Abstract
Objective
Increased femoral anteversion (FA) has been correlated with less varus deformities in osteoarthritic (OA) knees, but the relationship between FA and the degree of valgus deformity in osteoarthritic (OA) knees is still largely unknown. We aimed to thoroughly analyze the distribution of FA in relation to varus or valgus deformities of the lower extremity in OA knees, and to further clarify the relationship between FA and trochlear morphology.
Methods
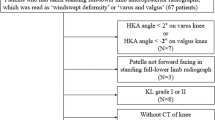
235 lower extremities with OA knees were divided into five groups according to the mechanical tibiofemoral angle: excessive valgus (< − 10°), moderate valgus (− 10° to − 3°), neutral (− 3° to 3°), moderate varus (3° to 10°), and excessive varus (> 10°). FA (measured using the posterior condylar axis [pFA] and the transepicondylar axis [tFA]) was measured, and the relationships of FA to the mechanical tibiofemoral angle and femoral trochlear morphology were identified.
Results
Excessive FA (pFA ≥ 20°) was observed in 30.2% of all patients and in 58.8% of patients in the excessive valgus group. pFA showed a strong correlation with mechanical tibiofemoral angle (p = 0.018). Both the pFA and the tFA of patients in the excessive valgus group were greater than those in other four groups (all p ≤ 0.037). There were significant correlations between tFA and trochlear parameters, including the sulcus angle (SA), lateral trochlear slope (LTS), and medial trochlear slope (MTS) (all p ≤ 0.028).
Conclusion
High FA is prevalent, particularly in severe valgus knees, and FA is significantly related to the femoral trochlear morphology in OA knees. With the aim of improving the patellofemoral prognosis and complications, high FA should be considered during total knee arthroplasty.
Similar content being viewed by others
Introduction
Patellofemoral complications (anterior knee pain, patellar maltracking) are common, with an incidence ranging from 5 to 12%, after total knee arthroplasty (TKA) for osteoarthritic (OA) knees [11]. These complications occur owing to excessive or uneven patellofemoral contact pressure or abnormal patellofemoral kinematics after TKA [13]. Accurate rotational alignments of the femoral component are fundamental to achieving satisfactory tibiofemoral and patellofemoral kinematics [4]. However, most studies on TKA have focused on the rotational profile of the distal femur alone. Only a few clinical studies have investigated the relationship of local rotational characteristics to the overall lower-extremity alignment, particularly the relative rotational positions of the femoral neck and distal femur in OA knees, namely femoral anteversion (FA).
Increased FA, which is defined as increased internal rotation of the distal femoral condyles relative to the femoral neck in the transverse plane, has been considered a predisposing factor for lateral patellar dislocation and one of the major risk factors for disparities between the patella and the trochlear groove [2], which affects patellar tracking and the patellofemoral joint contact pressure [5]. Previous studies have found that FA correlates to the coronal deformities of OA knees, but their relationships are still controversial [2, 4, 19]. Therefore, a thorough evaluation of the influence of FA variations in OA knees may help achieve satisfactory patellofemoral outcomes after TKA. Also, how FA influences the patellofemoral joint in OA knees is largely unknown.
Given the insufficient data in the literature, we aimed to analyze the distribution of FA according to coronal alignment and to further investigate how FA affects the parameters of femoral trochlear morphology in OA knees. We hypothesized that (i) a higher prevalence of abnormal FA (≥ 20°) can be observed in valgus than in varus deformities and (ii) FA would also show significant correlations with parameters related to the femoral trochlea in OA knees.
Materials and methods
Study population
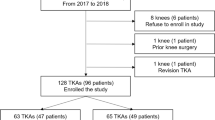
After obtaining institutional review board approval, we performed this retrospective study in patients who underwent primary TKA for knee osteoarthritis (Kellgren–Lawrence grades 3–4) between April 2015 and December 2020. Patients were included only when they had both preoperative standing full-limb anteroposterior radiography and axial computed tomography (CT) images of the femur and tibia. Patients were excluded if they met the following criteria: patellofemoral instability or dislocation, posttraumatic osteoarthritis, previous fracture or surgery of the lower extremity, neuromuscular dysfunction, rheumatic arthritis, or other types of inflammatory arthritis. Finally, a total of 145 patients (20 males and 125 females) providing 235 lower extremities were included in this study. The mean age and body mass index of the included patients were 67.8 years (47–87 years) and 26.4 kg/m2 (17.5–34.1 kg/m2), respectively.
Radiographic assessments
Coronal alignment of the lower extremity was measured using bilateral standing radiography (Philips Medical Systems, Best, Netherlands) of the entire lower extremity (Fig. 1) CT (SOMATOM Force; Siemens Inc., Munich, Germany) examinations were performed with the lower extremities fixed in neutral rotation in a supine position with the knees extended [4]. A specially developed CT protocol scanning including the femur and tibia was used [21, 22, 25]. The slice thickness of the axial CT images was 1 mm.
FA was separately measured between the femoral neck axis and the posterior condylar axis (pFA) and between the femoral neck axis and the clinical transepicondylar axis (tFA) [4] (Fig. 2). As for the morphological parameters of the femoral trochlea, the sulcus angle (SA) was the angle formed by the deepest point of the trochlear groove and the top points of lateral and medial anterior condyles [9]. The medial and lateral trochlear slopes (MTS, LTS) were those between the TEA (Transepicondylar axis) and the line connecting the deepest point of the trochlear groove and the top points of the lateral or medial anterior condyle, respectively[9]. The medial and lateral trochlear heights (MTH, LTH) were the lengths of the perpendicular lines connecting the TEA with the top points of the lateral and medial anterior condyles, respectively [18]. The ratio of the LTH and the MTH was defined as the bianterior ratio (BAC) [18]. To minimize the impact of bone size, the MTH and LTH values relative to body height were calculated (MTH-BH and LTH-BH, respectively) (Fig. 3). All parameters were measured using a picture archiving and communication system, with minimum detectable changes of 0.1° in angle measurement and 0.1 mm in length measurement [3]. All measurements were performed by two independent observers (two senior orthopedic residents). The observers repeated the measurements two times with a 3-week interval to minimize learning effects after the initial measurements. To assess the inter- and intraobserver reliability of the measurements, the interclass correlation coefficients of all parameters in all patients were used. All intraclass correlation coefficients of the interobserver and intraobserver reliabilities were high (Table 1).
Measurements of the morphology of the femoral trochlea. A SA: angle formed by the deepest point of the trochlear groove and the top points of the lateral and medial anterior condyles. LTS and MTS: angle formed between the TEA and the line connecting the deepest point of the trochlear groove and the top point of the lateral or medial anterior condyle, respectively. B LTH and MTH: length of the perpendicular line connecting the TEA and the top point of lateral or medial anterior condyle, respectively.
Statistical analysis
All statistical analyses were performed using SPSS (version 24.0; SPSS Inc., Chicago, IL, USA). All quantitative data in this study passed the test of normality (Kolmogorov–Smirnov test). Pearson correlation analysis was used to determine the relationships of FA to the mechanical alignment of the lower extremity and the femoral trochlear morphology. One-way analysis of variance and post hoc analysis were performed to determine the statistical significance of the differences in the degree of FA among five coronal alignment groups: excessive valgus (< − 10°), moderate valgus (− 10° to − 3°), neutral (− 3° to 3°), moderate varus (3° to 10°), and excessive varus (> 10°). A stepwise regression model using tFA and MTA was constructed. Sample size was calculated for a desired power of 80% and an α value of 0.05, and an estimated sample size of 216 was deemed to be required [19]. A p value of < 0.05 was considered statistically significant.
Results
An abnormal FA (≥ 20°) was observed in 30.2% of all patients and in 58.8% of patients in the excessive valgus group (Fig. 4). pFA negatively correlated with coronal alignment (r = − 0.154, p = 0.018; Table 2). In the subgroup analysis, pFA was, on average, approximately 7.41° to 7.95° greater in the excessive valgus group than in the other four groups (all p ≤ 0.016) (Fig. 5). Meanwhile, although no statistically significant correlation was found between MTA and tFA (r = − 0.118, p = 0.071) (Table 2), tFA was, on average, 6.16° to 6.54° greater in the excessive valgus group than in the other four groups (p ≤ 0.037) (Fig. 5).
With respect to the femoral trochlear morphology, tFA positively correlated with SA (r = 0.201, p = 0.002) and negatively correlated with LTS (r = − 0.144, p = 0.028) and MTS (r = − 0.169, p < 0.009) in OA knees (Fig. 6). Based on the regression analysis for all participants, tFA partly explained the variation of SA (β = 0.201, p = 0.002), LTS (β = − 0.144, p = 0.028), and MTS (β = − 0.150, p = 0.002), while MTA partly explained the variation of MTS (β = 0.162, p = 0.012) (Table 3). OA knees with pFA ≥ 20° had significantly greater SA (p = 0.024) and lower MTS (p = 0.032) than OA knees with pFA < 20° (Table 4).
Correlations of tFA with the morphology of the femoral trochlea, including the sulcus angle (SA), lateral trochlea slope (LTS), medial trochlea height (MTH), medial trochlea height (LTH), medial trochlea height (MTH), lateral trochlea height relative to body height (LTH-BH), medial trochlea height relative to body height (MTH-BH), and bianterior condyle ratio (BAC). *p < 0.05; **p < 0.01
Discussion
The main finding of this report is that high FA is prevalent, especially in OA knees with severe valgus deformity. On the other hand, increased FA is associated with flattening of the femoral trochlea.
It is well known that rotational deformities of the distal femur in varus or valgus OA knees should be considered for determining the femoral component rotation when performing TKA [4]. However, only limited data are available about the relationship of rotational deformities of the distal femur to the overall lower-extremity rotational alignment [4, 20]; specifically, quantitative data on the influence of FA during TKA, which are important for interpreting the rotational ability of the distal femur relative to the hip. There is no consensus on the relationship between the mechanical alignment of the lower extremity and the degree of FA in patients with OA knees in the few studies that address this issue [4, 19]. Moon et al. [4] assessed the degree of FA using the transepicondylar axis (tFA) instead of the conventional method of using the posterior condylar axis to eliminate the influence of the posterior condyle [1, 9, 17]. They found no correlation between the coronal alignment and the degree of FA, so they believe that the correlation between mechanical alignment and FA can be mainly attributed to the relationship between the posterior condylar geometry and the coronal alignment. However, Yoon et al. [19] reported that the tFA angle decreased as the degree of varus deformity increased. It should be noted that Moon et al. only generally divided coronal alignment deformities into varus and valgus groups, whereas Yoon et al. further divided the varus group into three subgroups, and almost one-third of the included OA patients had knees with excessive varus deformity (> 10°) in their study. Therefore, it is reasonable to speculate that the change in FA with mechanical alignment may be more evident in knees with excessive varus or valgus deformities. Accordingly, in the current study, we further divided the coronal deformities into five groups, including an excessive valgus group, which was not reported in the aforementioned studies. Our results verified our speculation that tFA was significantly greater in the excessive valgus group than in the other groups. In addition, over half (58.8%) of the OA patients in the excessive valgus group had excessive FA (≥ 20°) [6, 7], and this ratio was significantly greater than for other groups (around one-fourth to one-third). These findings demonstrate that high FA is prevalent, particularly in severe valgus knees. Despite substantial improvements in surgical technologies, the reported incidence of patellofemoral complications still varies from 5 to 12% [11, 23]. Increased FA has been considered a predisposing factor for patellar maltracking, which is one of the major reasons for patellofemoral complications after TKA [2, 5, 13]. Therefore, the prevalence of high FA in OA knees found in the current study may contribute to the high incidence of patellofemoral complications after TKA.
However, only limited knowledge is currently available on the clinical implications of variations in FA for TKA. Mobile-bearing TKA may have potential clinical applications because it can theoretically adjust for rotational malalignment through its self-aligning feature and improve patellar tracking. It has also actually been used for complex patellar maltracking in patients with valgus knee osteoarthritis with permanent patellar dislocation [8]. Additionally, as femoral derotational osteotomy for the treatment of patellar dislocation has been shown to achieve good clinical results [14], it is feasible to implement correction osteotomy at the distal femur for OA knees, as required during TKA operation.
Restoration of the femoral trochlear anatomy influences the functional outcomes of OA knees after TKA [15]. Besides coronal deformity of the lower extremity [24], FA has also been reported to relate to the morphology of the femoral trochlea in previous studies [5, 9, 12]. Liebensteiner et al. [9] investigated the trochlear sulcus and LTS, and their results showed that healthy knees have a shallower trochlear sulcus and a flatter LTS with a higher FA. Reikerhs et al. [12] and Diederichs et al. [5] found a weak or no correlation between FA and the trochlear sulcus or slope in a limited patient group with increased femoral anteversion. Most of these studies focused on healthy knees or knees with femoral trochlear dysplasia, but there has been little study of OA knees in this context. Our results showed that, apart from coronal deformities, increased FA is another important contributor to the flattening of the trochlea, and femoral trochleas with high FA (≥ 20°) were significantly flatter than those with normal FA. This flattening of the trochlea in OA knees with increased FA may be an adaption to the resulting increase in lateral patellofemoral stress. However, during TKA, when a surgeon performs a standard resection of the anterior cortex and uses a prosthesis with a uniform anterior femoral thickness regardless of the variable morphology of the femoral trochlea induced by FA, patellofemoral overstuffing or understuffing may occur after TKA [10, 16]. The present results may provide some useful information for the patellofemoral morphology design of femoral prostheses to accurately replicate femoral trochlea discrepancies according to FA for TKA.
This study had some limitations. First, we included only Asian patients. Racial disparities in FA or in morphological parameters related to the patellofemoral joint may exist, and caution should be used when applying the current results to populations of different ethnicities. Second, the current research lacked clinical results and did not analyze patellofemoral kinematics. Clinical and kinematic analyses of how FA affects the patellofemoral joint after TKA for OA knees should be further investigated to verify the clinical meaning of the current results.
Conclusion
In OA knees, high FA is prevalent, especially in knees with severe valgus deformity. Increased FA is associated with variable morphology of the femoral trochlea. With the aim of reducing the incidence of patellofemoral complications, the FA should be taken into account during TKA.
Availability of data and materials
Not applicable.
Abbreviations
- FA:
-
Femoral anteversion
- tFA:
-
FA using the transepicondylar axis
- pFA:
-
FA using the posterior condylar axis
- SA:
-
Sulcus angle
- LTS:
-
Lateral trochlear slope
- MTS:
-
Medial trochlear slope
- MTH:
-
Medial trochlear height
- LTH:
-
Lateral trochlear height
- OA:
-
Osteoarthritic
- TKA:
-
Total knee arthroplasty
- CT:
-
Computed tomography
References
Akman A, Demirkan F, Sabir N, Oto M, Yorukoglu C, Kiter E (2017) Femoral bowing plane adaptation to femoral anteversion. Indian J Orthop 51(1):49–54
Berger RA, Crossett LS, Jacobs JJ, Rubash HE (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 356:144–153
Chang CB, Choi JY, Koh IJ, Seo ES, Seong SC, Kim TK (2010) What should be considered in using standard knee radiographs to estimate mechanical alignment of the knee? Osteoarthritis Cartil 18(4):530–538
Chang MJ, Jeong HJ, Kang SB, Chang CB, Yoon C, Shin JY (2018) Relationship between coronal alignment and rotational profile of lower extremity in patients with knee osteoarthritis. J Arthroplasty 33(12):3773–3777
Diederichs G, Köhlitz T, Kornaropoulos E, Heller MO, Vollnberg B, Scheffler S (2013) Magnetic resonance imaging analysis of rotational alignment in patients with patellar dislocations. Am J Sports Med 41(1):51–57
Fabricant PD, Fields KG, Taylor SA, Magennis E, Bedi A, Kelly BT (2015) The effect of femoral and acetabular version on clinical outcomes after arthroscopic femoroacetabular impingement surgery. J Bone Joint Surg Am 97(7):537–543
Flury A, Hoch A, Andronic O, Fritz B, Imhoff FB, Fucentese SF (2020) Increased femoral antetorsion correlates with higher degrees of lateral retropatellar cartilage degeneration, further accentuated in genu valgum. Knee Surg Sports Traumatol Arthrosc 12:1760–1768
Kamada K, Matsumoto T, Takayama K, Araki D, Hashimoto S, Hayashi S (2017) Mobile bearing total knee arthroplasty for valgus knee osteoarthritis with permanent patellar dislocation: a case report and review of the literature. Case Rep Orthop 2017:1230412
Liebensteiner MC, Ressler J, Seitlinger G, Djurdjevic T, El Attal R, Ferlic PW (2016) High femoral anteversion is related to femoral trochlea dysplasia. Arthroscopy 32(11):2295–2299
Lozano R, Campanelli V, Howell S, Hull M (2019) Kinematic alignment more closely restores the groove location and the sulcus angle of the native trochlea than mechanical alignment: implications for prosthetic design. Knee Surg Sports Traumatol Arthrosc 27:1504–1513
Teel AJ, Esposito JG, Lanting BA, Howard JL, Schemitsch EH (2012) Patellar resurfacing in primary total knee replacement: a meta-analysis. J Bone Joint Surg Am 94:2270–2278
Reikerås O (1992) Patellofemoral characteristics in patients with increased femoral anteversion. Skelet Radiol 21(5):311–313
Terashima T, Onodera T, Sawaguchi N, Kasahara Y, Majima T (2015) External rotation of the femoral component decreases patellofemoral contact stress in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23(11):3266–3272
Tian G, Yang G, Zuo L, Li F, Wang F (2020) Femoral derotation osteotomy for recurrent patellar dislocation. Arch Orthop Trauma Surg 140(12):2077–2084
Varadarajan KM, Rubash HE, Li G (2011) Are current total knee arthroplasty implants designed to restore normal trochlear groove anatomy? J Arthroplasty 26:274–281
Werth L, Saffarini M, Amsler F, Abdelkafy A, Hirschmann MT (2017) The need for secondary resurfacing is affected by trochlear height in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:3818–3823
Xu Z, Zhang H, Chen J, Mohamed SI, Zhou A (2019) Femoral anteversion is related to tibial tubercle-trochlear groove distance in patients with patellar dislocation. Arthroscopy 36(4):1114–1120
Yang G, Dai Y, Dong C, Kang H, Niu J, Lin W (2020) Distal femoral morphological dysplasia is correlated with increased femoral torsion in patients with trochlear dysplasia and patellar instability. Bone Joint J 102-B(7):868–873
Yoon JR, Lee JK, Ryu J, Um R, Yang JH (2021) Increased external rotation of the osteoarthritic knee joint according to the genu varum deformity. Knee Surg Sports Traumatol Arthrosc 29(4):1098–1105
Zhao Z, Wang W, Wang S, Jiang L, Zhang S, Zhao Y (2015) Femoral rotation influences dynamic alignment of the lower extremity in total knee arthroplasty. Int Orthop 39:55–60
Hokari S, Tanifuji O, Kobayashi K, Mochizuki T, Katsumi R, Sato T, Endo N (2020) The inclination of the femoral medial posterior condyle was almost vertical and that of the lateral was tilted medially. Knee Surg Sports Traumatol Arthrosc 28(12):3858–3864
Yang Y, Zeng X, Jin Y, Zhu Z, Tsai TY, Chen J, Shen H, Li P (2022) The presence of cartilage affects femoral rotational alignment in total knee arthroplasty. Front Surg 16(9):802631
Goicoechea N, Hinarejos P, Torres-Claramunt R, Leal-Blanquet J, Sánchez-Soler J, Monllau JC (2021) Patellar denervation does not reduce post-operative anterior knee pain after primary total knee arthroplasty with patellar resurfacing. Knee Surg Sports Traumatol Arthrosc 29(10):3346–3351
Du Z, Chen S, Yan M, Yue B, Zeng Y, Wang Y (2017) Do size, shape, and alignment parameters of the femoral condyle affect the trochlear groove tracking? A morphometric study based on 3D-computed tomography models in Chinese people. BMC Musculoskelet Disord 18(1):4
Mochizuki T, Tanifuji O, Koga Y, Sato T, Kobayashi K, Nishino K, Watanabe S, Ariumi A, Fujii T, Yamagiwa H, Omori G, Endo N (2017) Sex differences in femoral deformity determined using three-dimensional assessment for osteoarthritic knees. Knee Surg Sports Traumatol Arthrosc 25(2):468–476
Acknowledgements
The authors would like to thank all the staff of the Department of Joint Surgery in The First Affiliated Hospital of Sun Yat-sen University for giving all kinds of support and help for this study.
Funding
This work was supported by the 5010 Clinical Research Project of Sun Yatsen University (2010005).
Author information
Authors and Affiliations
Contributions
CL—conception, drafting, substantial revision; CL, YY, and SH—searched the literature and analyzed the data; PH and DX—conception, substantial revision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from all subjects before the study. The ethics committee of the First Affiliated Hospital of Sun Yat-sen University approved the study protocol ([2011] 57).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, C., Ye, Y., He, S. et al. High femoral anteversion in osteoarthritic knees, particularly for severe valgus deformity. J Orthop Traumatol 23, 38 (2022). https://doi.org/10.1186/s10195-022-00653-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10195-022-00653-8