Abstract
Objects
The retrospective study aimed to determine the prevalence rate and antimicrobial susceptibility of extended-spectrum beta-lactamases (ESBLs)–producing Klebsiella pneumoniae and Escherichia coli in 2013–2017 at a single center in China.
Methods
Klebsiella pneumoniae and Escherichia coli data were collected from the microbiological laboratory. VITEK 2 compact system was used for the identification and antimicrobial susceptibility testing. ESBL status was determined as per the Clinical and Laboratory Standards Institute (CLSI) protocols microdilution method.
Results
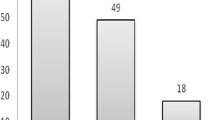
Among a total of 2774 strains of Klebsiella pneumoniae and 2154 strains of Escherichia coli, 15.79% and 36.86% were found to be ESBL producers, respectively. In all patients infected by ESBLs-producing strains, those over 60 years accounted for the largest proportion. Infection by ESBLs-producing Klebsiella pneumoniae was more common in male, while that by ESBLs-producing Escherichia coli was more common in female. Urine and respiratory secretions were the most common sources of ESBLs-producing strains; however, ESBLs-producing strains from urine had been significantly declined. No carbapenem-resistant isolate was found, and all ESBLs-producing strains were resistant to ceftriaxone, aztreonam, and piperacillin. There were no differences in resistance rates between ESBLs-producing Escherichia coli and Klebsiella pneumoniae to ceftazidime and cefepime; however, ESBLs-producing Klebsiella pneumoniae showed higher resistance rates to piperacillin/tazobactam, amikacin, gentamicin, and co-trimoxazole compared with ESBLs-producing Escherichia coli.
Conclusion
Different ESBLs-producing organisms have their own epidemiological characteristics, and the resistance of ESBLs-producing Klebsiella pneumoniae and Escherichia coli is different even to the same antibiotics. Therefore, it is important to continuously monitor the status of ESBLs-producing organisms, and an improved antimicrobial stewardship and infection control are much required.



Similar content being viewed by others
References
Leylabadlo HE, Kafil HS, Yousefi M, Aghazadeh M, Asgharzadeh M (2016) Persistent infection with metallo-beta-lactamase and extended spectrum beta-lactamase producer Morganella morganii in a patient with urinary tract infection after kidney transplantation. J Nat Sci, Biol Med 7(2):179–181. https://doi.org/10.4103/0976-9668.184707
Paterson DL, Bonomo RA (2005) Extended-spectrum beta-lactamases: a clinical update. Clin Microbiol Rev 18(4):657–65+. https://doi.org/10.1128/Cmr.18.4.657-686.2005
Mehdipour Moghaddam MJ, Mirbagheri AA, Salehi Z, Habibzade SM (2015) Prevalence of class 1 Integrons and extended spectrum beta lactamases among multi-drug resistant Escherichia coli isolates from north of Iran. Iran Biomed J 19(4):233–239
Jean SS, Coombs G, Ling T, Balaji V, Rodrigues C, Mikamo H, Kim MJ, Rajasekaram DG, Mendoza M, Tan TY, Kiratisin P, Ni Y, Weinman B, Xu Y, Hsueh PR Epidemiology and antimicrobial susceptibility profiles of pathogens causing urinary tract infections in the Asia-Pacific region: results from the Study for Monitoring Antimicrobial Resistance Trends (SMART), 2010-2013. Int J Antimicrob Ag 2016;47(4):328–334 doi: https://doi.org/10.1016/j.ijantimicag.2016.01.008
Zhang H, Yang Q, Liao K, Ni Y, Yu Y, Hu B, Sun Z, Huang W, Wang Y, Wu A, Feng X, Luo Y, Chu Y, Chen S, Cao B, Su J, Duan Q, Zhang S, Shao H, Kong H, Gui B, Hu Z, Badal R, Xu Y (2017) Update of incidence and antimicrobial susceptibility trends of Escherichia coli and Klebsiella pneumoniae isolates from Chinese intra-abdominal infection patients. BMC Infect Dis 17(1):776. https://doi.org/10.1186/s12879-017-2873-z
Institute CaLS.2013 Performance standards for antimicrobial susceptibility testing; twenty-third informational supplement. CLSI document M100-S23. Wayne, PA
Institute CaLS. 2014 Performance standards for antimicrobial susceptibility testing; twenty-fourth informational supplement. CLSI document M100-S24. Wayne, PA
Institute CaLS. 2015Performance standards for antimicrobial susceptibility testing; twenty-fifth informational supplement. CLSI document M100-S25. Wayne, PA
Institute CaLS.2016 Performance standards for antimicrobial susceptibility testing,26th Edition. CLSI document M100S. Wayne, PA
Institute CaLS.2017 Performance standards for antimicrobial susceptibility testing; 27th Edition. CLSI document M100S. Wayne, PA.,
Fupin Hu, Demei Zhu, Fu Wang,et al. CHINET surveillance of bacterial resistance across China: report of the results in 2016. Chin J Infect Chemother 2016;17(5):481–491
Hu F, Wang F, Jiang X et al (2015) Report of CHINET antimicrobial resistance surveillance program in 2015. Chin J Infect Chemother 16(6):685–694
Hu F, Wang F, Jiang X et al (2014) CHINET 2014 surveillance of bacterial resistance in China. Chin J Infect Chemother 15(5):401–410
Hu F, Wang F, Jiang X et al (2013) CHINET 2013 surveillance of bacterial resistance in China. Chin J Infect Chemother 14(5):369–378
Zhang H, Yang Q, Liao K, Ni Y, Yu Y, Hu B, Sun Z, Huang W, Wang Y, Wu A, Feng X, Luo Y, Hu Z, Chu Y, Chen S, Cao B, Su J, Gui B, Duan Q, Zhang S, Shao H, Kong H, Badal RE, Xu Y (2016) Antimicrobial susceptibilities of aerobic and facultative gram-negative bacilli from intra-abdominal infections in patients from seven regions in China in 2012 and 2013. Antimicrob Agents Chemother 60(1):245–251. https://doi.org/10.1128/AAC.00956-15
Rodriguez-Bano J, Alcala JC, Cisneros JM, et al. Community infections caused by extended-spectrum beta-lactamase-producing Escherichia coli. Arch Intern Med 2008;168(17):1897–1902 doi: DOI https://doi.org/10.1001/archinte.168.17.1897
Canton R, Novais A, Valverde A et al (2008) Prevalence and spread of extended-spectrum beta-lactamase-producing Enterobacteriaceae in Europe. Clin Microbiol Infect: Off Publ Eur Soc Clin Microbiol Infect Dis 14(Suppl 1):144–153. https://doi.org/10.1111/j.1469-0691.2007.01850.x
Krause KM, Serio AW, Kane TR, Connolly LE (2016) Aminoglycosides: an overview. Cold Spring Harbor Perspect Med 6(6). https://doi.org/10.1101/cshperspect.a027029
Eftekhar FP, Seyedpour SMM (2015) Prevalence of qnr and aac(6′)-Ib-cr Genes in clinical isolates of Klebsiella Pneumoniae from Imam Hussein Hospital in Tehran. Iranian J Med Sci 40(6):515–521
Ho PL, Leung LM, Chow KH, Lai EL, Lo WU, Ng TK (2016) Prevalence of aminoglycoside modifying enzyme and 16S ribosomal RNA methylase genes among aminoglycoside-resistant Escherichia coli isolates. J Microbiol, Immunol Infect= Wei mian yu gan ran za zhi 49(1):123–126. https://doi.org/10.1016/j.jmii.2014.08.012
Du XD, Li DX, Hu GZ et al (2012) Tn1548-associated armA is co-located with qnrB2, aac(6′)-Ib-cr and blaCTX-M-3 on an IncFII plasmid in a Salmonella enterica subsp. enterica serovar Paratyphi B strain isolated from chickens in China. J Antimicrob Chemother 67(1):246–248. https://doi.org/10.1093/jac/dkr407
Robin F, Beyrouthy R, Bonacorsi S, Aissa N, Bret L, Brieu N, Cattoir V, Chapuis A, Chardon H, Degand N, Doucet-Populaire F, Dubois V, Fortineau N, Grillon A, Lanotte P, Leyssene D, Patry I, Podglajen I, Recule C, Ros A, Colomb-Cotinat M, Ponties V, Ploy MC, Bonnet R (2017) Inventory of extended-Spectrum-beta-lactamase-producing Enterobacteriaceae in France as assessed by a multicenter study. Antimicrob Agents Chemother 61(3). https://doi.org/10.1128/AAC.01911-16
Azargun R, Sadeghi MR, Soroush Barhaghi MH, Samadi Kafil H, Yeganeh F, Ahangar Oskouee M, Ghotaslou R (2018) The prevalence of plasmid-mediated quinolone resistance and ESBL-production in Enterobacteriaceae isolated from urinary tract infections. Infect Drug Resist 11:1007–1014. https://doi.org/10.2147/IDR.S160720
Wiener ES, ELH LMH, Kristie Johnson J (2016) Are fluoroquinolones appropriate for the treatment of extended-Spectrum β-lactamase-producing gram-negative bacilli? J Pharm Technol 32(1):16–21
Morrissey I, Hackel M, Badal R, Bouchillon S, Hawser S, Biedenbach D (2013) A review of ten years of the Study for Monitoring Antimicrobial Resistance Trends (SMART) from 2002 to 2011. Pharmaceuticals 6(11):1335–1346. https://doi.org/10.3390/ph6111335
Ponce-de-Leon A, Rodriguez-Noriega E, Morfin-Otero R et al (2018) Antimicrobial susceptibility of gram-negative bacilli isolated from intra-abdominal and urinary-tract infections in Mexico from 2009 to 2015: results from the Study for Monitoring Antimicrobial Resistance Trends (SMART). PLoS One 13(6):e0198621. https://doi.org/10.1371/journal.pone.0198621
Quan J, Zhao D, Liu L, Chen Y, Zhou J, Jiang Y, du X, Zhou Z, Akova M, Yu Y (2017) High prevalence of ESBL-producing Escherichia coli and Klebsiella pneumoniae in community-onset bloodstream infections in China. J Antimicrob Chemother 72(1):273–280. https://doi.org/10.1093/jac/dkw372
Xia S, Fan X, Huang Z, Xia L, Xiao M, Chen R, Xu Y, Zhuo C (2014) Dominance of CTX-M-type extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli isolated from patients with community-onset and hospital-onset infection in China. PLoS One 9(7):e100707. https://doi.org/10.1371/journal.pone.0100707
Chopra T, Marchaim D, Veltman J, Johnson P, Zhao JJ, Tansek R, Hatahet D, Chaudhry K, Pogue JM, Rahbar H, Chen TY, Truong T, Rodriguez V, Ellsworth J, Bernabela L, Bhargava A, Yousuf A, Alangaden G, Kaye KS (2012) Impact of cefepime therapy on mortality among patients with bloodstream infections caused by extended-spectrum-beta-lactamase-producing Klebsiella pneumoniae and Escherichia coli. Antimicrob Agents Chemother 56(7):3936–3942. https://doi.org/10.1128/AAC.05419-11
Acknowledgments
We thank Yanlei Li, a doctor of the laboratory medicine in the Second Hospital of Jilin University, for her imparting knowledge in the field of microbiology and the writing assistance.
Funding
This study was financially supported by the Science and Technology Agency of Jilin Province [grant number 201603034YY].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Responsible Editor: Afonso Barth
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, Y., Zhang, Q., Jin, Y. et al. Epidemiology and antimicrobial susceptibility profiles of extended-spectrum beta-lactamase–producing Klebsiella pneumoniae and Escherichiacoli in China. Braz J Microbiol 50, 669–675 (2019). https://doi.org/10.1007/s42770-019-00081-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42770-019-00081-7