Abstract
Background
The diagnosis of periprosthetic joint infection (PJI) remains a challenge in clinical practice. Many novel serum and joint fluid biomarkers have important implications for the diagnosis of PJI. The presented study evaluated the value of joint fluid interleukin-6 (IL-6) combined with the neutral polymorphonuclear leukocyte (PMN%) ratio for chronic PJI diagnosis after arthroplasty.
Materials and methods
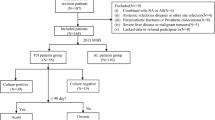
Sixty patients with chronic PJI or aseptic failure who underwent hip or knee revision from January 2018 to January 2020 in our department were included in this retrospective study. According to the 2013 MSIS diagnostic criteria, the 60 patients were divided into a PJI group and a non-PJI group (30 patients per group). We collected the joint fluid before surgery and determined the level of IL-6 and the PMN% by ELISA, and the differences between the two groups were compared. The diagnostic efficacy of joint fluid IL-6 combined with PMN% in chronic PJI was analyzed using a receiver operating characteristic curve (ROC curve).
Results
The diagnosis of PJI using joint fluid IL-6 combined with PMN% presented an area under the curve of 0.983, which was more accurate than the areas under the curve for diagnosis using IL-6 and PMN% individually (0.901 and 0.914, respectively). The optimal threshold values for IL-6 and PMN% were 662.50 pg/ml and 51.09%, respectively. Their sensitivity and specificity were 96.67% and 93.33%, respectively. The accuracy of the diagnosis of PJI was 95.00%.
Conclusions
Joint fluid IL-6 combined with PMN% can be used as an auxiliary method to detect chronic infection around the prosthesis after hip/knee arthroplasty.
Level of evidence
Patients who underwent hip/knee revision at the First Hospital of Chongqing Medical University for periprosthetic infection or aseptic failure of the prosthesis after hip/knee arthroplasty from January 2018 to January 2020 were included.
Trial registration This study was approved by the ethics committee of the First Hospital of Chongqing Medical University on September 26, 2018 (local ethics committee number: 20187101) and registered with the China Clinical Trials Registry (registration number: ChiCTR1800020440) with an approval date of December 29, 2018.
Similar content being viewed by others
Introduction
Total joint arthroplasty (TJA) is an effective treatment modality for end-stage bone and joint disease [1, 2]. Although there have been significant improvements in preventing periprosthetic joint infection (PJI), infection remains a significant challenge and a common cause of failure after TJA [3, 4]. The reported incidence of PJI is still between 0.5 and 2.0%, and it has become the leading cause of total knee arthroplasty failure and the third leading cause of total hip arthroplasty revision [5, 6]. In recent years, although there have been many advances in the diagnosis of PJI, distinguishing between post-arthroplasty infection and aseptic failure remains difficult in some cases. Therefore, establishing an accurate and timely diagnostic strategy is crucial for the management of PJI [7].
Many novel serum and joint fluid biomarkers, such as CD14, TREM-1, and TLR2, have shown promising potential in the diagnosis of PJI [8,9,10,11,12]. Qin et al. identified D-dimer as a valuable biomarker for the detection of chronic PJI. The combination of serum D-dimer and C-reactive protein (CRP) resulted in increased sensitivity compared to diagnosis based on serum D-dimer and CRP separately [1]. However, the detection techniques used for many biomarkers are not readily available in many hospitals, and there are varying degrees of controversy among different studies, making it difficult for the detection results to be widely used in clinical work. IL-6 is a cytokine produced by a variety of cells, including monocytes and macrophages, in response to immune responses, and can be significantly upregulated in pathogenic infection [13]. Neutrophils are the most abundant innate immune cells in the circulating blood, and they are one of the first lines of defense of the immune system against infections [8]. The diagnostic value of serum IL-6 in PJI was confirmed by previous studies, but its diagnostic sensitivity and specificity are not ideal [14].
Considering that the level of inflammatory markers in the joint fluid better reflects local inflammation [15], in this study, we tried to use IL-6 combined with PMN% in joint fluid to effectively identify the exact condition (chronic PJI or aseptic failure) in patients undergoing revision surgery after total joint arthroplasty and to obtain the threshold values for determining chronic PJI. This study also aimed to provide a reference for the diagnosis of chronic PJI.
Materials and methods
Study design and inclusion and exclusion criteria
This study was approved by the ethics committee of the First Hospital of Chongqing Medical University on September 26, 2018 (local ethics committee number: 20187101) and registered with the China Clinical Trials Registry (registration number: ChiCTR1800020440) with an approval date of December 29, 2018. Patients who underwent hip/knee revision at the First Hospital of Chongqing Medical University for periprosthetic infection or aseptic failure of the prosthesis after hip/knee arthroplasty from January 2018 to January 2020 were included. Inclusion criteria: age > 18 years; periprosthetic infection or aseptic failure of the prosthesis after initial replacement, with a recommendation for second-stage revision surgery; no other infection during the 2-year follow-up after hip/knee replacement. Exclusion criteria: (1) inflammatory arthritis, such as rheumatoid arthritis; (2) patients who had used antibiotics within the previous 2 weeks; (3) a history of petechiae, prosthetic heart valves, or hypercoagulation; (4) heavy smokers or patients with malignancy; (5) acute infections [16, 17].
The diagnostic criteria for chronic PJI were the isolation of pathogens from two or more separate tissue or fluid samples from around the involved prosthetic joint and the presence of at least four of the following six criteria: (1) elevated erythrocyte sedimentation rate (ESR) and CRP; (2) elevated joint fluid white blood cell count; (3) elevated joint fluid percent neutrophils (PMN%); (4) pus from the involved joint; (5) the isolation of microorganisms from periprosthetic joint tissue or fluid cultures; (6) periprosthetic histopathological specimens with a mean neutrophil count of 5 in five high-powered fields under high-powered microscopy. Patients were divided into a periprosthetic infection group (in which the patients had symptoms of infection, such as pain, that were present for more than 6 weeks after the implantation of the prosthesis) and a non-infected (non-PJI) control group [10].
Sample collection and determination
Clinical data relevant to the study included medical histories and laboratory examinations from patients undergoing revision surgery. The medical history included the patient’s age, gender, BMI, previous surgery, functional status of the affected limb at the current admission, presence of nocturnal or resting pain, presence of fever or a definite history of infection and comorbidities, and physical examination (whether the joint skin temperature was elevated, presence of redness, swelling, heat and pain, presence of sinus tract or pus). Laboratory examinations included serum CRP, ESR, PMN%, and joint fluid IL-6 testing on admission. In addition, all patients discontinued antibiotics for 2 weeks before arthrocentesis, and joint fluid was obtained by arthrocentesis at admission or preoperatively, with cell sorting and pathogenic microorganism culture. Histopathology and pathogenic microorganism culture of at least three periprosthetic tissues were performed intraoperatively. Microbial cultures of all specimens included aerobic, anaerobic, fungal, and prolonged cultures.
Immediately after admission, 1–2 ml of joint fluid were collected. 2 h after collection, all cellular and particulate components were removed by centrifugation at 1000 rpm for 10 min. The levels of IL-6 and PMN% in the joint fluid were measured using an IMMULITE 1000 immunoassay system (Siemens Healthcare, Erlangen, Germany). Serum ESR and CRP were measured by blood collection at admission and 1 day before surgery, respectively.
Statistical analysis
Categorical variables were analyzed using SPSS version 25 software (IBM Corp., Armonk, NY). Continuous variables were expressed as mean ± standard deviation, and categorical variables were expressed as counts and percentages. The independent samples t-test was used for measures that conformed to a normal distribution, and the Mann–Whitney U test was used to compare the differences between the two groups for measures that did not conform to a normal distribution. Correlations between variables were analyzed using Pearson’s correlation coefficient. MedCalc 15.2.2 software (MedCalc Software, Ostend, Belgium) was used to analyze the receiver operating characteristic (ROC) curves and the area under the curve (AUC) values. Youden’s j statistic was used to determine the optimal cut-off value for the diagnosis of chronic PJI. The sensitivity, specificity, accuracy, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio, negative likelihood ratio, and diagnostic odds ratio (DOR) were calculated for two serum markers (CRP, ESR) and joint fluid IL-6. p < 0.05 was considered statistically significant.
Results
Table 1 shows the demographics of the two groups. Thirty patients who were judged as having chronic PJI based on the MSIS 2013 diagnostic criteria were matched 1:1 with non-PJI patients according to age, sex, and body mass index (BMI). Thirty non-PJI patients were included in the control group (Table 1). The differences in the general data between the two groups, including age, weight, height, BMI, gender, and joint type, were not statistically significant (P > 0.05).
The levels of IL-6 and PMN% in joint fluid and of ESR and CRP in serum in both groups are shown in Table 2. The IL-6 concentration in joint fluid in the PJI group was 1154.50 (893.00) pg/ml, which was significantly higher than that in the non-PJI group, 390.50 (394.50) pg/ml (P < 0.001). The PMN% of joint fluid in the PJI group, 69.71% (25.85%), was significantly higher than that in the non-PJI group: 40.06% (22.49%) (P < 0.001). Serum ESR and CRP concentrations were not statistically different in the PJI (ESR: 35.00 (33.50) mm/h; CRP: 19.10 (18.40) mg/L) and non-PJI (ESR: 30.00 (16.00) mm/h; CRP: 16.40 (19.79) mg/L) groups (P > 0.05).
To assess the predictive value of joint fluid IL-6 and PMN% for chronic PJI, we developed a ROC diagnostic analysis model (Fig. 1), determined the optimal cut-off value from the ROC curve, and calculated the AUC to calculate the specificity, sensitivity, and accuracy of these markers for the diagnosis of chronic PJI. The AUC for joint fluid IL-6 was 0.901 (0.827 to 0.975) and the AUC for PMN% was 0.914 (0.841 to 0.988). The AUC for IL-6 combined with PMN% for the diagnosis of chronic PJI was 0.983 (0.959 to 1.000). The sensitivity for diagnosing chronic PJI was 83.33% (64.55 to 93.69%), the specificity was 83.33% (64.55 to 93.69%), and the accuracy was 83.33% when the critical value of joint fluid IL-6 was 662.50 pg/ml. When the critical value was 51.09%, the sensitivity of PMN% for detecting PJI was 96.67% (80.95 to 99.83%), the specificity was 73.33% (53.83 to 87.02%) and the accuracy was 85.00%. Further evaluation of the combined diagnostic value of joint fluid IL-6 combined with PMN% for chronic PJI showed a sensitivity of 96.67% (80.95 to 99.83%), specificity of 93.33% (76.49 to 98.84%), and accuracy of 95.00% for the diagnosis of chronic PJI (Table 3).
Table 4 shows the relevant diagnostic features of the inflammatory indicators IL-6 and PMN% in the synovial fluid. The PPV and NPV of IL-6 in synovial fluid for the diagnosis of chronic PJI were 83.33 and 83.33%, respectively (for a cutoff value of 662.50 pg/ml). The PPV and NPV of PMN% for the diagnosis of PJI were 78.38 and 95.65%, respectively (for a cutoff value of 51.09%), and the PPV and NPV of IL-6 combined with PMN% were 93.55 and 96.55%, respectively. The positive likelihood ratio, negative likelihood ratio, and diagnostic odds ratio (DOR) for IL-6 combined with PMN% in the patients’ synovial fluid were 14.50, 0.04, and 406, respectively. The positive likelihood ratio, negative likelihood ratio, and DOR for IL-6 were 5, 0.2, and 25, respectively, and the positive likelihood ratio, negative likelihood ratio, and DOR for PMN% were 3.625, 0.045, and 80.56, respectively.
Discussion
The clinical symptoms and laboratory markers that patients with chronic PJI may show are not obvious, which greatly increases the difficulty of diagnosing chronic PJI [3, 18,19,20]. Therefore, it is crucial to seek means that can accurately diagnose infection. In recent years, with the exploration of novel inflammatory markers and the study of prosthetic ultrasonic lysis culture and molecular diagnostic techniques, the diagnostic accuracy of PJI has been greatly improved [21, 22]. Considering that serum inflammatory markers may be affected by concomitant inflammation in other organs and systems, the assessment of local markers of the affected joint is more valuable for the diagnosis of PJI [7, 23, 24]. High levels of IL-6 in body fluids are associated with acute localized bacterial infections and are an anti-inflammatory factor and mediator of the infection response [25, 26]. Related studies have shown that serum CRP levels are elevated 4–6 h after IL-6 stimulation, suggesting that IL-6 is a relatively sensitive biomarker of early immune responses [27]. PMN is an important part of the human body and plays an important role in resisting microbial invasion and promoting the occurrence, development, and resolution of inflammation. Elevated synovial fluid PMN% has been identified as a useful marker for the diagnosis of PJI in previous studies [28]. In this study, we measured joint fluid IL-6 and PMN% levels in 60 patients to explore the value of joint fluid IL-6 combined with PMN% in distinguishing chronic PJI from aseptic failure, and we found that joint fluid IL-6 combined with PMN% has a high recognition accuracy (95.00%) for PJI.
Previous studies have demonstrated that IL-6 in joint fluid and blood is useful in the diagnosis of chronic PJI but cannot be used as the sole diagnostic criterion [29]. A prospective case–control study showed that serum IL-6 is a valuable and more accurate index for the diagnosis of PJI than ESR and CRP, with a sensitivity and specificity of 0.97 and 0.91, respectively, for the diagnosis of PJI [30]. A systematic evaluation conducted in 2018 explored the diagnostic accuracy of serum, synovial, and tissue tests for PJI and showed that joint fluid IL-6 had a good specificity (0.971) but varying degrees of decreased sensitivity (0.875) [31]. This result is similar to the present study, which found that the sensitivity of joint fluid IL-6 for chronic PJI was 83.33% and its diagnostic specificity was 83.33%, but the diagnostic accuracy of joint fluid IL-6 combined with PMN% for chronic periprosthetic infection after joint replacement was 95.00%, indicating that joint fluid IL-6 combined with PMN% has a higher diagnostic value for chronic PJI. Kai Xie et al. [25] also found that the AUC of joint fluid IL-6 levels for the diagnosis of PJI was higher than that of serum IL-6 levels, with an AUC of 0.96, a sensitivity of 91%, a specificity of 90%, and a diagnostic threshold of 2300 pg/ml. The detection of IL-6 with a threshold of 662.50 pg/ml in combination with the detection of PMN% with a threshold of 51.09% was found to provide the best discrimination between chronic PJI and aseptic failure of the prosthesis, yielding an accuracy of 95%. Its ability to significantly improve the accuracy of PJI diagnosis gives it superior clinical diagnostic significance.
This study has some limitations. First, there is currently a lack of a real gold standard for diagnosing PJI. We used the 2013 MSIS diagnostic criteria as the basis for grouping in this study, and some patients in the non-PJI group may have been false-negative patients, but this is a situation faced by all studies evaluating the diagnosis of PJI infection. Second, the sample size of our study was small. However, as an initial test, the current study has shown promising results, so a larger multicenter study could be conducted to further validate the findings. Finally, patients on antibiotics for two weeks before surgery were excluded from this study to eliminate confounding factors. However, this may have created testing prerequisites that differ from those used in clinical practice, limiting the generalizability of the results of this study.
Our study found significantly elevated IL-6 and PMN% values in the synovial fluid of PJI patients. Based on the MSIS criteria, IL-6 combined with PMN% had higher sensitivity and specificity for the diagnosis of chronic PJI. From the above analysis, we believe that IL-6 combined with PMN% in synovial fluid is a promising diagnostic index for PJI and may be included in the diagnostic criteria for PJI in the future. This combination of joint synovial fluid biomarkers can improve the accuracy of PJI diagnosis, providing clinicians with a more timely and accurate diagnosis of PJI, and bringing benefits to patients. Therefore, more research that focuses on finding biomarkers with high accuracy, cost-effectiveness, and feasibility is needed.
Conclusion
In this study, it was shown that the combination of joint fluid IL-6 and PMN% can be used as a specific molecular marker for the diagnosis of chronic PJI, and the most appropriate thresholds for IL-6 and PMN% were found to be > 662.50 pg/ml) and > 51.09%, respectively. This combination is more sensitive and specific in distinguishing aseptic failure after arthroplasty from chronic PJI than IL-6 or PMN% in joint fluid alone. However, there are few clinical examples of the combined use of joint fluid IL-6 and PMN% for the diagnosis of PJI, so more evidence is needed to support the use of joint fluid IL-6 combined with PMN% as a valid reference indicator for diagnosing PJI and determining the timing of prosthetic reimplantation.
Availability of data and materials
The data that support the fundings of this study are available from the corresponding author, Ning Hu, upon reasonable request.
Abbreviations
- PJI:
-
Prosthetic joint infection
- IL-6:
-
Interleukin-6
- ROC:
-
Receiver operating characteristic
- CRP:
-
C-reactive protein
- ESR:
-
Erythrocyte Sedimentation Rate
- SF:
-
Synovial fluid
- CI:
-
Confidence interval
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- AUC:
-
Area under the curve
- MSIS:
-
Musculoskeletal Infection Society
- MR:
-
Mannose-receptor
- G-CSF:
-
Granulocyte colony-stimulating
- TNF-α:
-
Tumor necrosis factor α
- IFN-γ:
-
Interferon γ
References
Qin L, Li F, Gong X, Wang J, Huang W, Hu N (2020) Combined measurement of D-dimer and C-reactive protein levels: highly accurate for diagnosing chronic periprosthetic joint infection. J Arthroplasty 35(1):229–234
Cai YQ, Fang XY, Huang CY, Li ZM, Huang ZD, Zhang CF, Li WB, Zhang ZZ, Guan ZP, Zhang WM (2021) Destination joint spacers: a similar infection-relief rate but higher complication rate compared with two-stage revision. Orthop Surg 13(3):884–891
Goswami K, Parvizi J, Maxwell Courtney P (2018) Current recommendations for the diagnosis of acute and chronic PJI for hip and knee-cell counts, alpha-defensin, leukocyte esterase next-generation sequencing. Curr Rev Musculoskelet Med 11(3):428–438
Kheir MM, Tan TL, Shohat N, Foltz C, Parvizi J (2018) Routine diagnostic tests for periprosthetic joint infection demonstrate a high false-negative rate and are influenced by the infecting organism. J Bone Joint Surg Am 100(23):2057–2065
Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ (2010) The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res 468(1):45–51
Gwam CU, Mistry JB, Mohamed NS, Thomas M, Bigart KC, Mont MA, Delanois RE (2017) Current epidemiology of revision total hip arthroplasty in the United States: national inpatient sample 2009 to 2013. J Arthroplasty 32(7):2088–2092
Qin L, Li X, Wang J, Gong X, Hu N, Huang W (2020) Improved diagnosis of chronic hip and knee prosthetic joint infection using combined serum and synovial IL-6 tests. Bone Joint Res 9(9):587–592
Marazzi MG, Randelli F, Brioschi M, Drago L, Romanò CL, Banfi G, Massaccesi L, Crapanzano C, Morelli F, Corsi Romanelli MM, Galliera E (2018) Presepsin: a potential biomarker of PJI? A comparative analysis with known and new infection biomarkers. Int J Immunopathol Pharmacol 31:394632017749356
Galliera E, Drago L, Vassena C, Romanò C, Gioia Marazzi M, Salcito L, Corsi Romanelli MM (2014) Toll-like receptor 2 in serum: a potential diagnostic marker of prosthetic joint infection? J Clin Microbiol 52(2):620–623
Raby AC, Holst B, Le Bouder E, Diaz C, Ferran E, Conraux L, Guillemot JC, Coles B, Kift-Morgan A, Colmont CS, Szakmany T, Ferrara P, Hall JE, Topley N, Labéta MO (2013) Targeting the TLR co-receptor CD14 with TLR2-derived peptides modulates immune responses to pathogens. Sci Transl Med 5(185):185
Shahi A, Parvizi J (2017) The role of biomarkers in the diagnosis of periprosthetic joint infection. EFORT Open Rev 1(7):275–278
Wetters NG, Berend KR, Lombardi AV, Morris MJ, Tucker TL, Della Valle CJ (2012) Leukocyte esterase reagent strips for the rapid diagnosis of periprosthetic joint infection. J Arthroplasty 27(8 Suppl):8–11
Mihara M, Hashizume M, Yoshida H, Suzuki M, Shiina M (2012) IL-6/IL-6 receptor system and its role in physiological and pathological conditions. Clin Sci 122(4):143–159
Randau TM, Friedrich MJ, Wimmer MD, Reichert B, Kuberra D, Stoffel-Wagner B, Limmer A, Wirtz DC, Gravius S (2014) Interleukin-6 in serum and in synovial fluid enhances the differentiation between periprosthetic joint infection and aseptic loosening. PLoS ONE 9(2):e89045
Huang S, Thomsson KA, Jin C, Ryberg H, Das N, Struglics A, Rolfson O, Björkman LI, Eisler T, Schmidt TA, Jay GD, Krawetz R, Karlsson NG (2022) Truncated lubricin glycans in osteoarthritis stimulate the synoviocyte secretion of VEGFA, IL-8, and MIP-1α: interplay between O-linked glycosylation and inflammatory cytokines. Front Mol Biosci 9:942406
Parvizi J, Gehrke T (2014) Definition of periprosthetic joint infection. J Arthroplasty 29(7):1331
Osmon DR, Berbari EF, Berendt AR, Lew D, Zimmerli W, Steckelberg JM, Rao N, Hanssen A, Wilson WR (2013) Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis 56(1):e1–e25
Sanzén L, Sundberg M (1997) Periprosthetic low-grade hip infections. Erythrocyte sedimentation rate and C-reactive protein in 23 cases. Acta Orthop Scand 68(5):461–5
Hackett DJ, Rothenberg AC, Chen AF, Gutowski C, Jaekel D, Tomek IM, Parsley BS, Ducheyne P, Manner PA (2015) The economic significance of orthopaedic infections. J Am Acad Orthop Surg 23(Suppl):S1-7
Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ (2009) The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am 91(1):128–133
Bergin PF, Doppelt JD, Hamilton WG, Mirick GE, Jones AE, Sritulanondha S, Helm JM, Tuan RS (2010) Detection of periprosthetic infections with use of ribosomal RNA-based polymerase chain reaction. J Bone Joint Surg Am 92(3):654–663
Haddad FS (2018) Next generation sequencing: is this the moment? Bone Joint J 100(2):125–126
Zhao J, Wang J, Liu Y, Han XX, Xu B, Ozaki Y, Zhao B (2022) Detection of prostate cancer biomarkers via a SERS-based aptasensor. Biosens Bioelectron 216:114660
Zhang L, Huang Y, Lin Y, Zhang A, Zou R, Xu H, Wang S (2022) Prognostic significance of CD56 expression in patients with multiple myeloma: a meta-analysis. Hematology 27(1):122–131
Xie K, Dai K, Qu X, Yan M (2017) Serum and synovial fluid interleukin-6 for the diagnosis of periprosthetic joint infection. Sci Rep 7(1):1496
Helfgott DC, Tatter SB, Santhanam U, Clarick RH, Bhardwaj N, May LT, Sehgal PB (1989) Multiple forms of IFN-beta 2/IL-6 in serum and body fluids during acute bacterial infection. J Immunol 142(3):948–953
Póvoa P (2002) C-reactive protein: a valuable marker of sepsis. Intensive Care Med 28(3):235–243
Kraus RF, Gruber MA (2021) Neutrophils—from bone marrow to first-line defense of the innate immune system. Front Immunol 12:767175
Grzelecki D, Walczak P, Szostek M, Grajek A, Rak S, Kowalczewski J (2021) Blood and synovial fluid calprotectin as biomarkers to diagnose chronic hip and knee periprosthetic joint infections. Bone Joint J 103(1):46–55
Di Cesare PE, Chang E, Preston CF, Liu CJ (2005) Serum interleukin-6 as a marker of periprosthetic infection following total hip and knee arthroplasty. J Bone Joint Surg Am 87(9):1921–1927
Gallo J, Svoboda M, Zapletalova J, Proskova J, Juranova J (2018) Serum IL-6 in combination with synovial IL-6/CRP shows excellent diagnostic power to detect hip and knee prosthetic joint infection. PLoS ONE 13(6):e0199226
Acknowledgements
Xudong Su and Bo Zhu are co-first authors and have the same status in the article.
Funding
General Project of the National Natural Science Foundation of China (project number: 82072443), Excellent Project of the Chongqing Overseas Returnee Entrepreneurship and Innovation Support Program (project number: CX2022032), General Project of the Chongqing Technology Innovation and Application Development Special Project (project number: Cstc2020jscx-msxmx0094), and the key project of the Chongqing Science and Health Joint Medical Research Project (project number: 2019ZDXM014).
Author information
Authors and Affiliations
Contributions
XS and BZ designed the study and wrote the preliminary manuscript. LQ, JY, LW, ZX, KW, JW, LC, CZ, CC, and WH did the analysis and interpretation of data and prepared the manuscript. NH and YX contributed to the study design and the final manuscript revision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This retrospective study was approved by the institutional review board of the First Affiliated Hospital of Chongqing Medical University on September 26, 2018 (local ethics committee reference No. 20187101), and was registered in the Chinese Clinical Trials Registry (registration number ChiCTR1800020440) with the approval date of December 29, 2018.
Consent for publication
All patients gave consent for publication.
Competing interests
Authors, cooperators, and sponsors have no potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Su, X., Zhu, B., Qin, L. et al. Joint fluid interleukin-6 combined with the neutral polymorphonuclear leukocyte ratio (PMN%) as a diagnostic index for chronic periprosthesis infection after arthroplasty. J Orthop Traumatol 24, 34 (2023). https://doi.org/10.1186/s10195-023-00712-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10195-023-00712-8