Abstract
The role of gut microbiota in type 2 diabetes (T2D) has been investigated through many recent studies conducted in different parts of the globe. However, intrinsic differences in the gut microbiota related to geography, ethnicity, dietary preferences, etc. tend to confound the disease-associated differences and make the search for any universal T2D-specific signature a challenging task. The present work makes an attempt to identify population or sub-population specific consensus gut microbiota signatures of T2D with a particular focus on Asian-Indians, who are reported to exhibit a distinct T2D phenotype. In this process, the article reviews and summarizes different microbial genera that have been reported to be associated with T2D in earlier studies conducted in different geographies. The results indicate that while the taxonomic signatures of T2D-associated gut microbiota (i.e. the presence and abundance of particular genera) may vary between populations, their functional roles in context of T2D pathophysiology have more coherence. Furthermore, it appears that while the gut microbiota of T2D subjects from different geographies are characterized by a combination of depletion of beneficial/ commensal taxa as well as an enrichment of harmful, pro-inflammatory and infectious taxonomic groups, the latter phenomenon may be more prevalent in Asian-Indian T2D subjects.

Similar content being viewed by others
References
Deshpande AD, Harris-Hayes M, Schootman M (2008) Epidemiology of diabetes and diabetes-related complications. Phys Ther 88(11):1254–1264. https://doi.org/10.2522/ptj.20080020
Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J (2020) Epidemiology of type 2 diabetes—global burden of disease and forecasted trends. J Epidemiol Glob Health 10(1):107–111. https://doi.org/10.2991/jegh.k.191028.001
Lin X et al (2020) Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep 10:14790. https://doi.org/10.1038/s41598-020-71908-9
Singer ME, Dorrance KA, Oxenreiter MM, Yan KR, Close KL (2021) The type 2 diabetes ‘modern preventable pandemic’ and replicable lessons from the COVID-19 crisis. Prev Med Rep 25:101636. https://doi.org/10.1016/j.pmedr.2021.101636
Salis S, Anjana RM, Unnikrishnan R, Syed S, Mohan V (2022) Remission of type 2 diabetes: how, when, and for whom? J Physicians India Assoc. https://doi.org/10.5005/japi-11001-0078
Li W-Z, Stirling K, Yang J-J, Zhang L (2020) Gut microbiota and diabetes: From correlation to causality and mechanism. World J Diabetes. https://doi.org/10.4239/wjd.v11.i7.293
Gurung M et al (2020) Role of gut microbiota in type 2 diabetes pathophysiology. EBioMedicine. https://doi.org/10.1016/j.ebiom.2019.11.051
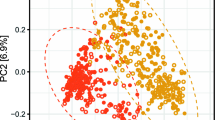
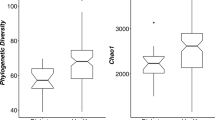
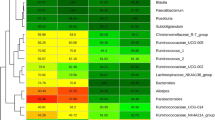
Alvarez-Silva C et al (2021) Trans-ethnic gut microbiota signatures of type 2 diabetes in Denmark and India. Genome Med 13(1):1–13
Pinna NK et al (2021) Trans-ethnic gut microbial signatures of prediabetic subjects from India and Denmark. Genome Med 13(1):1–20
Karlsson FH et al (2013) Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature. https://doi.org/10.1038/nature12198
Maskarinec G et al (2021) The gut microbiome and type 2 diabetes status in the multiethnic cohort. PLoS ONE. https://doi.org/10.1371/journal.pone.0250855
Dwiyanto J et al (2021) Ethnicity influences the gut microbiota of individuals sharing a geographical location: a cross-sectional study from a middle-income country. Sci Rep. https://doi.org/10.1038/s41598-021-82311-3
Borrello K et al (2022) Dietary intake mediates ethnic differences in gut microbial composition. Nutrients 14(3):660. https://doi.org/10.3390/nu14030660
Anjana RM et al (2020) Novel subgroups of type 2 diabetes and their association with microvascular outcomes in an Asian Indian population: a data-driven cluster analysis: the INSPIRED study. BMJ Open Diabetes Res Care. https://doi.org/10.1136/bmjdrc-2020-001506
Pasolli E et al (2017) Accessible, curated metagenomic data through ExperimentHub. Nat Methods. https://doi.org/10.1038/nmeth.4468
Beghini F et al (2021) Integrating taxonomic, functional, and strain-level profiling of diverse microbial communities with bioBakery 3. Elife 10:e65088. https://doi.org/10.7554/eLife.65088
Zhou W et al (2019) Longitudinal multi-omics of host-microbe dynamics in prediabetes. Nature. https://doi.org/10.1038/s41586-019-1236-x
Sankaranarayanan K et al (2015) Gut Microbiome diversity among cheyenne and arapaho individuals from Western Oklahoma. Curr Biol CB. https://doi.org/10.1016/j.cub.2015.10.060
Feng Q et al (2015) Gut microbiome development along the colorectal adenoma-carcinoma sequence. Nat Commun 6:6528. https://doi.org/10.1038/ncomms7528
Qin J et al (2012) A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 490(7418):55–60. https://doi.org/10.1038/nature11450
Yu J et al (2017) Metagenomic analysis of faecal microbiome as a tool towards targeted non-invasive biomarkers for colorectal cancer. Gut. https://doi.org/10.1136/gutjnl-2015-309800
Das T et al (2021) Alterations in the gut bacterial microbiome in people with type 2 diabetes mellitus and diabetic retinopathy. Sci Rep. https://doi.org/10.1038/s41598-021-82538-0
Talukdar R et al (2021) The gut microbiome in pancreatogenic diabetes differs from that of Type 1 and Type 2 diabetes. Sci Rep. https://doi.org/10.1038/s41598-021-90024-w
Gaike AH et al (2020) The gut microbial diversity of newly diagnosed diabetics but not of prediabetics is significantly different from that of healthy nondiabetics. Systems. https://doi.org/10.1128/mSystems.00578-19
Bhute SS, Suryavanshi MV, Joshi SM, Yajnik CS, Shouche YS, Ghaskadbi SS (2017) Gut microbial diversity assessment of Indian type-2-diabetics reveals alterations in eubacteria, archaea, and eukaryotes. Front Microbiol 8:214. https://doi.org/10.3389/fmicb.2017.00214
Jumas-Bilak E et al (2007) Acidaminococcus intestini sp. Nov., isolated from human clinical samples. Int J Syst Evol Microbiol. https://doi.org/10.1099/ijs.0.64883-0
Singh SB, Lin HC (2015) Hydrogen sulfide in physiology and diseases of the digestive tract. Microorganisms 3(4):866–889. https://doi.org/10.3390/microorganisms3040866
Murros KE, Huynh VA, Takala TM, Saris PEJ (2021) Desulfovibrio bacteria are associated with Parkinson’s disease. Front Cell Infect Microbiol 11:652617. https://doi.org/10.3389/fcimb.2021.652617
Sanjiwani MID, Aryadi IPH, Semadi IMS (2022) Review of literature on akkermansia muciniphila and its possible role in the etiopathogenesis and therapy of type 2 diabetes mellitus. J ASEAN Fed Endocr Soc 37(1):69–74. https://doi.org/10.15605/jafes.037.01.13
Karlsson CLJ, Onnerfält J, Xu J, Molin G, Ahrné S, Thorngren-Jerneck K (2012) The microbiota of the gut in preschool children with normal and excessive body weight. Obes Silver Spring Md. https://doi.org/10.1038/oby.2012.110
Adeshirlarijaney A, Gewirtz AT (2020) Considering gut microbiota in treatment of type 2 diabetes mellitus. Gut Microbes. https://doi.org/10.1080/19490976.2020.1717719
Doumatey AP et al (2020) Gut microbiome profiles are associated with type 2 diabetes in urban Africans. Front Cell Infect Microbiol 10:63. https://doi.org/10.3389/fcimb.2020.00063
Zeevi D et al (2019) Structural variation in the gut microbiome associates with host health. Nature. https://doi.org/10.1038/s41586-019-1065-y
Wu GD et al (2011) Linking long-term dietary patterns with gut microbial enterotypes. Science. https://doi.org/10.1126/science.1208344
Yoshida N et al (2018) Bacteroides vulgatus and Bacteroides dorei reduce gut microbial lipopolysaccharide production and inhibit atherosclerosis. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.118.033714
Liu X et al (2022) Blautia—a new functional genus with potential probiotic properties? Gut Microbes. https://doi.org/10.1080/19490976.2021.1875796
Tong X et al (2018) Structural alteration of gut microbiota during the amelioration of human type 2 diabetes with hyperlipidemia by metformin and a traditional Chinese herbal formula: a multicenter, randomized, open label clinical trial. MBio 9(3):e02392-e2417. https://doi.org/10.1128/mBio.02392-17
Jia W et al (2012) Diversity and distribution of sulphate-reducing bacteria in human faeces from healthy subjects and patients with inflammatory bowel disease. FEMS Immunol Med Microbiol 65(1):55–68. https://doi.org/10.1111/j.1574-695X.2012.00935.x
Rowan F, Docherty NG, Murphy M, Murphy B, Calvin Coffey J, O’Connell PR (2010) Desulfovibrio bacterial species are increased in ulcerative colitis. Dis Colon Rectum. https://doi.org/10.1007/DCR.0b013e3181f1e620
Boulangé CL, Neves AL, Chilloux J, Nicholson JK, Dumas M-E (2016) Impact of the gut microbiota on inflammation, obesity, and metabolic disease. Genome Med 8(1):42. https://doi.org/10.1186/s13073-016-0303-2
Zhang L et al (2021) Gut microbiota and type 2 diabetes mellitus: association, mechanism, and translational applications. Mediators Inflamm 2021:5110276. https://doi.org/10.1155/2021/5110276
Engels C, Ruscheweyh H-J, Beerenwinkel N, Lacroix C, Schwab C (2016) The common gut microbe Eubacterium hallii also contributes to intestinal propionate formation. Front Microbiol 7:713. https://doi.org/10.3389/fmicb.2016.00713
Maioli TU et al (2021) Possible benefits of faecalibacterium prausnitzii for obesity-associated gut disorders. Front Pharmacol 12:740636. https://doi.org/10.3389/fphar.2021.740636
Abo Ali FH, Ashour ZA, Shahin RY, Zaki WK, Ragab SB, Attia MY (2013) Role of intestinal microflora (Lactobacillus Acidophilus) in phagocytic function of leukocytes in type 2 diabetic patients. Egypt J Med Hum Genet. https://doi.org/10.1016/j.ejmhg.2012.10.003
Anand S, Kaur H, Mande SS (2016) Comparative in silico analysis of butyrate production pathways in gut commensals and pathogens. Front Microbiol 7:1945. https://doi.org/10.3389/fmicb.2016.01945
Bajaj JS et al (2012) Colonic mucosal microbiome differs from stool microbiome in cirrhosis and hepatic encephalopathy and is linked to cognition and inflammation. Am J Physiol Gastrointest Liver Physiol 303(6):G675-685. https://doi.org/10.1152/ajpgi.00152.2012
Chiu C-M et al (2014) Systematic analysis of the association between gut flora and obesity through high-throughput sequencing and bioinformatics approaches. BioMed Res Int 2014:906168. https://doi.org/10.1155/2014/906168
Srinivasan S et al (2019) Megasphaera lornae sp. Nov., Megasphaera hutchinsoni sp. Nov., and Megasphaera vaginalis sp. Nov.: novel bacteria isolated from the female genital tract. Int J Syst Evol Microbiol. https://doi.org/10.1099/ijsem.0.004702
Barlow GM, Yu A, Mathur R (2015) Role of the gut microbiome in obesity and diabetes mellitus. Nutr Clin Pract Off Publ Am Soc Parenter Enter Nutr. https://doi.org/10.1177/0884533615609896
Hiippala K et al (2020) Novel odoribacter splanchnicus strain and its outer membrane vesicles exert immunoregulatory effects in vitro. Front Microbiol 11:575455. https://doi.org/10.3389/fmicb.2020.575455
Gomez-Arango LF et al (2016) Increased systolic and diastolic blood pressure is associated with altered gut microbiota composition and butyrate production in early pregnancy. Hypertens Dallas Tex 1979. https://doi.org/10.1161/HYPERTENSIONAHA.116.07910
Shen Z et al (2018) Insights into Roseburia intestinalis which alleviates experimental colitis pathology by inducing anti-inflammatory responses. J Gastroenterol Hepatol. https://doi.org/10.1111/jgh.14144
Zhu C et al (2018) Roseburia intestinalis inhibits interleukin-17 excretion and promotes regulatory T cells differentiation in colitis. Mol Med Rep. https://doi.org/10.3892/mmr.2018.8833
Hoffmann TW et al (2016) Microorganisms linked to inflammatory bowel disease-associated dysbiosis differentially impact host physiology in gnotobiotic mice. ISME J. https://doi.org/10.1038/ismej.2015.127
Carbonero F, Benefiel AC, Alizadeh-Ghamsari AH, Gaskins HR (2012) Microbial pathways in colonic sulfur metabolism and links with health and disease. Front Physiol 3:448. https://doi.org/10.3389/fphys.2012.00448
Jie Z et al (2017) The gut microbiome in atherosclerotic cardiovascular disease. Nat Commun 8(1):845. https://doi.org/10.1038/s41467-017-00900-1
Braccia DJ, Jiang X, Pop M, Hall AB (2021) The capacity to produce hydrogen sulfide (H2S) via cysteine degradation is ubiquitous in the human gut microbiome. Front Microbiol 12:705583. https://doi.org/10.3389/fmicb.2021.705583
Kamboj K, Vasquez A, Balada-Llasat J-M (2015) Identification and significance of Weissella species infections. Front Microbiol 6:1204. https://doi.org/10.3389/fmicb.2015.01204
Gholizadeh P et al (2019) Microbial balance in the intestinal microbiota and its association with diabetes, obesity and allergic disease. Microb Pathog 127:48–55. https://doi.org/10.1016/j.micpath.2018.11.031
Macia L et al (2012) Microbial influences on epithelial integrity and immune function as a basis for inflammatory diseases. Immunol Rev. https://doi.org/10.1111/j.1600-065X.2011.01080.x
Vetrani C et al (2022) From gut microbiota through low-grade inflammation to obesity: key players and potential targets. Nutrients 14(10):2103. https://doi.org/10.3390/nu14102103
Yabe D, Kuwata H, Seino Y (2019) The journey to understanding incretin systems: Theory, practice and more theory. J Diabetes Investig. https://doi.org/10.1111/jdi.13123
Dula SB et al (2010) Evidence that low-grade systemic inflammation can induce islet dysfunction as measured by impaired calcium handling. Cell Calcium 48(2–3):133–142. https://doi.org/10.1016/j.ceca.2010.07.007
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
AD and NKP are employed by TCS Research, the R&D division of Tata Consultancy Services Ltd (TCS). SSM is associated to TCS Research as an advisor and consultant. While TCS supported the authors with salaries and remunerations, it had no role in design and execution of the study, nor in writing the article. The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dutta, A., Pinna, N.K. & Mande, S.S. Gut Microbiota of the Asian-Indian Type 2 Diabetes Phenotype: How Different It Is from the Rest of the World?. J Indian Inst Sci 103, 91–102 (2023). https://doi.org/10.1007/s41745-022-00351-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41745-022-00351-8