Abstract
Background
Point-of-care ultrasound (POCUS) is becoming more prevalent in recent years for evaluating patients presenting with musculoskeletal injuries in the emergency department (ED). This imaging modality has been utilized to diagnose soft tissue and bony injuries accurately, obtain appropriate consultation, and perform timely interventional procedures in the ED.
Case presentation
We present the case of a 55-year-old man who presented to the ED with significant left ankle pain following a ground-level fall. His physical examination showed swelling and tenderness around the ankle. POCUS examination aided the rapid and accurate detection of acute Achilles tendon rupture.
Conclusion
This case demonstrates that POCUS is a valuable diagnostic tool in evaluating patients with a suspected Achilles tendon rupture, especially in a resource-limited setting.
Similar content being viewed by others
Background
Point-of-care ultrasound (POCUS) is becoming more prevalent in recent years for evaluating patients presenting with musculoskeletal injuries in the emergency department (ED). POCUS has been utilized to diagnose soft tissue and bony injuries accurately, obtain appropriate consultation, and perform timely interventional procedures in ED [1, 2]. Recent research studies have shown that POCUS can accurately identify long bone and metatarsal fractures, ligament injuries, and joint effusions distinguishing cellulitis from abscesses [3,4,5,6]. History and physical examination alone can miss up to 20% of tendon injuries in the initial phase, resulting in difficult repair and poor functional strength [5]. Because most tendons are relatively superficial, POCUS can easily identify these injuries. According to the literature, emergency physicians can use POCUS to identify tendon injuries with 100% sensitivity and 95% specificity [7]. We present a case of a partial Achilles tendon rupture in a middle-aged male patient who was rapidly diagnosed by POCUS in the ED, resulting in early management and orthopedic outpatient referral.
Case presentation
A 55-year-old man with a history of diabetes mellitus and seronegative rheumatoid arthritis presented to the ED of the Aga Khan University Hospital (AKUH), Karachi, with a complaint of pain and swelling in the left ankle and inability to bear weight on his left lower limb after a history of ground-level fall 2 h back. He initially went to an outside hospital, where an X-ray of his foot showed an avulsion fracture of the calcaneal bone (Fig. 1).
He was referred to AKUH for an orthopedic opinion. On arrival, he was vitally stable. The general physical and systemic examination was unremarkable. His musculoskeletal examination showed significant swelling and tenderness around the left ankle and difficulty bending the foot downward (plantarflexion) (Fig. 2). He had no sensory deficits and no overlying skin changes or open wounds.
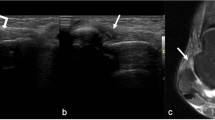
The on-call ED consultant performed a POCUS. The patient was lying prone with his feet hanging off the bed. A high-frequency linear probe was selected and placed on the posterior ankle in the long axis in a neutral position, which showed the disruption of the typical linear tendon fibers. Dynamic testing revealed the movement of the distal stump of the Achilles tendon adjacent to hypoechoic fluid, most likely reactive edema or blood from the acute rupture. Hyperechogenicity was also noted at the proximal end of the Achilles tendon, with acoustic shadowing probably representing an avulsed fragment of the calcaneum (Fig. 3).
Point-of-care ultrasound with a longitudinal view of the Achilles tendon. The white arrow indicates an avulsed fragment of calcaneum, the black arrow indicates the torn edge of the Achilles tendon, and the white triangle indicates calcaneum. Blue arrows indicate the proximal end and distal end (left to right). The red arrow indicates a possible hematoma between the torn edges of the Achilles tendon
His foot was splinted in the plantar flexion position, and an orthopedic follow-up was arranged in two days. His MRI (magnetic resonance imaging) of the foot was done on an outpatient basis as advised by the orthopedic consultant, who was reported as an “avulsion fracture of the calcaneum at the attachment site of the Achilles tendon with retraction of the partially ruptured Achilles tendon. The retracted ruptured end of the Achilles tendon is at the level of the distal articular margin of the tibia and is approximately 47mm from its attachment site. Significant surrounding soft tissue edema and hematoma are noted.” He was treated conservatively with analgesics and non-weight-bearing status.
Discussion
An Achilles tendon rupture diagnosis in the ED is often made solely based on history and physical exam; however, up to 20% of ruptures go unnoticed during the hyperacute phase and are frequently misdiagnosed as an ankle sprain [8]. Clinical examinations for diagnosing Achilles tendon rupture using diagnostic maneuvers, including the Thompson test and the presence of a palpable tendon defect, have shown sensitivities between 73 and 96%. Misdiagnosis and delayed treatment can lead to chronic discomfort, nonunion, and mobility issues [9]. MRI is often used to assess musculoskeletal complaints and is the study of choice when tendon rupture is suspected. This imaging modality provides greater anatomic detail and accuracy in detecting partial Achilles tendon rupture [10]. However, the utility of MRI in the ED is limited due to the longer scan times and higher expenses.
POCUS is a useful ancillary tool for evaluating soft tissue injuries in real time and at a lower cost. The sensitivity of ultrasound for detecting this type of injury ranges from 79 to 100%. The clinical utility of ultrasound in Achilles tendon injuries has previously been demonstrated [11,12,13,14]. It enables rapid bedside confirmation and distinguishes between partial and complete tears [15]. The patient should lie prone with feet hanging off the bed. A high-frequency linear probe should be used as it provides better resolution for superficial structures. The probe should be placed and slide gently over the Achilles tendon to identify different views. In a ruptured Achilles tendon, there will be a discontinuity in the tendon fibers, with the surrounding anechoic area representing the blood or edema. Dynamic assessment may show a lack of movement in the torn area during foot extension and flexion and can differentiate between full or partial-thickness tendon rupture.
Our case demonstrates the importance of POCUS in early decision-making and management of patients in a resource-limited country. Literature has shown that the POCUS has a positive impact on clinical decision-making in resource-limited settings, resulting in a decreased length of stay in EDs and a measurable reduction in planned referrals [16, 17]. Moreover, using POCUS also reduces the safety issues and costs associated with invasive and conventional testing like CT-scan and MRI [18].
Conclusion
POCUS is a practical and valuable modality to diagnose Achilles tendon rupture in patients presenting to the ED with a history of an ankle injury at the bedside. In combination with clinical history and examination, this can reduce ED stay and the number of expensive and time-consuming imaging resulting in cost-effectiveness, early decision-making, and planned referrals. POCUS is especially well-suited for resource-limited settings due to its quick accessibility of results and independence from additional infrastructure and staff (radiologists). As advancements continue, affordability and portability will further ease the adoption of POCUS over time.
Availability of data and materials
Available on reasonable request to noman.ali@aku.edu.
Abbreviations
- AKUH:
-
Aga Khan University Hospital
- ED:
-
Emergency department
- MRI:
-
Magnetic resonance imaging
- POCUS:
-
Point-of-care ultrasound
References
Situ-LaCasse E, Grieger RW, Crabbe S, Waterbrook AL, Friedman L, Adhikari S. Utility of point-of-care musculoskeletal ultrasound in the evaluation of emergency department musculoskeletal pathology. World J Emerg Med. 2018;9(4):262–6.
Waterbrook AL, Adhikari S, Stolz U, Adrion C. The accuracy of point-of-care ultrasound to diagnose long bone fractures in the ED. Am J Emerg Med. 2013;31(9):1352–6.
Pourmand A, Shokoohi H, Maracheril R. Diagnostic accuracy of point-of-care ultrasound in detecting upper and lower extremity fractures: an evidence-based approach. Am J Emerg Med. 2018;36(1):134–6.
Lee SH, Yun SJ. The feasibility of point-of-care ankle ultrasound examination in patients with recurrent ankle sprain and chronic ankle instability: comparison with magnetic resonance imaging. Injury. 2017;48(10):2323–8.
Chen K-C, Lin AC-M, Chong C-F, Wang T-L. An overview of point-of-care ultrasound for soft tissue and musculoskeletal applications in the emergency department. J Intensive Care. 2016;4(1):1–11.
Subramaniam S, Bober J, Chao J, Zehtabchi S. Point-of-care ultrasound for diagnosis of abscess in skin and soft tissue infections. Acad Emerg Med. 2016;23(11):1298–306.
Wu TS, Roque PJ, Green J, Drachman D, Khor KN, Rosenberg M, et al. Bedside ultrasound evaluation of tendon injuries. Am J Emerg Med. 2012;30(8):1617–21.
Hartgerink P, Fessell DP, Jacobson JA, van Holsbeeck MT. Full- versus partial-thickness Achilles tendon tears: sonographic accuracy and characterization in 26 cases with surgical correlation. Radiology. 2001;220(2):406–12.
Steginsky BD, Van Dyke B, Berlet GC. The missed Achilles tear: now what? Foot Ankle Clin. 2017;22(4):715–34.
Kayser R, Mahlfeld K, Heyde CE. Partial rupture of the proximal Achilles tendon: a differential diagnostic problem in ultrasound imaging. Br J Sports Med. 2005;39(11):838–42 discussion -42.
Adhikari S, Marx J, Crum T. Point-of-care ultrasound diagnosis of acute Achilles tendon rupture in the ED. Am J Emerg Med. 2012;30(4):634.e3-4.
Lee WJ, Tsai WS, Wu RH. Focused ultrasound for traumatic ankle pain in the emergency department. J Emerg Med. 2013;44(2):476–7.
Odom M, Haas N, Phillips K. Bedside ultrasound diagnosis of complete Achilles tendon tear in a 25-year-old man with calf injury. J Emerg Med. 2018;54(5):694–6.
Stickles SPFL, Demarest M, Raio C. Achilles tendon rupture. West J Emerg Med. 2015;16(1):161–2.
Pass B, Robinson P, Ha A, Levine B, Yablon CM, Rowbotham E. The Achilles tendon: imaging diagnoses and image-guided interventions—AJR expert panel narrative review. Am J Roentgenol. 2022;219(3):355–68.
Reynolds TA, Amato S, Kulola I, Chen CJ, Mfinanga J, Sawe HR. Impact of point-of-care ultrasound on clinical decision-making at an urban emergency department in Tanzania. PLoS ONE. 2018;13(4):e0194774.
Andersen CA, Holden S, Vela J, Rathleff MS, Jensen MB. Point-of-care ultrasound in general practice: a systematic review. Ann Fam Med. 2019;17(1):61–9.
Van Schaik GWW, Van Schaik KD, Murphy MC. Point-of-care ultrasonography (POCUS) in a community emergency department: an analysis of decision making and cost savings associated with POCUS. J Ultrasound Med. 2019;38(8):2133–40.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
NA- Conceptualization, Supervision and Writing, Reviewing, and Editing. JD- Investigation and Data Curation. NH, SS- Writing, Reviewing, and Editing. All authors read and approved final draft of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was taken from the Ethical Review Committee of Aga Khan University Hospital, Karachi, Pakistan. Ethics standards under the guidelines of the “Declaration of Helsinki” were followed. The patient provided written informed consent.
Consent for publication
The patient provided written informed consent for the publication of this case report and the images.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Habibullah, N., Dayo, J., Soomar, S.M. et al. Use of point-of-care ultrasound in a low-resource setting to diagnose Achilles tendon rupture and avulsion fracture of the calcaneal bone. Int J Emerg Med 16, 66 (2023). https://doi.org/10.1186/s12245-023-00544-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12245-023-00544-7