Abstract
Background
Coccidioidomycosis is a systemic infection caused by dimorphic fungi Coccidioides spp. endemic to Southwestern United States and Central and South America. A history of residence and travel in these areas is essential for the diagnostic of coccidioidomycosis, which has highly variable symptoms ranging from asymptomatic to severe, disseminated infection, and even death. Immunocompromised patients of coccidioidomycosis experience a high risk of dissemination, chronic infection, and mortality. Meningitis is one of the most deleterious coccidioidomycosis and can cause various life-threatening complications.
Case presentation
Here we report a case of Coccidioides posadasii meningitis in a 49-year-old female who returned to China after one and a half years residence in Los Angeles, USA. The repeated routine cultures using CSF for bacteria or fungi were all negative. To hunt for an infectious etiology, the state-of-the-art technology metagenomic next-generation sequencing (mNGS) was then utilized, suggesting Coccidioides posadasii. Organizational pathological examination and polymerase-chain-reaction (PCR) results subsequently confirmed the mNGS detection.
Conclusion
To our knowledge, cases for coccidioidal meningitis have been rarely reported in China. While global travelling may spread this disease across continents and make the diagnosis more difficult. mNGS can detect almost all known pathogens with high sensitivity and specificity, especially for uncommon pathogen, such as Coccidioides posadasii in China.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Coccidioidomycosis is a mycosis commonly caused by Coccidioides immitis and Coccidioides posadasii, which only spreads in the Southwestern United States and Central and South America [1,2,3]. Primary host exposure to Coccidioides is mainly via inhalation of aerosolized arthroconidia upon soil disruption [4]. Coccidioidomycosis commonly manifests as an asymptomatic infection or a mild respiratory infection in humans and other vertebrate hosts [5]. However, the disease can also cause disseminated infection, progressive pulmonary infection, and infections in other organs including skin, bone, brain, and meninges [6]. In addition, coccidioidomycosis presents diverse symptoms among different patients and along different disease stages. Both clinical and imageological presentations of coccidioidomycosis are not typical, making it easy to be misdiagnosed [6]. This disease is rarely reported in China. There are 39 reported cases of coccidioidomycosis in China during 1958–2017 [7]. The number of coccidioidal meningitis cases are even smaller.
Here we report a case of C. posadasii infected meningitis in a 49-year-old female who returned to China after one and a half years residence in Los Angeles, USA. During this period, the patient had tidied up the flowers and other plants in the garden for several times, probably inhaled Coccidioides spores, and then got infected. Traditional clinical diagnostic assays failed to identify the pathogen. Metagenomic next-generation sequencing (mNGS) was then introduced. mNGS is a new approach that can rapidly identify almost all known pathogens in clinical samples with high sensitivity and specificity. It has been used in many clinical practices, including meningitis [8]. In this study, C. posadasii was finally detected by mNGS from cerebrospinal fluid (CSF) sample.
Case presentation
A 49-year-old female patient complained of fever and headache for 32 day was hospitalized in the Department of Infectious Diseases of Guangzhou Panyu Central Hospital, Guangdong, China, on October 29th, 2020. She had lived for one and a half years in Los Angeles, USA and just returned to China 2 days before. While living in the United States, she traveled around Los Angeles and trimmed plants for several times in the garden.
The symptoms included a sudden onset of fever (39 °C), severe headache, and rash on her face and back while she was in Los Angeles on September 27th. The patient went to local hospitals several times, but computed tomography (CT) showed no abnormities on her head. She received symptomatic treatments, but had not fully recovered.
When admitted to our hospital, the patient was with headaches, fevers, vomiting, and maculopapular rashes (1.5 cm × 1.5 cm) on the face and back. Her white blood cell count (WBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) were slightly higher than the normal range, but her electrolytes was slightly lower. CT examinations revealed small nodules in the posterior apex of her left upper lobe and lateral segment of middle lobe of right lung, but no abnormalities in head.
The empiric combinatory therapy (ceftriaxone sodium 2 g daily and acyclovir 0.5 g q8h) for both viral and bacterial meningitis was given. A lumbar puncture was performed on day 34. The CSF opening pressure was greater than 400 mmH2O. CSF analysis demonstrated positive pandy test and negative cryptococcal antigen, gene Xpert MTB/RIF assay, and culture result (Fig. 1). Drug dehydration and other symptomatic treatments were added. But there was no relief of the symptoms.
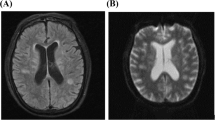
A lumbar puncture was repeated on the 39th day (Fig. 1). Autoimmune encephalitis spectrum results were positive of the anti-MOG-IgG antibodies for the serum and the CSF (1:32 and 1:3.2, respectively). To further identify the pathogen, PACEseq mNGS (Hugobiotech, Beijing, China) of CSF and blood was performed on a Nextseq 550 platform (Illumina, California, USA). A total of 308 unique sequence reads were finally aligned to the C. posadasii genome in CSF, which showed a dominant abundance of 2.32% in all microbial species after excluding the human reads from the total gene pool (Fig. 2). The blood mNGS showed negative of the pathogen. A targeted PCR of C. posadasii and Sanger sequencing were subsequently applied, which finally confirmed the mNGS detection of CSF (Fig. 3). In addition, the tissue biopsy of the patient’s back rash indicated HE Stain, PAS stain (+), and hexamine silver stain (+) (Fig. 4), which were also in line with coccidioidomycosis. Considering the abnormal signals in the bilateral parieto-occipital lobes and the meninges by magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA), the patient was finally diagnosed with C. posadasii infected meningitis.
The treatment was adjusted with fluconazole (800 mg intravenously daily) and ceftriaxone (4 g q24h). Other symptomatic treatments were also performed, such as mannitol (125 ml intravenously q8h) to reduce intracranial hypertension. The detailed treatments were shown in Fig. 1.
The patient gradually recovered over the next 7 days. The body temperature returned to normal, and the headache and dizziness relieved. Repeated lumbar puncture revealed the pressure at 200 mmH2O (Fig. 1). The patient's vital signs were stable. The patient was then transmitted to Third Affiliated Hospital of Sun Yat-Sen University for antifungal treatment with altericin B combined fluconazole. One month later, the patient’s symptoms improved and was finally discharged. She was required oral fluconazole. On February 2021, reexamine of the patient found high blood fat with intrajugular venous thrombosis and head sinus. The patient was given levarabban, oral anticoagulant therapy, fluvastatin, and oral calcium supplements. After 3-month follow-up, her headache aggravated with a increase intracranial pressure. The patient then received dehydration treatments.
Discussion and conclusions
Coccidioidomycosis is a systemic fungal infection caused by C. immitis or C. posadasii, which usually exist in hot and dry environment. In endemic areas, farmers and construction workers who frequently touch the soil have a higher prevalence [9]. Cases with disseminated coccidioidomycosis had a high risk (~ 50%) to develop into coccidioidal meningitis within weeks to months [10]. As one of the most deleterious coccidioidomycosis, coccidioidal meningitis can result in various life-threatening complications, including vasculitis, cerebral infarction, hydrocephalus, and Spinal arachnoiditis [11, 12]. Coccidioidal meningitis can also cause symptoms such as chronic persistent headaches, fever, nausea, and vomiting, and it is uniformly fatal in patients without treatment [6, 13]. In this study, the patient had lived in the United States for a long time with a history of touching soil and organizing flowers and plants in the garden. She experienced repeated fever, headache, and rash after the onset. Analysis of CSF and imaging examinations revealed infectious lesions. However, routine clinical tests, including culture did not find the pathogen. Finally, mNGS was used and successfully revealed coccidioidomycosis, which was later confirmed by PCR and biopsy results.
The routine diagnosis of coccidioidomycosis include immunologic assays, culture, and histopathology of tissues. However, there are many limitations. For example, serology is most commonly used, but the sensitivity is not ideal in the early diagnosis, especially for immunocompromised patients. mNGS is a new molecular diagnostic method which performs many advantages comparing with traditional methods. It can rapidly detect almost all known pathognes in one run with high sensitivity and specificity [14,15,16,17]. mNGS has been applied in pathogens detection in various clinical practices, such as meningitis, sepsis, and acute respiratory infection, especially for diseases infected by new, rare, difficult-to-culture, and mixed pathogens [6, 8, 18]. Due to the really low incidence of coccidioidomycosis in China, it was not first considered. So, the traditional methods failed to diagnose the pathogen. Fortunately, mNGS was used and finally detected the pathogen, which helped the diagnosis and timely treatment.
Due to the high mortality (90% in 1 year and 100% in 2 years) of coccidioidal meningitis in untreated patients, the early identification of pathogens and the timely antibiotic treatment is the key for a favorable prognosis [19]. However, the early diagnosis of coccidioidal meningitis remains a clinical challenge. This case indicated the possibility of mNGS as an early diagnostic measure for coccidioidomycosis, and proposes to employ this procedure in patients with relative symptoms and travel history.
Availability of data and materials
The data of this manuscript is available at http://ngdc.cncb.ac.cn/omix/preview/AAFXROl8, Reference Number PRJCA006430.
Abbreviations
- WBC:
-
White blood cell count
- CRP:
-
C-reactive protein
- ESR:
-
Erythrocyte sedimentation rate
- CSF:
-
Cerebrospinal fluid
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- MRA:
-
Magnetic resonance angiography
- PCR:
-
Polymerase chain reaction
- PPI:
-
Proton-pump inhibitor
References
Hector RF, Laniado-Laborin R. Coccidioidomycosis—a fungal disease of the Americas. PLoS Med. 2005;2(1):e2.
Twarog M, Thompson GR 3rd. Coccidioidomycosis: recent updates. Semin Respir Crit Care Med. 2015;36(5):746–55.
Welsh O, Vera-Cabrera L, Rendon A, Gonzalez G, Bonifaz A. Coccidioidomycosis. Clin Dermatol. 2012;30(6):573–91.
Cox RA, Magee DM. Coccidioidomycosis: host response and vaccine development. Clin Microbiol Rev. 2004;17(4):804–39, table of contents.
Smith CE, Beard RR, et al. Varieties of coccidioidal infection in relation to the epidemiology and control of the diseases. Am J Public Health Nations Health. 1946;36(12):1394–402.
Stockamp NW, Thompson GR 3rd. Coccidioidomycosis. Infect Dis Clin North Am. 2016;30(1):229–46.
Liang G, Shen Y, Lv G, Zheng H, Mei H, Zheng X, Kong X, Blechert O, Li D, Liu W. Coccidioidomycosis: imported and possible domestic cases in China: a case report and review, 1958–2017. Mycoses. 2018;61(7):506–13.
Wilson MR, Sample HA, Zorn KC, Arevalo S, Yu G, Neuhaus J, Federman S, Stryke D, Briggs B, Langelier C, et al. Clinical metagenomic sequencing for diagnosis of meningitis and encephalitis. N Engl J Med. 2019;380(24):2327–40.
Laws RL, Cooksey GS, Jain S, Wilken J, McNary J, Moreno E, Michie K, Mulkerin C, McDowell A, Vugia D, et al. Coccidioidomycosis outbreak among workers constructing a solar power farm—Monterey County, California, 2016–2017. MMWR Morb Mortal Wkly Rep. 2018;67(33):931–4.
Ho J, Fowler P, Heidari A, Johnson RH. Intrathecal amphotericin B: a 60-year experience in treating coccidioidal meningitis. Clin Infect Dis. 2017;64(4):519–24.
Johnson RH, Einstein HE. Coccidioidal meningitis. Clin Infect Dis. 2006;42(1):103–7.
Mischel PS, Vinters HV. Coccidioidomycosis of the central nervous system: neuropathological and vasculopathic manifestations and clinical correlates. Clin Infect Dis. 1995;20(2):400–5.
Johnson R, Ho J, Fowler P, Heidari A. Coccidioidal meningitis: a review on diagnosis, treatment, and management of complications. Curr Neurol Neurosci Rep. 2018;18(4):19.
Acewicz A, Witkowski G, Rola R, Ryglewicz D, Sienkiewicz-Jarosz H. An unusual presentation of Listeria monocytogenes rhombencephalitis. Neurol Neurochir Pol. 2017;51(2):180–3.
Simner PJ, Miller S, Carroll KC. Understanding the promises and hurdles of metagenomic next-generation sequencing as a diagnostic tool for infectious diseases. Clin Infect Dis. 2018;66(5):778–88.
Long Y, Zhang Y, Gong Y, Sun R, Su L, Lin X, Shen A, Zhou J, Caiji Z, Wang X, et al. Diagnosis of sepsis with cell-free DNA by next-generation sequencing technology in ICU patients. Arch Med Res. 2016;47(5):365–71.
Miao Q, Ma Y, Wang Q, Pan J, Zhang Y, Jin W, Yao Y, Su Y, Huang Y, Wang M, et al. Microbiological diagnostic performance of metagenomic next-generation sequencing when applied to clinical practice. Clin Infect Dis. 2018;67(suppl_2):S231–40.
Chen Y, Feng W, Ye K, Guo L, Xia H, Guan Y, Chai L, Shi W, Zhai C, Wang J, et al. Application of metagenomic next-generation sequencing in the diagnosis of pulmonary infectious pathogens from bronchoalveolar lavage samples. Front Cell Infect Microbiol. 2021;11:541092.
Stevens DA, Zhang Y, Finkelman MA, Pappagianis D, Clemons KV, Martinez M. Cerebrospinal fluid (1,3)-beta-d-glucan testing is useful in diagnosis of coccidioidal meningitis. J Clin Microbiol. 2016;54(11):2707–10.
Acknowledgements
We acknowledge all healthcare workers involved in the diagnosis and treatment of the patient.
Funding
This study was not supported by any specific grants or foundation.
Author information
Authors and Affiliations
Contributions
MY1 was involved in the literature review, planning and writing of the manuscript. FX was involved in case identification, literature review, planning and editing of the manuscript. LX, LH, SX, MY2, YL, and PF were involved in planning, writing and editing of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Competing interests
The authors have declared that no competing interests exist.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mao, Y., Li, X., Lou, H. et al. Detection of Coccidioides posadasii in a patient with meningitis using metagenomic next-generation sequencing: a case report. BMC Infect Dis 21, 968 (2021). https://doi.org/10.1186/s12879-021-06661-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-021-06661-z