Abstract
Since the discovery of the Kv1.3 voltage-gated K+ channel in human T cells in 1984, ion channels are considered crucial elements of the signal transduction machinery in the immune system. Our knowledge about Kv1.3 and its inhibitors is outstanding, motivated by their potential application in autoimmune diseases mediated by Kv1.3 overexpressing effector memory T cells (e.g., Multiple Sclerosis). High affinity Kv1.3 inhibitors are either small organic molecules (e.g., Pap-1) or peptides isolated from venomous animals. To date, the highest affinity Kv1.3 inhibitors with the best Kv1.3 selectivity are the engineered analogues of the sea anemone peptide ShK (e.g., ShK-186), the engineered scorpion toxin HsTx1[R14A] and the natural scorpion toxin Vm24. These peptides inhibit Kv1.3 in picomolar concentrations and are several thousand-fold selective for Kv1.3 over other biologically critical ion channels. Despite the significant progress in the field of Kv1.3 molecular pharmacology several progressive questions remain to be elucidated and discussed here. These include the conjugation of the peptides to carriers to increase the residency time of the peptides in the circulation (e.g., PEGylation and engineering the peptides into antibodies), use of rational drug design to create novel peptide inhibitors and understanding the potential off-target effects of Kv1.3 inhibition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the discovery of the Kv1.3 K+ channel in human T cells in 1984 (Chandy et al. 1984; Matteson and Deutsch 1984) this channel was identified as a potential target for immunomodulation and consequently, several high affinity inhibitors were developed to block Kv1.3. These include small molecules derived from plant alkaloids (e.g., Psora-4, (Vennekamp et al. 2004)) and many of them are venom-derived peptides (Chandy and Norton 2017; Norton and Chandy 2017; Panyi et al. 2006). One of these peptides, the ShK toxin-based Dalazatide has already been approved for clinical trials targeting plaque psoriasis (Tarcha et al. 2017). It is quite intriguing to imagine why a K+ channel, rather than the more commonly known calcium-release activated Ca2+ channel (CRAC) of T cells (Feske et al. 2005), is the primary target in autoimmune diseases (Panyi et al. 2004a). The paragraphs below will briefly introduce this concept.
Upon antigen presentation (Fig. 1) activation of T cells requires a Ca2+ signal that depends critically on Ca2+ entry into the cytoplasm through the CRAC channel. This channel is formed by the pore-forming ORAI subunits in the plasma membrane and the STIM proteins embedded in the endoplasmic reticulum membrane (Feske et al. 2015). Once CRAC channels are open, the magnitude and the kinetics of the Ca2+ signal is determined by the electrochemical driving force for Ca2+ entry. The driving force for Ca2+ is governed by the interplay between the Ca2+ influx through the CRAC channels and the consequent depolarizing effect which is counterbalanced by two K+ currents, the K+ efflux through the voltage-gated Kv1.3 channel and the intermediate conductance calcium-activated KCa3.1 K+ channel (Cahalan and Chandy 2009; Feske et al. 2012, 2015). This K+ channel dependence of the membrane potential (~ − 50 mV), required for efficient Ca2+signaling, makes T cell activation sensitive to K+ channel blockers. It is interesting to note that direct block of the CRAC channels is also an option to modulate immune responses (Stauderman 2018), but the T cell and T cell subset-specific expression of Kv1.3 makes Kv1.3 a more attractive target, as introduced below.
The role of ion channels in T cell activation. T-cell receptor (TCR, top right) stimulation by a specific antigen (green triangle) leads to increased IP3 (green dots) concentration in the cytosol through the activation of phospholipase-C signaling cascade. The increased IP3 concentration activates the IP3-receptor (green channel) located in the smooth endoplasmic reticulum (sER) Ca2+ store. Ca2+-release through the activated IP3-receptor increases the Ca2+ (red dots) concentration of the cytosol and consequently the Ca2+ content in the sER stores decreases. This in turn activates store-operated Ca2+ entry through the interaction of the ER Ca2+ sensor STIM1 (blue protein) and the pore-forming unit of the functional CRAC channel, ORAI1 (red channel). The resultant inward Ca2+ flux will depolarize the cell membrane and activate the voltage-gated Kv1.3 channel (light purple channel with schematic voltage sensor), whilst the increased intracellular Ca2+ concentration enhances the activity of the Ca2+-activated KCa3.1 channel [light blue channel with the associated calmodulin (CaM)]. The activation of both voltage- and Ca2+-activated K+ channels will cause K+ efflux (purple dots) and consequently repolarize the membrane potential (Vm↓). Repolarization counteracts the depolarizing effect of Ca2+ entry through the ORAI1, thereby maintaining the electrical driving force for further Ca2+ entry. The complex interplay of ion channel activities generates a characteristic Ca2+ signal in activated T-cells (right middle of the cell) that regulates a plethora of cellular processes, leading to cell activation and cell type-specific effector functions
Activation and clonal expansion of lymphocytes is essential for the generation of an efficient immune response to pathogens and foreign antigens. Inhibition of immune responses, however, is required to prevent rejection of the transplanted organs or to treat autoimmune diseases where self-antigens are targeted. Suppression of T cell activation can be achieved using conventional immunosuppressive drugs, such as cyclosporin A, tacrolimus (FK-506) and rapamycin (Halloran 2004). As these molecules target second messenger pathways that are common in immune cells, e.g., inhibition of calcineurin by cyclosporin A (Schreiber and Crabtree 1992), their application results in generalized immunosuppression. This means that inhibition of T cell activation and proliferation is not specific for a given autoantigen-induced T cell population, and as such, the treatment increases the risk of infections (Kim and Perfect 1989; Lallana and Fadul 2011; Orlicka et al. 2013). In addition, nephrotoxicity of cyclosporin A and tacrolimus is significant even at doses used in the treatment of autoimmune diseases (Chighizola and Ong 2016; Halloran 2004). An ideal, selective immunosuppressor drug would target pathologically activated T cell subsets that induce tissue damage in autoimmune diseases (Chiang et al. 2017). T cells can be classified into various subsets based on their cell surface marker expression and functional states. A seminal paper by Wulff et al. (2003) described that Kv1.3 is uniquely overexpressed in activated CCR7− effector memory T (TEM) cells, whereas CCR7+ naïve and central memory T (TCM) cells preferentially express the KCa3.1 channel (Wulff et al. 2003). Upon the activation of naïve and TCM cells the expression of KCa3.1 increases substantially from 10–50 to 500–600/cell and as such, the activation and proliferation of these T cell subsets becomes KCa3.1-dependent. On the contrary, the Kv1.3 expression selectively increases from ~ 300 to ~ 1500/cell in TEM upon activation which makes their activation and proliferation sensitive to Kv1.3 inhibition. Since overactive and autoreactive T cells that induce tissue damage in many autoimmune diseases are TEM cells, and their activation and proliferation can be preferentially suppressed by selective Kv1.3 blockers without affecting naïve and TCM cells (Cahalan and Chandy 2009; Chandy and Norton 2017; Chi et al. 2012; Wulff et al. 2003), high affinity and high selectivity Kv1.3 inhibitors are good candidates for selective immunosuppression.
The applicability of Kv1.3 inhibitors in the management of numerous experimental autoimmune disease models has been demonstrated. Of these, the most significant progress has been achieved in the treatment of experimental autoimmune encephalomyelitis, a rat model for multiple sclerosis (Beeton et al. 2005). Kv1.3 blockers were shown to ameliorate the symptoms in pristane-induced MHC class II-restricted chronic arthritis model in rats, a model for rheumatoid arthritis, and in experimental autoimmune diabetes in rats (Beeton et al. 2005). Other diseases, where Kv1.3 inhibition and selective immunosuppression may be beneficial, are psoriasis (Kundu-Raychaudhuri et al. 2014) and Sjogren’s syndrome (Legany et al. 2016), and more recently, targeting of T cell subsets using Kv1.3 inhibitors in Inflammatory Bowel Diseases (Crohn’s disease and ulcerative colitis) has been proposed (Tajti et al. 2020). Furthermore, several neuroinflammatory diseases are proposed to be targeted by Kv1.3 inhibitors, including Alzheimer’s disease, where inhibition of Kv1.3 expressed in microglia seems to be important (Nguyen et al. 2017; Rangaraju et al. 2015). Several extensive reviews have addressed the applicability of ion channel blockers in the management of autoimmune diseases (Chandy and Norton 2017; Norton and Chandy 2017; Panyi et al. 2006; Serrano-Albarras et al. 2019; Tajti et al. 2020; Varga et al. 2010; Wulff et al. 2009).
Natural and conventionally engineered peptide toxin blockers Kv1.3
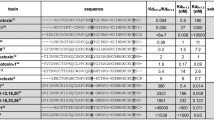
The Kalium database (http://kaliumdb.org), which is a collection of natural peptides acting on potassium channels mostly originating from the venoms of animals like scorpions, snakes, spiders and sea anemones, currently lists over 300 entries (Fig. 2). A large fraction of these toxins block or modify the gating of Kv1.3, but the active concentration varies widely over the range of pM to µM. While quite a few are active at nanomolar concentrations, only a handful of natural toxins has an affinity for Kv1.3 characterized by a Kd value in the pM range. Some of the most effective ones are the sea anemone toxin ShK (Kd = 11 pM, (Kalman et al. 1998)) and the scorpion toxins OSK1 (Kd = 14 pM, (Mouhat et al. 2005)), HsTx1 (Kd = 11 pM (Lebrun et al. 1997)) and Vm24, a toxin characterized by our group (3 pM) (Gurrola et al. 2012; Varga et al. 2012). They all share the typical structure of 30–40 residues stabilized by 3 or 4 disulfide bridges and use a critical lysine residue to protrude into the selectivity filter of the channel. Besides the lysine, other toxin residues also contribute to the high affinity binding via pairwise interactions with channel residues. These influential residues vary among the toxins, so it is not surprising that their selectivity profile among K+ channels also varies. On the other hand, topological similarity of the outer pore region among K+ channels, especially closely related ones, which forms the docking site for toxins may result in comparable affinities of a given toxin for multiple channels. For example, in addition to the high affinity for Kv1.3, ShK also potently blocks Kv1.1, Kv1.4 and Kv1.6, OSK1 blocks Kv1.1 and Kv1.2, while HsTx1 also blocks Kv1.1. Interestingly, Vm24, the toxin that we described showed the best selectivity in its natural form as it proved to be more than 1500-fold selective over ten other ion channels tested. For potential therapeutic use a minimum of 100-fold selectivity is desired of a compound, which is rarely found in natural toxins if they are tested on multiple channels.
Strategies to obtain Kv1.3 inhibitor peptides discussed in the paper. Native peptides can be isolated from venomous animals, like scorpions (https://upload.wikimedia.org/wikipedia/commons/f/ff/Vaejovis_Mexicanus.jpg). Alternatively, peptide toxins can be generated using recombinant techniques or solid phase peptide synthesis (not shown). Peptide modifications can be rationalized based on sequence analysis and docking, or can be the result of artificial intelligence (AI)-based design (https://www.innoarchitech.com/blog/artificial-intelligence-deep-learning-neural-networks-explained). Phage display technology can work together with molecular biology to result in novel peptides (immobilized channels are in blue, phages display various peptides indicated by red objects, the ones carrying diamonds bind the channel). Dashed arrow indicates other approaches not discussed in the review, e.g., venom gland transcriptome analysis. The target of the peptide (green ribbon diagram) is the Kv1.3 channel (purple) in effector memory T cells (TEM) and the diseases where peptides can be used as experimental therapeutic tools are listed in the bottom. Dashed arrow indicates other diseases not discussed in the review
Due to their inherent high affinity for their targets these toxins are attractive lead compounds for drug development, and consequently significant effort has been invested into improving their selectivity. Careful systematic sequence analysis along with mutational and docking simulation studies have identified residues both in toxins and in channels that are determinants of strong binding. This information allowed the engineered modification of toxins to tailor their selectivity in the desired direction (Fig. 2). For example, in the case of HsTx1 docking and molecular dynamics simulations were used to predict the effect of point mutations in the toxin sequence on binding to Kv1.3 (Rashid et al. 2014). Confirming the predictions, the HsTX1[R14A] mutant retained its high affinity for Kv1.3 but barely blocked Kv1.1, improving its selectivity to over 2000-fold for Kv1.3 over Kv1.1. Similar enhancement of toxin selectivity was achieved with OSK1 and AnTx based on sequence analysis and comparison with other K+ channel-blocking toxins. In OSK1, a double mutant version showed improved affinity for Kv1.3 with a Kd = 3 pM, but without any gains in selectivity (Mouhat et al. 2005). However, an additional mutation brought on great improvement in selectivity, although with a slight decrease in affinity for Kv1.3. Likewise, our group used sequence analysis to design a modified version of AnTx, a scorpion toxin blocking Kv1.2 and Kv1.3 channels with similar potencies, in order to improve its selectivity for Kv1.3 (Bartok et al. 2015a). The AnTx[N17A/F32T] double mutant version maintained the high affinity of the natural toxin for Kv1.3 while losing its potency for Kv1.2, resulting in a selectivity over 16,000-fold. Subsequent NMR-based structure analysis showed different flexibilities of the natural and modified toxin, which probably underlies the observed difference in selectivity.
How much the pharmacological properties of a natural toxin can be refined by engineered modifications is best exemplified by the ShK toxin (Pennington et al. 2009), which has been developed into an experimental drug for autoimmune diseases called Dalazatide (Tarcha et al. 2017). Based on docking simulations first the critical lysine of ShK was mutated to a non-natural amino acid to improve toxin selectivity (Kalman et al. 1998). Then various N-terminal extensions were tested, of which the addition of a phosphotyrosine via a linker proved advantageous for toxin properties. However, this molecule, ShK-170, had stability problems especially at higher temperatures due to pH-related hydrolysis and oxidation processes (Pennington et al. 2009). To overcome these problems several analogs were produced, of which ShK-192 containing a methionine isostere and a C-terminal amide was found to be the most stable. The modified toxin was confirmed to be a potent and selective blocker of Kv1.3, which effectively inhibited the proliferation of TEM cells and suppressed delayed-type hypersensitivity in rats. It could be detected in the blood at effective channel-blocking concentrations even 72 h after a subcutaneous injection. It was also found to be non-toxic in trials as long as 4 weeks, as judged by blood cell counts, blood chemistry or histopathology. Thus, the multi-aspect refinement of the natural ShK toxin serves as a proof of concept for the pharmacological value of peptide toxins.
Artificial Intelligence (AI)-guided drug design and phage display: novel alternatives to drug discovery
The examples above demonstrate the power of rational drug design, which is expected to receive a boost from artificial intelligence (AI) via machine learning techniques (Fig. 2), as increased computing power and more sophisticated algorithms will allow more accurate predictions. Despite the ever deeper understanding of the molecular mechanisms underlying diseases and great advancements in medical methods and technology, the introduction of new drugs continues to be a very time-consuming and costly procedure. Although the last few years show a promise of some improvement, data from the past two decades indicate that about 90 percent of drugs entering Phase I trials eventually fail to make it to approval (Mullard 2019; Smietana et al. 2016).
AI is envisioned to gain increasing roles in multiple aspects of drug development in the future such as prediction of peptide structures from primary sequences, the interaction of drug molecules with target proteins, the binding affinity, the physicochemical, pharmacokinetic and toxicity parameters of potential drug molecules, the repurposing of currently used drugs (Fernandez-Ballester et al. 2020) and even the prediction of potential side effects. Efforts are also being made to use AI techniques for virtual screening to replace high throughput screening as the initial step in testing and scoring the binding of molecules of large libraries to target proteins in silico.
As the pharmacological characterization of peptide toxins demands substantial experimental work, the targets of most toxins have not been identified yet, and most of the rest have only been tested on a limited number of ion channels. Thus, the possibility of predicting the targets solely based on primary sequence or basic structure by computational methods seems tempting. It is reasonable to assume that closely related toxins, especially those sharing identical disulfide bridge structures and some residues at key positions will bind to the same or very similar channels. Many supporting examples can be found for this notion among toxins blocking KV channels (Bartok et al. 2015b). However, counterexamples also exist, for example among spider toxins with high sequence similarities having different ion channel families as targets (Diochot et al. 1999; Middleton et al. 2002). Yet, the viability of the approach is supported by a study, in which the most likely ion channel target type was identified for a large number of conotoxins, peptides from the venoms of cone snails, with high accuracy simply based on their primary sequences with improved machine learning algorithms (Asuncion 2019).
Thus, bioinformatics methods that use statistical analysis to determine patterns and descriptors from the primary structure of peptide toxins may be used to identify plausible target ion channel families, such as KV versus NaV channels. However, currently these methods seem inadequate to predict selectivity among channel subtypes within the families, which would be crucial to avoid undesired reactions with off target channels during a potential therapeutic application (Kaas and Craik 2015).
Prediction of toxin-channel interactions to that detail requires the use of docking programs or molecular dynamics simulations. Current docking programs aim to find the correct orientation of the peptide blocker as it binds to the channel surface based on interatomic forces and surface potentials. Even though by now many docking programs exist, their use requires many approximations. An essential prerequisite for predicting blocker binding is detailed knowledge of the channel structure. Obtaining structures by X-ray crystallography required tedious long-lasting work with low success rate, but with the advent of improved cryo-EM techniques the number of determined structures grows daily at an increasing rate (Lau et al. 2018). Of these, the structure of the rat Kv1.2/Kv2.1 paddle chimera in lipid nanodisks was determined recently using cryo-EM which provides highly relevant data for the pore architecture of a K+ channel closely related to Kv1.3 (Matthies et al. 2018). Although the X-ray crystal structure of Kv1.3 is currently not known, a cryo-EM structure of the channel is under review (http://dx.doi.org/10.2139/ssrn.3467250). Analysis of the cryo-EM structure of the bacterial NavAB/human Nav1.7 Na+ channel chimera in complex with the tarantula toxin Huwentoxin-IV allowed the identification of the key toxin residue that interacts with the voltage-sensor of the channel and stabilize the complex in the resting state (Wisedchaisri et al. 2021). This and other cryo-EM structures of the toxin-channel complexes may be extremely useful in guiding AI-based drug design (Lau et al. 2018).
Still the programs today are unable to routinely deliver accurate docking configurations of channel-toxin complexes without applying multiple restrictions and boundary conditions, which require prior structural knowledge or assumptions (Gordon et al. 2013). Lacking these prevents true in silico high-throughput screening of toxins due to the high number of possible docking orientations and the consequent high computing costs. NMR measurements can supply interatomic distances for channel-toxin complexes, but these represent ensemble averages possibly originating from distinct gating conformations. Toxin pore blockers that bind by inserting a lysine or arginine side chain into the pore are easier to model, since this imposes many restrictions on the possible orientations thereby greatly reducing their number and thus the computing demand. For the same reason both the channel and the toxin may be modeled as rigid structures as in the lock and key model, but the induced fit model considering the flexibility of both partners is the more realistic description of the interaction requiring more computing power.
As appealing as it may sound, machine learning algorithms also require large amounts of experimental input data of known ligand-receptor interactions. Currently the PDB database contains the high-resolution structure of over 1000 membrane proteins, of which more than 300 belong to ion channels (Fernandez-Ballester et al. 2020). While numerous peptide toxin—ion channel docking interactions have already been published, the data quantity is likely to be only a small fraction of what would be required for efficient pattern recognition by neuronal network-based deep learning techniques (Mak and Pichika 2019). Thus, the highly promising prospects of AI in developing peptide toxin-based drugs currently seems to be limited by the shortage of experimental input data and the time-consuming experimental verification of in silico predictions.
As explained above, one possibility to create novel molecules for targeting ion channels is to understand the molecular interactions leading to the high affinity and specificity binding of inhibitors to the channels. Although these approaches resulted in several high affinity inhibitors of Kv1.3, finding novel inhibitors with unique properties is time consuming and is limited, among others, by the amount of toxins that can be isolated from the venoms. This obstacle can be circumvented by creating a scaffold-based/target-biased library and a high-throughput selection strategy, introduced into the development of Kv1.3 inhibitors by Takacs et al. in 2009 (Takacs et al. 2009). This technology is based on the selection of a peptide scaffold, in this case the scaffold of the α-KTx toxins (Miller 1995; Rodriguez de la Vega and Possani 2004), and applying the phage-display technology (Fig. 2) for targeting ion channels (Li 1997). Using this method, and applying the restrictions derived from the basic scaffold of the peptides, the authors generated 11,200 toxin variants in a combination library. Phages expressing the peptides were sorted based on high affinity binding to an immobilized ion channel construct (Kv1.3 pore domain grafted to the bacterial KcsA K+ channel). As a result, they have identified a novel toxin, called Mokatoxin-1 (referring to the Hungarian word “móka” which translates to English “fun”) constructed from the combination of Ce3 toxin (P0C163, α-2.10), AgTx2 (P46111 α-3.2) and ChTX P13487 α-1.1). The novel peptide has nanomolar affinity for Kv1.3 (Kd ~ 1 nM) and displays more than 1000-fold and 620-fold selectivity for Kv1.3 over Kv1.1 and Kv1.2, respectively. Thus, this novel, high throughput technique allows the isolation of novel, high affinity blockers of ion channels. The strategy was used to create peptide toxins targeting the bacterial KcsA K+ channel (Zhao et al. 2015) and the development of the high affinity inhibitor of the human voltage-gated proton channel, hHv1, Corza6 (C6) (Zhao et al. 2018).
Efforts to increase plasma lifetime of the peptides: conjugation to antibodies, PEGylation and nanocomplex formation
Peptide toxins are ~ 4000 Da peptides therefore they have very short half-life, e.g., ~ 50 min. in Lewis rats upon a single dose of 50 µg/kg for SHK(L5) administered subcutaneously (Beeton et al. 2005) [our knowledge of the plasma half-life of Dalazatide in humans is limited (Tarcha et al. 2017)]. The short half-life poses a significant limitation to the therapeutic application of peptides. In order to increase the plasma lifetime of peptide toxins several innovative strategies were used recently. One of these is to create a Kv1.3 targeting antibody. This was engineered by grafting the selective Kv1.3 blocker, Vm24, into the ultralong complementary determining region of a humanized bovine antibody (Synagis), resulting in Syn-Vm24-CDR3L (Wang et al. 2016). The grafting resulted in a significant improvement in the stability as compared to the Vm24 peptide (84% of the antibody remained intact versus the recorded 52% in case of the pure Vm24 in rat serum after 72 h incubation) and even if the affinity of the Syn-Vm24-CDR3L was decreased approximately 200-fold as compared to Vm24 (IC50 = 0.59 nM vs. ~ 0.003 nM) it still remained potent in sub-nanomolar concentrations and showed high selectivity against human effector memory T-cells, in which KV1.3 is the predominant potassium channel. Another potent selective Kv1.3 blocker, HsTx1[R14A], the analogue of HsTx1, was also engineered recently by PEGylation (Tanner et al. 2017) as well as Poly(Lactic-co-Glycolic Acid) (PLGA) microsphere formulation (Jin et al. 2020) to improve the pharmacokinetic parameters with retained selectivity and biological effects. PEGylation was achieved by conjugating the toxin with an activated 30kD monomethoxy-PEG-aldehyde and it resulted in a 1300-fold decrease in affinity as compared to the pure HsTx1[R14A] resulting an IC50 of 35.9 ± 6.3 nM (vs. the IC50 = 27 ± 9 pM for the pure toxin) which is still reasonable. The selectivity was not altered as a consequence of PEGylation and the (rat) serum half-life was dramatically increased to 37.3 h (vs. the less than 1 h in case of pure toxin) and it was still present in detectable concentrations for 14 days (Tanner et al. 2017). This increased half-life permits a less frequent, weekly administration of PEG-HsTx1[R14A]. Contrary to the covalent modifications above, PLGA (Poly(Lactic-co-Glycolic Acid) microsphere formulation of HsTx1[R14A] means the encapsulation of the toxin molecules into an emulsion system, resulting microspheres in the size-range of several µm depending on the applied PLGA materials. Subcutaneous administration of the toxin-loaded PLGA-RG503H microspheres in rats caused a relatively rapid burst release of HsTx1[R14A]; however, it provided detectable plasma concentrations well above the therapeutic level for up to 11 days compared to the ~ 8 h for subcutaneous administration of the non-formulated toxin (Jin et al. 2020).
Outlook
Peptide blockers of Kv1.3 seem to be promising therapeutic tools in the management of autoimmune diseases. A significant body of knowledge has been assembled already about native and rational drug design-guided/engineered toxins that are inhibiting Kv1.3 with high affinity and specificity. Novel techniques, such as phage display and AI-guided drug design is utilized to produce new, and possibly better Kv1.3 inhibitors. Conjugation of the peptides to carriers or incorporating them into microspheres improves the plasma residency time of the peptides. However, several questions remain to be addressed. One of the key questions is the off-target effect of the Kv1.3 inhibitors. Originally, the tissue distribution of Kv1.3 was reported to be very limited, mostly in immune cells and in the central nervous system (Panyi et al. 2004b). This limited tissue distribution of Kv1.3 is challenged by multiple studies indicating the expression of Kv1.3 in human vascular smooth muscle cells (Cidad et al. 2015), and in a variety of cancers (reviewed in (Teisseyre et al. 2019)). The consequences of Kv1.3 expression in these cells must be evaluated and the potential side-effects need to be minimized using, for example, targeted drug delivery (Tesauro et al. 2019). Another challenging field is the design of peptides that penetrate the blood brain barrier (BBB) to reach the central nervous system, which may be desirable in the Kv1.3-based prevention of relapses in multiple sclerosis where the BBB might still be a barrier for drug penetration (Lund et al. 2013). BBB penetration of the toxins may also be crucial to target Kv1.3 expressed in microglia in neurodegenerative diseases, such as Alzheimer’s disease, Parkinson’s disease and in chemically-induced status epilepticus seizures [reviewed recently in Tajti et al. (2020)]. In line with these, several strategies were developed to shuttle peptides across the BBB that include the conjugation to cell penetrating peptides or targeting membrane transporters (Oller-Salvia et al. 2016; Sanchez-Navarro et al. 2017).
References
Asuncion XE, Sampaco A-RB, Adorna H, Magadia J, BoÒgolan VP, Lluisma A (2019) Predicting the molecular targets of conopeptides by using principal component analysis and multiclass logistic regression philippine. J Sci 148:237–245
Bartok A, Fehér K, Bodor A, Rákosi K, Tóth GK, Kövér KE, Panyi G, Varga Z (2015a) An engineered scorpion toxin analogue with improved Kv1.3 selectivity displays reduced conformational flexibility. Sci. Rep. 5:18397. https://doi.org/10.1038/srep18397
Bartok A, Panyi G, Varga Z (2015b) Potassium channel blocking peptide toxins from scorpion venom. In: Gopalakrishnakone P, Possani L, Schwartz EF, de la Vega RR (eds) Scorpion venoms, vol 4. Springer, Dordrecht, pp 493–527
Beeton C, Pennington MW, Wulff H, Singh S, Nugent D, Crossley G, Khaytin I, Calabresi PA, Chen CY, Gutman GA, Chandy KG (2005) Targeting effector memory T cells with a selective peptide inhibitor of Kv1.3 channels for therapy of autoimmune diseases. Mol Pharmacol 67:1369–1381
Cahalan MD, Chandy KG (2009) The functional network of ion channels in T lymphocytes. Immunol Rev 231:59–87. https://doi.org/10.1111/j.1600-065X.2009.00816.x
Chandy KG, Decoursey TE, Cahalan MD, McLaughlin C, Gupta S (1984) Voltage-gated potassium channels are required for human T lymphocyte activation. J Exp Med 160:369–385
Chandy KG, Norton RS (2017) Peptide blockers of Kv1.3 channels in T cells as therapeutics for autoimmune disease. Curr Opin Chem Biol 38:97–107. https://doi.org/10.1016/j.cbpa.2017.02.015
Chi V, Pennington MW, Norton RS, Tarcha EJ, Londono LM, Sims-Fahey B, Upadhyay SK, Lakey JT, Iadonato S, Wulff H, Beeton C, Chandy KG (2012) Development of a sea anemone toxin as an immunomodulator for therapy of autoimmune diseases. Toxicon 59:529–546
Chiang EY, Li T, Jeet S, Peng I, Zhang J, Lee WP, DeVoss J, Caplazi P, Chen J, Warming S, Hackos DH, Mukund S, Koth CM, Grogan JL (2017) Potassium channels Kv1.3 and KCa3.1 cooperatively and compensatorily regulate antigen-specific memory T cell functions. Nat Commun 8:14644. https://doi.org/10.1038/ncomms14644
Chighizola CB, Ong VH, Meroni PL (2017) The use of cyclosporine A in rheumatology: a 2016 comprehensive review. Clin Rev Allergy Immunol 52:401–423. https://doi.org/10.1007/s12016-016-8582-3
Cidad P, Miguel-Velado E, Ruiz-McDavitt C, Alonso E, Jimenez-Perez L, Asuaje A, Carmona Y, Garcia-Arribas D, Lopez J, Marroquin Y, Fernandez M, Roque M, Perez-Garcia MT, Lopez-Lopez JR (2015) Kv1.3 channels modulate human vascular smooth muscle cells proliferation independently of mTOR signaling pathway. Pflugers Arch 467:1711–1722. https://doi.org/10.1007/s00424-014-1607-y
Diochot S, Drici MD, Moinier D, Fink M, Lazdunski M (1999) Effects of phrixotoxins on the Kv4 family of potassium channels and implications for the role of Ito1 in cardiac electrogenesis. Br J Pharmacol 126:251–263. https://doi.org/10.1038/sj.bjp.0702283
Fernandez-Ballester G, Fernandez-Carvajal A, Ferrer-Montiel A (2020) Targeting thermo TRP ion channels: in silico preclinical approaches and opportunities. Expert Opin Ther Targets 24:1079–1097. https://doi.org/10.1080/14728222.2020.1820987
Feske S, Prakriya M, Rao A, Lewis RS (2005) A severe defect in CRAC Ca2+ channel activation and altered K+ channel gating in T cells from immunodeficient patients. J Exp Med 202:651–662
Feske S, Skolnik EY, Prakriya M (2012) Ion channels and transporters in lymphocyte function and immunity. Nat Rev Immunol 12:532–547. https://doi.org/10.1038/nri3233
Feske S, Wulff H, Skolnik EY (2015) Ion channels in innate and adaptive immunity. Annu Rev Immunol 33:291–353. https://doi.org/10.1146/annurev-immunol-032414-112212
Gordon D, Chen R, Chung SH (2013) Computational methods of studying the binding of toxins from venomous animals to biological ion channels: theory and applications. Physiol Rev 93:767–802. https://doi.org/10.1152/physrev.00035.2012
Gurrola GB, Hernandez-Lopez RA, Rodriguez de la Vega RC, Varga Z, Batista CV, Salas-Castillo SP, Panyi G, del Rio-Portilla F, Possani LD (2012) Structure, function, and chemical synthesis of Vaejovis mexicanus peptide 24: a novel potent blocker of Kv1.3 potassium channels of human T lymphocytes. Biochemistry 51:4049–4061. https://doi.org/10.1021/bi300060n
Halloran PF (2004) Immunosuppressive drugs for kidney transplantation. N Engl J Med 351:2715–2729. https://doi.org/10.1056/NEJMra033540
Jin L, Pan Y, Pham AC, Boyd BJ, Norton RS, Nicolazzo JA (2020) Prolonged plasma exposure of the Kv1.3-inhibitory peptide HsTX1[R14A] by subcutaneous administration of a poly(lactic-co-glycolic acid) (PLGA) microsphere formulation. J Pharm Sci. https://doi.org/10.1016/j.xphs.2020.10.014
Kaas Q, Craik DJ (2015) Bioinformatics-aided venomics. Toxins (Basel) 7:2159–2187. https://doi.org/10.3390/toxins7062159
Kalman K, Pennington MW, Lanigan MD, Nguyen A, Rauer H, Mahnir V, Paschetto K, Kem WR, Grissmer S, Gutman GA, Christian EP, Cahalan MD, Norton RS, Chandy KG (1998) ShK-Dap22, a potent Kv1.3-specific immunosuppressive polypeptide. J Biol Chem 273:32697–32707
Kim JH, Perfect JR (1989) Infection and cyclosporine. Rev Infect Dis 11:677–690. https://doi.org/10.1093/clinids/11.5.677
Kundu-Raychaudhuri S, Chen YJ, Wulff H, Raychaudhuri SP (2014) Kv1.3 in psoriatic disease: PAP-1, a small molecule inhibitor of Kv1.3 is effective in the SCID mouse psoriasis–xenograft model. J Autoimmun 55:63–72. https://doi.org/10.1016/j.jaut.2014.07.003
Lallana EC, Fadul CE (2011) Toxicities of immunosuppressive treatment of autoimmune neurologic diseases. Curr Neuropharmacol 9:468–477. https://doi.org/10.2174/157015911796557939
Lau C, Hunter MJ, Stewart A, Perozo E, Vandenberg JI (2018) Never at rest: insights into the conformational dynamics of ion channels from cryo-electron microscopy. J Physiol 596:1107–1119. https://doi.org/10.1113/JP274888
Lebrun B, Romi-Lebrun R, Martin-Eauclaire MF, Yasuda A, Ishiguro M, Oyama Y, Pongs O, Nakajima T (1997) A four-disulphide-bridged toxin, with high affinity towards voltage-gated K+ channels, isolated from Heterometrus spinnifer (Scorpionidae) venom. Biochem J 328(Pt 1):321–327
Legany N, Toldi G, Orban C, Megyes N, Bajnok A, Balog A (2016) Calcium influx kinetics, and the features of potassium channels of peripheral lymphocytes in primary Sjogren’s syndrome. Immunobiology 221:1266–1272. https://doi.org/10.1016/j.imbio.2016.06.004
Li M (1997) Use of a modified bacteriophage to probe the interactions between peptides and ion channel receptors in mammalian cells. Nat Biotechnol 15:559–563. https://doi.org/10.1038/nbt0697-559
Lund H, Krakauer M, Skimminge A, Sellebjerg F, Garde E, Siebner HR, Paulson OB, Hesse D, Hanson LG (2013) Blood-brain barrier permeability of normal appearing white matter in relapsing-remitting multiple sclerosis. PLoS ONE 8:e56375. https://doi.org/10.1371/journal.pone.0056375
Mak KK, Pichika MR (2019) Artificial intelligence in drug development: present status and future prospects. Drug Discov Today 24:773–780. https://doi.org/10.1016/j.drudis.2018.11.014
Matteson DR, Deutsch C (1984) K channels in T lymphocytes: a patch clamp study using monoclonal antibody adhesion. Nature 307:468–471
Matthies D, Bae C, Toombes GE, Fox T, Bartesaghi A, Subramaniam S, Swartz KJ (2018) Single-particle cryo-EM structure of a voltage-activated potassium channel in lipid nanodiscs. Elife 7:e37558. https://doi.org/10.7554/eLife.37558
Middleton RE, Warren VA, Kraus RL, Hwang JC, Liu CJ, Dai G, Brochu RM, Kohler MG, Gao YD, Garsky VM, Bogusky MJ, Mehl JT, Cohen CJ, Smith MM (2002) Two tarantula peptides inhibit activation of multiple sodium channels. Biochemistry 41:14734–14747. https://doi.org/10.1021/bi026546a
Miller C (1995) The charybdotoxin family of K+-channel-blocking peptides. Neuron 15:5–10
Mouhat S, Visan V, Ananthakrishnan S, Wulff H, Andreotti N, Grissmer S, Darbon H, De Waard M, Sabatier JM (2005) K+ channel types targeted by synthetic OSK1, a toxin from Orthochirus scrobiculosus scorpion venom. Biochem J 385:95–104
Mullard A (2019) 2018 FDA drug approvals. Nat Rev Drug Discov 18:85–89. https://doi.org/10.1038/d41573-019-00014-x
Nguyen HM, Grossinger EM, Horiuchi M, Davis KW, Jin LW, Maezawa I, Wulff H (2017) Differential Kv1.3, KCa3.1, and Kir2.1 expression in “classically” and “alternatively” activated microglia. Glia 65:106–121. https://doi.org/10.1002/glia.23078
Norton RS, Chandy KG (2017) Venom-derived peptide inhibitors of voltage-gated potassium channels. Neuropharmacology 127:124–138. https://doi.org/10.1016/j.neuropharm.2017.07.002
Oller-Salvia B, Sanchez-Navarro M, Giralt E, Teixido M (2016) Blood-brain barrier shuttle peptides: an emerging paradigm for brain delivery. Chem Soc Rev 45:4690–4707. https://doi.org/10.1039/c6cs00076b
Orlicka K, Barnes E, Culver EL (2013) Prevention of infection caused by immunosuppressive drugs in gastroenterology. Ther Adv Chronic Dis 4:167–185. https://doi.org/10.1177/2040622313485275
Panyi G, Vamosi G, Bodnar A, Gaspar R Jr, Damjanovich S (2004a) Looking through ion channels: recharged concepts in T cell signaling. Trends Immunol 25:565–569
Panyi G, Varga Z, Gaspar R (2004b) Ion channels and lymphocyte activation. Immunol Lett 92:55–66
Panyi G, Possani LD, Rodriguez de la Vega RC, Gaspar R, Varga Z (2006) K+ channel blockers: novel tools to inhibit T cell activation leading to specific immunosuppression. Curr Pharm Des 12:2199–2220
Pennington MW, Beeton C, Galea CA, Smith BJ, Chi V, Monaghan KP, Garcia A, Rangaraju S, Giuffrida A, Plank D, Crossley G, Nugent D, Khaytin I, Lefievre Y, Peshenko I, Dixon C, Chauhan S, Orzel A, Inoue T, Hu X, Moore RV, Norton RS, Chandy KG (2009) Engineering a stable and selective peptide blocker of the Kv1.3 channel in T lymphocytes. Mol Pharmacol 75:762–773
Rangaraju S, Gearing M, Jin LW, Levey A (2015) Potassium channel Kv1.3 is highly expressed by microglia in human Alzheimer’s disease. J Alzheimers Dis 44:797–808. https://doi.org/10.3233/JAD-141704
Rashid MH, Huq R, Tanner MR, Chhabra S, Khoo KK, Estrada R, Dhawan V, Chauhan S, Pennington MW, Beeton C, Kuyucak S, Norton RS (2014) A potent and Kv1.3-selective analogue of the scorpion toxin HsTX1 as a potential therapeutic for autoimmune diseases. Sci Rep 4:4509. https://doi.org/10.1038/srep04509
Rodriguez de la Vega RC, Possani LD (2004) Current views on scorpion toxins specific for K+-channels. Toxicon 43:865–875
Sanchez-Navarro M, Teixido M, Giralt E (2017) Jumping hurdles: peptides able to overcome biological barriers. Acc Chem Res 50:1847–1854. https://doi.org/10.1021/acs.accounts.7b00204
Schreiber SL, Crabtree GR (1992) The mechanism of action of cyclosporin A and FK506. Immunol Today 13:136–142. https://doi.org/10.1016/0167-5699(92)90111-J
Serrano-Albarras A, Cirera-Rocosa S, Sastre D, Estadella I, Felipe A (2019) Fighting rheumatoid arthritis: Kv1.3 as a therapeutic target. Biochem Pharmacol 165:214–220. https://doi.org/10.1016/j.bcp.2019.03.016
Smietana K, Siatkowski M, Moller M (2016) Trends in clinical success rates. Nat Rev Drug Discov 15:379–380. https://doi.org/10.1038/nrd.2016.85
Stauderman KA (2018) CRAC channels as targets for drug discovery and development. Cell Calcium 74:147–159. https://doi.org/10.1016/j.ceca.2018.07.005
Tajti G, Wai DCC, Panyi G, Norton RS (2020) The voltage-gated potassium channel KV1.3 as a therapeutic target for venom-derived peptides. Biochem Pharmacol. https://doi.org/10.1016/j.bcp.2020.114146
Takacs Z, Toups M, Kollewe A, Johnson E, Cuello LG, Driessens G, Biancalana M, Koide A, Ponte CG, Perozo E, Gajewski TF, Suarez-Kurtz G, Koide S, Goldstein SA (2009) A designer ligand specific for Kv1.3 channels from a scorpion neurotoxin-based library. Proc Natl Acad Sci USA 106:22211–22216
Tanner MR, Tajhya RB, Huq R, Gehrmann EJ, Rodarte KE, Atik MA, Norton RS, Pennington MW, Beeton C (2017) Prolonged immunomodulation in inflammatory arthritis using the selective Kv1.3 channel blocker HsTX1[R14A] and its PEGylated analog. Clin Immunol 180:45–57. https://doi.org/10.1016/j.clim.2017.03.014
Tarcha EJ, Olsen CM, Probst P, Peckham D, Munoz-Elias EJ, Kruger JG, Iadonato SP (2017) Safety and pharmacodynamics of dalazatide, a Kv1.3 channel inhibitor, in the treatment of plaque psoriasis: a randomized phase 1b trial. PLoS ONE 12:e0180762. https://doi.org/10.1371/journal.pone.0180762
Teisseyre A, Palko-Labuz A, Sroda-Pomianek K, Michalak K (2019) Voltage-gated potassium channel Kv1.3 as a target in therapy of cancer. Front Oncol 9:933. https://doi.org/10.3389/fonc.2019.00933
Tesauro D, Accardo A, Diaferia C, Milano V, Guillon J, Ronga L, Rossi F (2019) Peptide-based drug-delivery systems in biotechnological applications: recent advances and perspectives. Molecules. https://doi.org/10.3390/molecules24020351
Varga Z, Hajdu P, Panyi G (2010) Ion channels in T lymphocytes: an update on facts, mechanisms and therapeutic targeting in autoimmune diseases. Immunol Lett 130:19–25. https://doi.org/10.1016/j.imlet.2009.12.015
Varga Z, Gurrola-Briones G, Papp F, Rodriguez de la Vega RC, Pedraza-Alva G, Tajhya RB, Gaspar R, Cardenas L, Rosenstein Y, Beeton C, Possani LD, Panyi G (2012) Vm24, a natural immunosuppressive peptide, potently and selectively blocks Kv1.3 potassium channels of human T cells. Mol Pharmacol 82:372–382. https://doi.org/10.1124/mol.112.078006
Vennekamp J, Wulff H, Beeton C, Calabresi PA, Grissmer S, Hansel W, Chandy KG (2004) Kv1.3-blocking 5-phenylalkoxypsoralens: a new class of immunomodulators. Mol Pharmacol 65:1364–1374
Wang RE, Wang Y, Zhang Y, Gabrelow C, Zhang Y, Chi V, Fu Q, Luo X, Wang D, Joseph S, Johnson K, Chatterjee AK, Wright TM, Nguyen-Tran VT, Teijaro J, Theofilopoulos AN, Schultz PG, Wang F (2016) Rational design of a Kv1.3 channel-blocking antibody as a selective immunosuppressant. Proc Natl Acad Sci USA 113:11501–11506. https://doi.org/10.1073/pnas.1612803113
Wisedchaisri G, Tonggu L, El-Din TMG, McCord E, Zeng N, Catterall WA (2021) Structural basis for high-affinity trapping of the NaV1.7 channel in its resting state by tarantula toxin. Mol Cell 81:1–11. https://doi.org/10.1016/j.molcel.2020.10.039
Wulff H, Calabresi PA, Allie R, Yun S, Pennington M, Beeton C, Chandy KG (2003) The voltage-gated Kv1.3 K+ channel in effector memory T cells as new target for MS. J Clin Invest 111:1703–1713
Wulff H, Castle NA, Pardo LA (2009) Voltage-gated potassium channels as therapeutic targets. Nat Rev Drug Discov 8:982–1001. https://doi.org/10.1038/nrd2983
Zhao R, Dai H, Mendelman N, Cuello LG, Chill JH, Goldstein SA (2015) Designer and natural peptide toxin blockers of the KcsA potassium channel identified by phage display. Proc Natl Acad Sci USA 112:E7013-7021. https://doi.org/10.1073/pnas.1514728112
Zhao R, Kennedy K, De Blas GA, Orta G, Pavarotti MA, Arias RJ, de la Vega-Beltran JL, Li Q, Dai H, Perozo E, Mayorga LS, Darszon A, Goldstein SAN (2018) Role of human Hv1 channels in sperm capacitation and white blood cell respiratory burst established by a designed peptide inhibitor. Proc Natl Acad Sci USA 115:E11847–E11856. https://doi.org/10.1073/pnas.1816189115
Funding
Open Access funding provided by University of Debrecen. The publication is supported by the GINOP-2.3.2-15-2016-00015 project (G.T. and G.P). The project is co-financed by the European Union and the European Regional Development Fund. The authors acknowledge the support of OTKA K119417 (G.P.) and EFOP-3.6.2-16-2017-00006 (G.P.).
Author information
Authors and Affiliations
Contributions
Z.V, G.T and G.P were responsible for writing the manuscript. G.T was responsible for figures. G.P was responsible for conceptualization.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
Not applicable, our paper does not contain any experiments connected to humans or animals.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Varga, Z., Tajti, G. & Panyi, G. The Kv1.3 K+ channel in the immune system and its “precision pharmacology” using peptide toxins. BIOLOGIA FUTURA 72, 75–83 (2021). https://doi.org/10.1007/s42977-021-00071-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42977-021-00071-7