Abstract
Background
There is a paucity of data regarding the prevalence of preoperative deep vein thrombosis (DVT) in patients with long bone (including femur, tibia and fibula) fractures of the lower limbs. We performed a meta-analysis to address the issue.
Methods
Electronic databases, including PubMed, EMBASE, the Web of Science, the Cochrane Library, the VIP database, CNKI, and the Wanfang database, were systematic searched for original articles that reported the prevalence of preoperative DVT in long bone fractures of the lower limbs from January 2016 to September 2021. The prevalence of preoperative DVT was pooled using random-effects models, and subgroups were established according to study type, detection method, sample size and fracture site.
Results
Twenty-three articles reporting on 18,119 patients were eligible. The overall pooled preoperative DVT prevalence was 24.1% (95% CI 19.3–28.8%). In different subgroups, the preoperative DVT prevalences were 18.2–27.3%, 15.2–28.6%, 23.1–24.9%, 18.2–26.0% and 23.2–23.4% for different study designs, sample sizes, age groups, detection methods and fracture sites, respectively.
Conclusions
Despite the heterogeneity among studies, this systematic review suggests that the prevalence of preoperative DVT, which may seriously affect the prognosis of patients, is high. Therefore, greater efforts should be devoted to the improvement of screening and prevention strategies for preoperative DVT in lower-extremity long bone fractures.
Level of Evidence: Level III.
Trial Registration The study was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database with the registration number CRD42022324706.
Similar content being viewed by others
Introduction
Fractures of the long bones of the lower extremities, including the femur, tibia and fibula, are often accompanied by high-energy injuries. Fracture ends can cause venous endothelial damage, blood is in a post-traumatic hypercoagulable state, and bone traction and long-term bed rest-immobilization can result in slow blood flow, all of which meet the conditions for thrombosis. Therefore, deep vein thrombosis (DVT) is common in patients with fractures of long bones of the lower extremities. It has been reported that DVT in periprosthetic and lower extremity fractures accounts for more than 95% of DVT patients in traumatic orthopedics, while that in upper extremity fractures is rare, with an overall incidence of 0.69% [1,2,3]. DVT can lead to prolonged hospitalization and increased hospitalization expenses [4]. Also, subsequent post-thrombotic syndrome (PTS) and pulmonary embolism (PE) may seriously affect the patient’s life quality and even lead to their death [5, 6].
Perioperative DVT is divided into preoperative and postoperative DVT according to the occurrence time. Besides the consequences mentioned above, preoperative DVT may cause a delay to surgery, shifting it from the optimal surgical timing and thus affecting the outcomes; more seriously, if a thrombus is not detected in time preoperatively, orthopedic surgery will cause it to break off, leading to PTS, PE and other adverse outcomes [7]. However, the existing guidelines do not distinguish between preoperative and postoperative DVT in terms of screening and diagnostic strategies. For patients with lower extremity fractures, routine venous ultrasound is recommended [8]. The prevention and management of postoperative DVT has been given more attention than those of preoperative DVT. We believe that the clarification of the prevalence of preoperative DVT in patients with long bone fractures of the lower extremities will help improve the standardization of preoperative DVT prevention, screening, diagnosis and treatment, and is conducive to the rational allocation of health resources.
However, only a small part of the literature focuses on the prevalence of preoperative DVT, and the results show a large heterogeneity. The prevalence of preoperative DVT in patients with proximal femoral fractures was reported to be 52.50% [9], whereas studies from Hong Kong revealed that the prevalence of preoperative DVT after hip fracture in elderly Chinese patients was low (5.3%) without thromboprophylaxis. From their perspective, routine venous thromboprophylaxis in those patients was not recommended [10]. One study noted a preoperative DVT prevalence of 43.92% for tibial plateau fractures [11], whereas another study reported a prevalence of only 16.3% [12]. In conclusion, there are conflicting statements regarding preoperative DVT prevalence and prophylaxis.
This systematic review aimed to investigate the prevalence of preoperative DVT in patients with long bone fractures of the lower extremities, providing a basis for clarifying the disease burden of preoperative DVT and developing reasonable screening strategies and preventative measures.
Methods
Search strategy
We searched PubMed, EMBASE, the Web of Science, the Cochrane Library, the VIP database, CNKI, and the Wanfang database for articles reporting the prevalence of preoperative DVT in patients with long bone fractures of the lower extremities published between January 2016 and September 2021, using the following search terms: (Femoral Fractures OR Tibial Fractures OR Fibular fractures) AND Venous Thrombosis. A comprehensive search of the literature was performed to identify all relevant studies. The references of the included studies were searched manually. The study was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database with the registration number CRD42022324706.
Selection criteria
Inclusion criteria
The inclusion criteria were as follows: (i) studies containing sufficient information on the prevalence of preoperative DVT in long bone fractures of the lower extremities, which include femoral neck, femoral shaft, intertrochanteric, subtrochanteric, tibial plateau, tibial shaft and fibula fractures; (ii) clinical trials, case–control studies and cohort studies; (iii) the study population included patients with preoperative DVT determined by color Doppler ultrasonography, duplex ultrasonography or venography following long bone (femur, tibia or fibula) fractures of the lower extremities; (iv) studies with a score of ≥ 6 on the Newcastle–Ottawa scale (NOS).
Exclusion criteria
The exclusion criteria were as follows: (i) reviews, case reports, conference papers or animal studies; (ii) studies with incomplete data that could not be combined, duplicate publications, literature for which the full text was not available, or case–control studies from which the total number of patients (needed to calculate the DVT prevalence) could not be obtained; (iii) studies including patients with pathological fractures (fractures caused by bone tuberculosis, osteomyelitis, bone tumors, osteoporotic fractures, etc.); (iv) studies reporting the preoperative DVT prevalence in fractures at sites other than lower-extremity long bones that were not discussed separately, making it impossible to extract the required data; (v) the time order of DVT and surgery was not clearly defined; (vi) the subject was venous thromboembolism (VTE, divided into DVT and PE), and the DVT prevalence was unclear.
Article screening
The retrieved publications were managed using EndNote X9 software. Firstly, duplicates were eliminated by the software based on information such as title, author, year of publication, and journal. After that, two researchers independently read the titles and abstracts for initial screening, and then the full texts were downloaded so that they could be thoroughly reviewed. Any inconsistency in the process was decided by the third researcher.
Quality assessment
The included studies were independently evaluated in terms of study design by two investigators using the Newcastle–Ottawa scale [13]. Studies with NOS scores ≥ 6 were included in the subsequent analysis.
Data extraction
The extraction of data from the eligible studies was performed independently by two researchers. A third researcher decided in the case of disagreement. An Excel table was established to collect relevant information including, but not limited to, the first author, year of publication, study design, country, study duration, sample size, NOS score, locations of fractures, DVT detection method and preoperative DVT prevalence.
Statistical analysis
All statistical evaluations were made using StataSE 15 (64 bit). The prevalence of preoperative DVT was calculated as the simple rate and measured with 95% confidence intervals (CIs). Interstudy heterogeneity was tested using the I2 test, and when P > 0.1 and I2 ≤ 50%, the heterogeneity was considered statistically insignificant and a fixed-effects model was applied. Otherwise, a random-effects model was used. Subgroups were divided according to study type, testing modality, sample size, and fracture site, and the prevalence was estimated for different subgroups. Begg’s statistical test was performed to assess the publication bias.
Results
Study selection
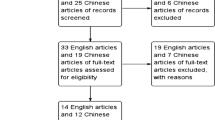
Of 3324 articles, 71 were eligible for full-text screening, and 23 original studies ultimately met the selection criteria (Fig. 1).
Study characteristics and quality assessment
For the 23 included studies, the years of publication ranged from 2016 to 2021, and, considered together, the durations of the studies covered the period from January 2010 to June 2020. The total number of lower extremity long bone fractures was 18,119, and the sample size in each study ranged from 119 to 7177. Eighteen studies had a NOS score of 7 and five studies had a NOS score of 6 (Table 1).
Prevalence of preoperative DVT in long bone fractures of the lower extremity
In the included literature, the reported preoperative DVT prevalence ranged from 5.10% to 52.50%, with significant heterogeneity between studies (p < 0.01, I2 = 98.7%), so a random-effects model was used. The pooled prevalence of preoperative DVT in long bone fractures of the lower extremities was 24.1% (95% CI 19.3–28.8%), as detailed in Fig. 2.
Begg’s test was performed on these 23 publications and found no significant publication bias (p > 0.05), as shown in Fig. 3.
Subgroup analysis
Study design
The 23 included papers were classified into different subgroups according to study design. Six were retrospective cohort studies, one was a nested case–control study, 13 were retrospective case–control studies, and three were prospective cohort studies.
The pooled prevalence was 18.2% (95% CI 8.0–28.4%) among retrospective cohort studies, 27.3% (95% CI 19.8–34.9%) among retrospective case–control studies and 26.2% (95% CI 14.8–37.7%) among prospective cohort studies (Fig. 4). A random-effects model was used due to significant heterogeneity.
Sample size
The 23 included papers were divided up according to the sample size. Fifteen had a sample size of ≤ 500, four had a sample size of 500–1000, and four had a sample size ≥ 1000.
The pooled prevalence was 28.6% (95% CI 21.1–36.1%) in the subgroup with a sample size of ≤ 500, 15.2% (95% CI 8.3–22.0%) in the subgroup with a sample size of 500–1000, and 17.3% (95% CI 5.4–29.2%) in the subgroup with a sample size of ≥ 1000, as shown in Fig. 5. The I2 test revealed significant heterogeneity, so a random-effects model was used for meta-analysis.
Mean age
Twenty-one publications reported relevant information on the patients’ mean age: the mean age in 15 studies was ≥ 50 years old, and that in six studies was < 50 years old.
The preoperative DVT prevalence was 24.9% (95% CI 18.4–31.4%) for patients with a mean age of ≥ 50 years old and 23.1% (95% CI 17.7–28.5%) for patients with mean age of < 50 years old (Fig. 6). Taking into account the significant heterogeneity, a random-effects model was used. The chi-square test was adopted to assess whether there was a statistical difference in DVT prevalence between the two subgroups (Pearson chi2 = 3.9219, P = 0.048).
DVT detection method
Subgroups were established according to the detection method: 12 used Doppler ultrasound, seven used duplex ultrasound, and two used venography. The remaining two did not specify the type of ultrasound used.
The preoperative DVT prevalence differed by detection method (18.2% [95% CI: − 3.0 to 39.5%] for the venography subgroup, 24.1% [95% CI 16.1–32.0%] for the duplex ultrasound subgroup, and 26.0% [95% CI 17.5–34.6%] for the subgroup that used Doppler ultrasound), as shown in Fig. 7.
Fracture site
Sixteen studies could be used to analyze the preoperative DVT prevalence of femoral fractures, and nine could be used to analyze that of tibiofibular fractures (two of them—those of Wang et al. [16] and Chang et al. [30]—included data related to both femoral and tibiofibular fractures), as detailed in Tables 2 and 3.
The preoperative DVT prevalence was 23.4% (95% CI 17.4–29.3%) for patients with femoral fractures and 23.2% (95% CI 15.3–31.1%) for patients with tibiofibular fractures, as shown in Fig. 8. There was significant heterogeneity, so a random-effects model was used.
Discussion
Based on our research, the pooled prevalence of preoperative DVT in lower-extremity long bone fractures was up to 24.1%. The results of these analyses suggest that the high prevalence of preoperative DVT, which is closely related to the patient’s prognosis, should be given more attention in clinical practice, and the differences in results between distinct subgroups indicate the influences of different factors in the formation of DVT.
Our study reported a higher preoperative DVT prevalence in patients with femoral fractures compared to tibiofibular fractures, which is generally consistent with the results of previous articles. Some studies have revealed that preoperative DVT prevalence was higher in femoral shaft fractures, proximal femoral fractures, and distal femoral fractures than in tibial plateau fractures and tibiofibular fractures [1, 34, 35]. Femoral fractures are usually due to higher energy, and vascular distribution in the thigh is dense, leading to severe endovascular injury and more bleeding, which contributes to a higher prevalence of DVT [1]. The classification method for fracture sites varied among the current studies, so our article is unable to provide more detailed categorization of the fracture sites. Our data indicate that DVT detection should be prioritized in patients with femoral fractures in the future due to the high prevalence of DVT in such fractures.
The prevalence of preoperative DVT in lower extremity fractures is higher in older adults than in younger adults, and the difference in DVT prevalence between these two subgroups was significant according to the results of a chi-square test. This finding suggests that advanced age may be an independent risk factor for the occurrence of preoperative DVT in long bone fractures of the lower extremities, which has been confirmed in previous studies [9, 17, 19]. Patients of advanced age are in a hypercoagulable state due to prolonged post-injury inactivity, and the poor vascular elasticity further increases the risk of DVT. Of note, eight of the included studies reported the use of prophylactic anticoagulation therapy (e.g., low-molecular-weight heparin) prior to the detection of DVT among patients with a mean age of ≥ 50 years. The use of antithrombotic medication could be a confounding factor that potentially influenced the results for different age subgroups. However, we cannot currently tell whether the age factor was influenced—and, if so, the degree of influence—due to a lack of evidence.
The sensitivity and specificity of DVT detection depended on the detection method. As previously noted [36], compared with venography, the sensitivity of duplex ultrasound for DVT detection was 92.1% and its specificity was 94.0%, whereas the sensitivity of the combined color Doppler ultrasound technique was 81.7% (77.4–85.5%) and its specificity was 92.7% (89.7–95.1%). However, the detection rate was lower in the color Doppler ultrasound subgroup than in the duplex ultrasound subgroup in our study. The workload of ultrasound examiners and the operational experience of physicians vary depending on the hospital, with some studies showing higher diagnostic consistency among experienced sonographers and a decrease in diagnostic consistency with less experience in hip ultrasound using Graf’s method [37]. The difference stated above may lead to differences in false-negative rates, thus affecting diagnostic accuracy. Differences in the location and time of ultrasound scanning between different studies (including scanning only the fractured lower limbs or scanning both lower limbs; performing one scan or multiple scans; etc.) may also be the source of error. The convenience and non-invasiveness of ultrasonography make it a first-line detection method for DVT despite its lower sensitivity compared to venography. In our analysis, the DVT prevalence was lower in the venography subgroup than in the two ultrasound subgroups, which does not seem to be consistent with the high sensitivity of venography. Shin [14] and colleagues performed venography only in patients, with a delay of over 24 h from the time of injury to surgery, which could lead to missed detection, while Song [15] and colleagues excluded patients with a history of VTE, which could lead to a lower DVT prevalence. The prevalence of preoperative DVT varied widely among the included studies. Chang [30] reported a DVT prevalence of only 5.10%, whereas in a study by Zhang [9], the prevalence of DVT was up to 52.5%. According to Zhang [9], DUS was conducted immediately after admission, but in the study of Chang [30], patients were all given subcutaneous low-molecular heparin injections upon admission, after which ultrasound was performed, implying that some patients who had formed a DVT might have been on heparin therapy before detection, which may explain the decrease in the prevalence of DVT. Among all the included studies, the timing of DVT detection was the first day after admission in four papers; 1 day before surgery in eight papers, seven of which mentioned prophylactic anticoagulation before testing; seven papers described the timing of testing only as "after admission" or "before surgery;" and the remaining three did not specify the timing of the study. The different timings of testing and anticoagulation strategies could lead to reduced comparability across studies. The existing guidelines, however, do not specify the timing and scanning area of preoperative DVT testing [8]. Our study suggests that preoperative DVT detection strategies need to be more standardized and detailed, which would provide guidance for the improvement of guidelines for perioperative DVT prevention and diagnosis.
The prevalence of DVT varied with the population characteristics. The DVT prevalence was lowest in the 500–1000 patient subgroup, with the lowest prevalence reported by Ma [27] and Niu [32]. The mean age of the sample in Ma’s [27] study was 44.6 years, which was much lower than the mean age across all the included literature; Niu's [32] study excluded patients with a history of VTE, which could have led to a lower risk of DVT at baseline in the included sample, thus explaining the low prevalence of DVT in this subgroup. We observed high degrees of heterogeneity in the prevalence estimates (I2 > 50%, p < 0.05), which could be explained by the differences in baseline risk of the patients. Some of the literature excludes patients with a history of DVT prior to admission, while a previous study showed that patients with a history of venous embolism had a significantly higher risk of reoccurring VTE after knee arthroscopy [38], suggesting that a history of DVT may influence preoperative DVT prevalence. A random-effects model was used to maintain the accuracy of the results due to the large heterogeneity between studies.
Our systematic review has several strengths. First, the studies included in this review were original studies of high quality and with a total sample size of 18,119, making it a large-scale study on the prevalence of preoperative DVT in lower extremity fractures. Second, our research provides a systematic estimation of the overall pooled prevalence of preoperative DVT in lower extremity fractures, and it further clarifies the prevalence of DVT in different subgroups to provide targeted referential suggestions for clinical work. Finally, most of the previous reviews discussed the postoperative prevalence of DVT, while our research focused on the preoperative prevalence of DVT in long bone fractures of the lower extremities, thus playing an important complementary role. The limitations of this study include the following. (i) Only nine of the studies included were cohort studies (which had the highest level of evidence), while the remaining 14 were case–control studies, which to some extent limits the level of evidence in the article. Also, there were some confounding factors in these studies, resulting in greater heterogeneity in the results. (ii) Twenty-two of the 23 articles included in this study sampled in China, and the data for the other article came from Korea. The lack of data from European and American countries could lead to poor extrapolation of our results for these populations. (iii) Given the accuracy of our results, we could not include some studies which did not distinguish DVT prevalence from VTE prevalence, which may have made the results less comprehensive. (iv) A substantial proportion (48%) of the included studies used anticoagulation before the detection of DVT, which may have resulted in an underestimate of the DVT prevalence. (v) One factor, the DVT detection time period, is not mentioned in some of the included studies, and the fracture sites could not be classified into more detailed categories, so we are unable to provide a corresponding estimate of DVT. This suggests that the timing of DVT screening, antithrombotic use and the fracture sites should be uniformly defined in future studies in order to derive a more scientifically rationalized focus for DVT screening.
This meta-analysis focused on the formation of preoperative DVT, and thus could help to lay greater emphasis on preoperative DVT screening and prevention. Existing guidelines only state that ultrasound should be routinely performed to clarify the diagnosis during the perioperative period in patients with lower extremity fractures (class IIA recommendation) [8]; they do not emphasize the importance of early preoperative DVT screening and prevention. In our study, the prevalence of preoperative DVT in lower extremity fractures was up to 24.1%. Considering that preoperative DVT may seriously affect the patient’s prognosis, high priority should be given to the screening and prevention of preoperative DVT in the management of lower extremity fractures.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available throughout the manuscript.
Abbreviations
- DVT:
-
Deep vein thrombosis
- PTS:
-
Post-thrombotic syndrome
- PE:
-
Pulmonary embolism
- PROSPERO:
-
International Prospective Register of Systematic Reviews
- NOS:
-
Newcastle–Ottawa scale
- VTE:
-
Venous thromboembolism
- CIs:
-
Confidence intervals
References
Zang JC, Ma XL, Ma JX, Jiang HQ, Li PF, Li YJ, Li FB, Han Z, Jiang X (2016) Epidemiological study on the incidence of deep vein thrombosis assosiated with fracture sites. Chin J Orthop 36(9):540–545. https://doi.org/10.3760/cma.j.issn.0253-2352.2016.09.005
Lu Y, Ma BT, Guo RL, Zhang JG, Wu YH, Pang GG, Xin JY, Ye WS, Zou YA, Wang Y, Dong Q, Wang XQ (2007) Deep vein thrombosis risk in orthopaedic traumatic patients. Chin J Orthop 27(9):693–698. https://doi.org/10.3760/j.issn:0253-2352.2007.09.012
Sun JP, Zhang K, Wang PF, Xue HZ, Sun L, Liu SG, Zhang BF, Li Z, Lin H (2019) Clinical characteristics and risk factors of proximal deep venous thrombosis in patients with fractures. Chin J Trauma 35(7):625–630. https://doi.org/10.3760/cma.j.issn.1001-8050.2019.07.008
Toker S, Hak DJ, Morgan SJ (2011) Deep vein thrombosis prophylaxis in trauma patients. Thrombosis. https://doi.org/10.1155/2011/505373
Datta I, Ball CG, Rudmik L, Hameed SM, Kortbeek JB (2010) Complications related to deep venous thrombosis prophylaxis in trauma: a systematic review of the literature. J Trauma Manag Outcomes 4(1):1. https://doi.org/10.1186/1752-2897-4-1
Stubbs MJ, Mouyis M, Thomas M (2018) Deep vein thrombosis. BMJ. https://doi.org/10.1136/bmj.k351
Wang T, Guo J, Long Y, Yin Y, Hou Z (2022) Risk factors for preoperative deep venous thrombosis in hip fracture patients: a meta-analysis. J Orthop Traumatol 23(1):19. https://doi.org/10.1186/s10195-022-00639-6
Zhou W, Cao FQ, Zeng RY, Jiang BG, Tang PF, Wu XB, Yu B, Hou ZY, Li J, Su JC, Liu GD, Yu BQ, Yuan Z, Ni JD, Chen YX, Fu DH, Tong PJ, Wang DL, Zhang DY, Zhang P, Zhang YF, Niu F, Yang L, Yang Q, Shi ZM, Zhou Q, Wang JW, Wang Y, He CJ, Che B, Zhao M, Xia P, Xiong LM, Cao LH, Chen X, Li H, Sun Y, Hu LC, Hu Y, Liu MF, Mi BB, Xiong Y, Xue H, Lin Z, Zhang YZ, Hu Y, Liu GH (2022) Expert consensus on diagnosis, prevention and treatment of perioperative lower extremity vein thrombosis in orthopedic trauma patients (2022 edition). Chin J Trauma 38(1):23–31. https://doi.org/10.3760/cma.j.cn501098-20210822-00451
Zhang J, Zhao K, Li J, Meng H, Zhu Y, Zhang Y (2020) Age over 65 years and high levels of C-reactive protein are associated with the risk of preoperative deep vein thrombosis following closed distal femur fractures: a prospective cohort study. J Orthop Surg Res 15(1):559. https://doi.org/10.1186/s13018-020-02089-4
Chan YK, Chiu KY, Cheng SW, Ho P (2004) The incidence of deep vein thrombosis in elderly Chinese suffering hip fracture is low without prophylaxis: a prospective study using serial duplex ultrasound. J Orthop Surg 12(2):178–183. https://doi.org/10.1177/230949900401200208
Fei C, Wei W, Zhang BF, Qu SW, Wang C, Sun JP, Li JH, Zhuang Y, Zhang K (2019) Incidence and risk factors of deep venous thrombosis in lower extremity in patients with tibial plateau fracture. Chin J Orthop Trauma 21(2):7. https://doi.org/10.3760/cma.j.issn.1671-7600.2019.02.002
Liu DW, Zhu YB, Chen W, Li JY, Zhao K, Zhang JZ, Meng HY, Zhang YZ (2020) Relationship between the inflammation/immune indexes and deep venous thrombosis (DVT) incidence rate following tibial plateau fractures. J Orthop Surg Res 15(1):241. https://doi.org/10.1186/s13018-020-01765-9
Wells GA, Shea BJ, O'Connell D, Peterson J, Tugwell P (2000) The Newcastle–Ottawa Scale (NOS) for assessing the quality of non-randomized studies in meta-analysis. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 24 Nov 2020.
Shin WC, Woo SH, Lee SJ, Lee JS, Kim C, Suh KT (2016) Preoperative prevalence of and risk factors for venous thromboembolism in patients with a hip fracture: an indirect multidetector CT venography study. J Bone Joint Surg Am 98(24):2089–2095. https://doi.org/10.2106/JBJS.15.01329
Song K, Yao Y, Rong Z, Shen Y, Zheng M, Jiang Q (2016) The preoperative incidence of deep vein thrombosis (DVT) and its correlation with postoperative DVT in patients undergoing elective surgery for femoral neck fractures. Arch Orthop Trauma Surg 136(10):1459–1464. https://doi.org/10.1007/s00402-016-2535-4
Wang H, Kandemir U, Liu P, Zhang H, Wang PF, Zhang BF, Shang K, Fu YH, Ke C, Zhuang Y, Wei X, Li Z, Zhang K (2018) Perioperative incidence and locations of deep vein thrombosis following specific isolated lower extremity fractures. Injury 49(7):1353–1357. https://doi.org/10.1016/j.injury.2018.05.018
Wang Z, Xiao J, Zhang Z, Qiu X, Chen Y (2018) Chronic kidney disease can increase the risk of preoperative deep vein thrombosis in middle-aged and elderly patients with hip fractures. Clin Interv Aging 13:1669–1674. https://doi.org/10.2147/CIA.S174691
Xia ZN, Xiao K, Zhu W, Feng B, Zhang BZ, Lin J, Qian WW, Jin J, Gao N, Qiu GX, Weng XS (2018) Risk assessment and management of preoperative venous thromboembolism following femoral neck fracture. J Orthop Surg Res 13(1):291. https://doi.org/10.1186/s13018-018-0998-4
Zhang BF, Wei X, Huang H, Wang PF, Liu P, Qu SW, Li JH, Wang H, Cong YX, Zhuang Y, Zhang K (2018) Deep vein thrombosis in bilateral lower extremities after hip fracture: a retrospective study of 463 patients. Clin Interv Aging 13:681–689. https://doi.org/10.2147/cia.S161191
Li J, Wang Q, Wang PF, Lu Y, Zhang BF, Li Z, Yang N, Tian D, Zhang K (2019) Perioperative deep venous thrombosis in patients with tibiofibular fracture. China J Orthop Trauma 21(11):952–958. https://doi.org/10.3760/cma.j.issn.1671-7600.2019.11.005
Fei C, Wang PF, Zhang BF, Wei W, Qu SW, Yang K, Li Z, Zhuang Y, Zhang K (2020) Incidence and risk factors of deep venous thrombosis of lower extremity in patients with intertrochanteric fractures. China J Trauma 36(03):251–258. https://doi.org/10.3760/cma.j.issn.1001-8050.2020.03.012
Li J, Wang Q, Lu Y, Li Z, Yang N, Tian D, Lin H, Zhang K (2020) Analysis of prevalence and risk factors of perioperative deep venous thrombosis in patients with intertrochanteric femur fractures. China J Trauma 36(06):536–543. https://doi.org/10.3760/cma.j.issn.1001-8050.2020.06.011
Wei Y, Li J, Zhang Y, Yu H, Xie J (2020) Prevalence rate and high-risk factors of preoperative lower-limb deep venous thrombosis in patients with hip fractures. J Clin Rehabil Tis Eng Res 24(27):5. https://doi.org/10.3969/j.issn.2095-4344.2756
Feng L, Xu L, Yuan W, Xu Z, Feng Z, Zhang H (2020) Preoperative anemia and total hospitalization time are the independent factors of preoperative deep venous thromboembolism in Chinese elderly undergoing hip surgery. BMC Anesthesiol 20(1):72. https://doi.org/10.1186/s12871-020-00983-2
Fu YH, Liu P, Xu X, Wang PF, Shang K, Ke C, Fei C, Yang K, Zhang BF, Zhuang Y, Zhang K (2020) Deep vein thrombosis in the lower extremities after femoral neck fracture: a retrospective observational study. J Orthop Surg. https://doi.org/10.1177/2309499019901172
Li JH, Zhang K, Zhang BF, Zhuang Y, Xue HZ, Qu SW, Fei C, Yang N, Tian D, Wang PF (2020) Relationship between the incidence of deep vein thrombosis during hospitalization and the energy of injury in tibial plateau fractures. Clin Appl Thromb Hemost. https://doi.org/10.1177/1076029620913948
Ma J, Qin J, Shang M, Zhou Y, Zhang Y, Zhu Y (2020) Incidence and risk factors of preoperative deep venous thrombosis in closed tibial shaft fracture: a prospective cohort study. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03685-z
Zuo J, Hu Y (2020) Admission deep venous thrombosis of lower extremity after intertrochanteric fracture in the elderly: a retrospective cohort study. J Orthop Surg Res 15(1):549. https://doi.org/10.1186/s13018-020-02092-9
Bai SC, Chen XY, Zhu CX, Zhang X, Lu YD, Lu J, Wei XL, Cui M, Liu YJ, Li FG (2021) Risk factors for preoperative venous thromboembolism in lower extremity in patients with tibial plateau fractures. China J Orthop 41(15):7. https://doi.org/10.3760/cma.j.cn121113-20210205-00137
Chang W, Wang B, Li Q, Zhang Y, Xie W (2021) Study on the risk factors of preoperative deep vein thrombosis (DVT) in patients with lower extremity fracture. Clin Appl Thromb Hemost. https://doi.org/10.1177/10760296211002900
Fan J, Zhou F, Xu X, Zhang Z, Tian Y, Ji H, Guo Y, Lv Y, Yang Z, Hou G (2021) Clinical predictors for deep vein thrombosis on admission in patients with intertrochanteric fractures: a retrospective study. BMC Musculoskelet Disord 22(1):328. https://doi.org/10.1186/s12891-021-04196-7
Niu S, Li J, Zhao Y, Ding D, Jiang G, Song Z (2021) Preoperative deep venous thrombosis (DVT) after femoral neck fracture in the elderly, the incidence, timing, location and related risk factors. BMC Musculoskelet Disord 22(1):264. https://doi.org/10.1186/s12891-021-04145-4
Zhu Y, Chen W, Li J, Zhao K, Zhang J, Meng H, Zhang Y, Zhang Q (2021) Incidence and locations of preoperative deep venous thrombosis (DVT) of lower extremity following tibial plateau fractures: a prospective cohort study. J Orthop Surg Res 16(1):113. https://doi.org/10.1186/s13018-021-02259-y
Zhou YJ, Lin J, Shi LT, Zhai D, Yang XH (2017) Comparative study on incidence of DVT at different position of lower limb fracture. J Chengde Med College 34(2):104–106
Zhang LP, Zhang ZZ (2019) Analysis of the incidence and location of perioperative deep vein thrombosis in single fracture of lower extremity. J Trauma Surg 21(6):435–437
Goodacre S, Sampson F, Thomas S, van Beek E, Sutton A (2005) Systematic review and meta-analysis of the diagnostic accuracy of ultrasonography for deep vein thrombosis. BMC Med Imaging 5:6. https://doi.org/10.1186/1471-2342-5-6
Cheng G, Ding Y, Fu QM, Chen X, Wang Y, Xiang X, Cai X (2017) Study for evaluating consistency of the hip using Graf’s method by sonographers with different experience under different conditions. J Clin Ultrasound Med 19(8):540–543
Krych AJ, Sousa PL, Morgan JA, Levy BA, Stuart MJ, Dahm DL (2015) Incidence and risk factor analysis of symptomatic venous thromboembolism after knee arthroscopy. Arthroscopy 31(11):2112–2118. https://doi.org/10.1016/j.arthro.2015.04.091
Acknowledgements
None.
Funding
This research was supported by Capital’s Funds for Health Improvement and Research (CFH2022-2-2074) and the Beijing Municipal Administration of Hospital Incubating program (PX2022015).
Author information
Authors and Affiliations
Contributions
YH: conception and design, article screening, data extraction and processing, interpretation of the data, drafting, final approval; LZ: conception and design, article screening, data extraction and processing, interpretation of the data, drafting, final approval; XT: supervision, final approval; FD: supervision, revision, final approval. All authors have agreed to the final version to be published and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants performed by any of the authors.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests for this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hu, Y., Zhu, L., Tian, X. et al. Prevalence of preoperative deep vein thrombosis in long bone fractures of lower limbs: a systematic review and meta-analysis. J Orthop Traumatol 24, 19 (2023). https://doi.org/10.1186/s10195-023-00699-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10195-023-00699-2