop Surg. 2019;27(8):e346–55.
Acknowledgements
Not applicable.
Funding
This study was funded by the Foundation of the Opening of Key Laboratory of the Ministry of Public Security (grant no GABFYBL202201).
Author information
Authors and Affiliations
Contributions
Jiangwei Kong is responsible for autopsy, immunohistochemical experiments and manuscript writing. Tengfei Yang and Xingan Yang are responsible for the autopsy and the collection of documents. Fu Zhang and Xinbiao Liao are responsible for the revision of the paper. Sihao Du is responsible for the immunohistochemical experiments and the revision of the paper. Dongri Li is responsible for autopsy, proposing ideas and paper revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
This work does not require ethical approval. Written informed consent was obtained from the family of the deceased in this case report.
Consent for publication
Consent to publication was obtained from the patients parents to publish the data.
Conflict of interest
We declare that we have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.

12879_2023_8559_MOESM1_ESM.png
Supplementary Material 1: Fig 1. Immunohistochemistry in adipose tissue around the right ventricle, adrenal gland and thymus was negative. (Right ventricle: a, S protein; b, N protein. Adrenal gland: c, S protein; d, N protein. Thymus: e, S protein; f, N protein.)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kong, J., Yang, T., Zhang, F. et al. Pulmonary fat embolism: a potentially new fatal complication of SARS-CoV-2 infection. A case report. BMC Infect Dis 23, 576 (2023). https://doi.org/10.1186/s12879-023-08559-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08559-4