Abstract
This study measured the parents’ experience after using a mobile health (mHealth) app based upon interface design, readability, and effectiveness in order to discuss possible behavior change and weight management to prevent childhood obesity. A mixed method approach using the system usability scale and semi-structured interviews in two phases that occurred over a period of 6 consecutive weeks were undertaken. Six families (n = 12) were recruited, with having one obese child as the primary inclusion criteria. The study findings were classified into three different aspects, namely usability assessment, usability score result, and parents’ preference which demonstrated diversified experiences regarding two versions of the app. Prioritizing the second version in respect to its user-friendly interface, behavior change, and health information, participants suggested necessary amendments to operate the app straightforwardly. The most significant result has identified an inadequate concentration on user (parents’) engagement from the development to the refinement of an mHealth app. Hence, childhood weight management has progressively intensified parental awareness through the intervention of mHealth. Further research should take into account determining the reciprocal relation between user experiences and user engagement to explore the nature of effectiveness of an mHealth app.
Similar content being viewed by others
The prevention of childhood obesity is an urgent public health concern of the twenty-first century and continues threatening the health and well-being of children in developing as well as developed countries (Ogden et al. 2015; Popkin and Doak 1998; Sahoo et al. 2015). World Health Organization (WHO 2017) has defined obesity as “abnormal or excessive fat accumulation where body mass index is greater than or equal 30 that presents a risk to health.” Describing the excessiveness, the Center for Disease Control and Prevention (2017) has outlined that the prevalence of childhood obesity among school-going children (aged 6–11 years old) are nearly 19% around the world. To take the edge off, the health information technology offers new and innovative state-of-the-art approaches such as telemedicine, electronic health (eHealth), mobile health (mHealth), online health forums, and text messaging services (Dietz et al. 2015; Finney Rutten et al. 2012; Oh et al. 2015) in childhood weight management.
However, a growing consensus recognized that the mechanism of childhood obesity is diverse (Sahoo et al. 2015). Concomitantly, King and colleagues (King et al. 2018) proposed that childhood obesity-related apps will not be sufficing to overcome this health challenge singlehandedly. Despite the noticeable role of parents in children’s weight management, commercial health promotion apps have insignificantly targeted parents’ contribution by far (Curtis et al. 2015).
There has been a lack of studies in the development of a standardized design process to boost user engagement with mHealth apps (Schnall et al. 2016). It seems to be no compelling reason to argue that commercial app design process has been overlooked engaging the parents in improving interfaces to accelerate the social practices. Addressing the limitations, this study aimed at exploring the usability (using system usability scale) and user preference (measured through parents’ experiences) of a nutrition education–based mHealth app TreCLifeStyle intervention to contribute in childhood weight management.
mHealth apps offer a range of attributes for supporting health behavior change such as “zero-geography feature” (Tate et al. 2013) (p. 407) which means to deliver and receive the service directly to the families regardless of locations (Curtis et al. 2015). However, the primary healthcare service–oriented technologies for childhood obesity management mainly consider electronic medical records as an adjuvant to public health surveillance system (Flood et al. 2015). This approach has made a few obstructions for healthcare providers including uncertain sustainability and colossal time investment (Avis et al. 2016). Moreover, how the provider-driven decision indifferent end-user engagement and experience in mHealth design process has received almost no serious attention.
It is now well documented that mHealth apps regarding childhood weight management should be explored (Schoffman et al. 2013). A noticeable consensus among researchers demonstrated that mHealth apps based upon weight management will sustain longer when it comes to ensuring parental engagement (Curtis et al. 2015; Hingle et al. 2010), to considering associated personal and external factors during interface design. In line with that approach, current study put spotlight on parents of obese child who might intensify self-management in respect to sedentary behaviors and daily dietary habit of family members. How parental engagement in design process can play a crucial role to develop a scalable mHealth interface is the utmost preference of this study.
Material and Methods
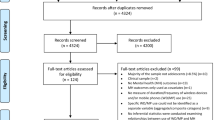
Research Design and Analysis
This study adopted mixed method research design to identify the perspectives and requirements of grassroot-level beneficiaries. Mixed method approach, also considered as a rigorous method, is effective to provide a deeper meaning of the phenomenon due to the potentiality of achieving both qualitative and quantitative dimension. Thus, the approach helped us to develop a broader understanding of mHealth usage in childhood obesity prevention. Participants underwent a semi-structured interview including questions about interface preference, dietary behavior, and user experience. Among other commonly used qualitative techniques (e.g., focus group discussion), semi-structured interview is more convenient to collect in-depth data from individual level. Considering study duration and other relevant resources, we found semi-structured interview as a best matched tool for this study. A “system usability scale (SUS) ideal format” (Brooke 1996, 2013; Lewis and Sauro 2018) was used to comprehend the usability of the mHealth app. SUS is well established in measuring usability of an interface. It consists of ten predefined questions (Brooke 2013) such as “I would like to use TreCLifeStyle app often,” “TreCLifeStyle app is useless and complex,” and “TreCLifeStyle app is easy to use” following a Likert scale (Allen and Seaman 2007). In the field of health information technology, usability signifies the effectiveness, efficiency, and satisfaction of the interface in a specified context of use (Bevan et al. 2015) while many people correlate the concept solely with “ease of use” of a product (Lowry et al. 2013). The study adopted thematic analysis (Braun et al. 2014) for qualitative data analysis, and quantitative data was guided by narrative analysis (Cortazzi 2014). Thus, the overall analysis of a process was followed by “mixing” and/or “combining” qualitative and quantitative data into a single study to provide richer data interpretations (Johnson et al. 2007).
Theoretical Framework Guiding the Study
Theories and models implemented in healthcare system (e.g., sedentary lifestyle, unhealthy diet, weight management) have guided researchers to construct intervention framework in order to explore behavior change (Curtis et al. 2015). Moreover, these models provided an integrated set of activities to translate theory into practice (S. Michie et al. 2011). Despite evoking outcomes, majority of these models have identified as static in structure (Michie et al. 2014). Research subsequently demonstrated the incoherence and incomprehensiveness together with a lack of consideration of the context in which a behavior happened and the explicit process of change in a model. Therefore, this study adopted stage of change theory also recognized as transtheoretical model (TTM) (Fernandez et al. 2016; Prochaska and Velicer 1997) to conceptualize the process of intentional behavior change (whether it happened or not). This study has observed five stages (precontemplation—not ready, contemplation—getting ready, preparation—ready, action—current “action,” maintenance—monitoring) of the change steps following the TTM. The TTM can be applied to a variety of behaviors, populations, and settings (e.g., treatment settings, prevention, and policy-making settings). While previous approaches in health promotion have spotlighted on biological influences in behavior (Sallis et al. 2015), the TTM incorporates decision-making process of individuals that is likely to be effective that is called intentional change (DiClemente 2015). Moreover, the TTM represented an extensive explanation of evidence-based behavior change intention.
Intervention Process and Detail Activities of the Study
The intervention of the TreCLifeStyle app has went through a step-by-step process, and the activities that have been undertaken in the study are presented in a tabulation format (Table 1).
-
Step 1:
meeting preuse of the app
-
Brief interview about children and habits related to the diet.
-
Questionnaire “La Dieta Mediterranea” (the Mediterranean diet).
-
Questionnaire about stage of behavior change.
-
Questionnaire about intention to use.
-
-
Step 2:
meeting post-use appA
-
Brief interview about children and habits related to the diet.
-
Questionnaire “La Dieta Mediterranea” (the Mediterranean diet).
-
SUS on appA.
-
Questionnaire about stage of behavior change.
-
Questionnaire about intention to use.
-
-
Step 3:
meeting post-use appB
-
Questionnaire “Dettagli su Dieta Mediterranea” (details of the Mediterranean diet).
-
SUS on appB.
-
Questionnaire about stage of behavior change.
-
Questionnaire about intention to use.
-
Final interview on the app TreCLifeStyle (comparison between both appA and appB) in their daily life.
-
Participants
The study site was in three rural areas of Trentino province, Italy (Grumo, Gardolo, and Riva del Garda), and two families were selected from each place. Participants were recruited from six single parent families who had one obese (BMI 85th–94th percentile) child through a convenience sampling method. Six parents (five females, one male) of six overweight children (two female, four male; mean age 8.83 years; SD 2.13) were selected and contacted with the help of enlisted pediatricians of a local organization named Fondazione Bruno Kessler (FBK), Trento. Twelve participants (n = 12) including parents and the overweight child (Table 2) were agreed to participate in the study. Initially, we informed the participants by phone call and fixed an interview schedule at their convenient. All the interviews have undertaken at participant’s home. Interviews were initiated by researchers from FBK, and a written informed consent was collected from the parents.
Data Collection
Data collection followed a close-ended questionnaire survey, system usability scale (SUS), and semi-structured interviews in two phases that lasted for six consecutive weeks and occurred between April and June 2016. Each interview was audio recorded and lasted for 20–30 min. Interviews and SUS questionnaires were completed in Italian language. Due to the language barrier, interviews were translated by a research assistant. The authors were aware of any kind of data misinterpretation; thus, the translated documents were re-checked for reliability by a professional translator.
Results
The study findings have been demonstrated through three interconnected thematic areas, namely usability assessment, usability score result, and parents’ preference—derived from a rigorous analysis of field data. Usability assessment talked about the usage pattern of the TreCLifeStyle app; usability score result incorporated usability score to determine the appropriateness of the app, and parents’ preference dealt with end-user’s experience regarding the app sustainability that discussed below.
Usability Assessment
The study developed a usability assessment poll comprising of specific questions underlined on the possible influence of the TreCLifeStyle app in respondents’ everyday life. The evaluation was followed a scoring scale from 1 to 5, where 1 demonstrates the “lowest influence” and 5 implies the “highest influence.” Field data explained that the most influenced participants were TL004 and TL006 whereas TL001 has confronted more operational issues of the app in different circumstances. Concerning the influence on dietary inquiries, TL001, TL003, and TL005 demonstrated inconsistency and the others have faced insignificant difficulties (Fig. 1).
Likewise, family food habit has been changed in each situation, and members were enthusiastic to partake in using the TreCLifeStyle app. Therefore, the participants get used to and became comfortable with modern innovative technologies which indicated a positive user acceptance. As a result, most of the respondents became self-dependent and ended up with relatively a distant contact with the pediatricians. Children accustomed to the jawbone bracelet (activity tracker) regularly to achieve the daily 10K-step goal. This activity tracker turned into a pulling in and intriguing instrument for them.
The study resulted a positive intention in behavior change among participants, and the impact of the app was analogous to each family. Majority of the families have scored over 15% while putting opinions on usability of the app (Fig. 2). Despite a positive impact of the app, two families (TL001 and TL003) scored slightly low compared with others that stipulates a dissatisfaction.
The study participants (both parents and children) reported regularly in respect to the food intake task by using the app. Since the parents were the main user of the app, they were involved in the reporting task and getting feedback. On the other hand, the children were using the jawbone bracelet to maintain everyday step goal. The overall stages of change were determined through the physical activity tracker, usage frequency, user engagement, and motivation level of the participants (Fig. 3).
A major finding was the constancy of participants in tracking daily meals. However, the interaction with the app has been abated significantly (mean number of meals inserted decreased from 2.79 to 0.44 per day) while the participants were asked to use the app electively.
Usability Score Result
The SUS score especially accounts for measuring usability, learnability, reliability, and validity of an app interface. Moreover, it represents an integrated measurement of the overall usability of the system (Bangor et al. 2008; Bevan 1995). The manifestation of SUS score follows a systematic approach. Each question should be converted into a new score ranging from 0 to 4. The aggregated scores need to multiply by 2.5 to acquire the general estimation of SUS (Brooke 1996). The scores that have a place from 0 (zero) to 100 do not denote the percentages, nevertheless ought to be considered as a percentile positioning. For example, SUS score 68 out of 100 represents the score that is at the 68th percentile in lieu of 68%. The SUS is neither a diagnosis nor an intention to tell about specific problems of the interface, yet it gives red (negative) or green (positive) signal to know how badly the usability needs to improve. Brook explained if a system score under 68 has probable serious problem with the interface usability which should be addressed further (Brooke 1996). Inversely, the system scored > 68 would be considered above average (Kortum and Sorber 2015) and more likely on right track. The score 80.3 or above stands for people who will use the interface without hesitation and will recommend to their friends.
To quantify the interface usability of the TreCLifeStyle app, this study developed a questionnaire following the “ideal” format of digital equipment corporation (Arntzen et al. 1995) comprises of ten questions. It was tested in two phases for version A and version B independently. Even though a dominant part of the questionnaire concentrated on usability of the interface, some essential questions especially demonstrated the experiences of end-users. The scale set up 1 to 5 score to gauge the data where 1 signified “strongly disagree” and 5 apprised “strongly agree.”
In both cases, a substantive status of the interface usability was displayed. The average SUS mean score was above 90 for appA and appB where the standard deviation was 3.6 (Figs. 4 and 5). The data appeared to suggest that each version had potential usability and gained user satisfaction. This result is considered as a compelling outcome of the user interfaces.
We observed that the usability score extended progressively in the second phase. For instance, the mean increased point for TL003, TL004, and TL005 was 7.5 (SD 2.5), and the mean score decreased for TL002 and TL006 was 2.5 points. Only TL001 remained consistent in both phases. Family of TL002 was still in the primary learning stage to use the appB in an effective manner. To clarify the downtrend, TL002 expressed, the interface of appA was straightforward to use whereas the second version (appB) contains a lot more information. On the other hand, the user TL006 deemed differently that appB is considerably more user-friendly and informative; yet it took a bit more time to learn properly. She added that, in contrast with both apps, appB is substantially user-friendly to understand even though it has some sophisticated features. Along with a huge amount of data generation and relatively complicated operating system, appB somewhat has created difficulties to comprehend the interfaces thoroughly.
Parents’ Preference
This section of the article has demonstrated the deterministic approach of end-users regarding the app. At the end of the piloting phase, participants were asked to use the TreCLifeStyle app (either appA or appB) voluntarily for the following 6 weeks. We found a diversified opinion from parents which was considered as first-hand user experience. The majority of parents have preferred appB to appA and shared their experience accordingly.
The statistics appeared in appB regarding nutrient balance and calories were convenient to the mother of TL001. According to her, appB gave access to add new meal and different food items. She found this version simpler and faster than appA.
The mother of child (TL002) said that her son is excited about the jawbone bracelet and became curious to see the daily footsteps in mobile phone. Since the appB showed daily footsteps along with some other features, the child become interested to use it regularly.
The father of third child (TL003) deemed that appB is more comfortable and direct. However, he faced some difficulties in adding different food items such as pasta and “fagioli” (beans), since these food items were not enlisted. He suggested to add insalata russa, tortel di patate (typical Italian food) to make the food item more comprehensive.
The mother of TL004 liked the refined functionalities of appB such as portions, statistics, and feedback. She agreed that appB was motivative, easy to use, and needs no tutorial to operate. In addition, the icons and functionalities were coherent and interactive. The visualization feature of the consumed calories was interesting to her; however, she found that appB is relatively time-consuming in terms of “food weight” option.
Parents have faced challenges to synchronize the activity tracker with a real-time data. Hence, the children used to lose the tracker when they go for some physical activities. These challenges need for further attention. The mother of TL005 was using the app and teaching the child how to use it properly. She expressed two interesting features regarding appB that assist her to determine the preference, for example, to take control over family eating habits and to see the nutrient statistics with appB.
The mother of TL006 was happy to see the calories and portions of her child’s everyday meal. She pointed that appB is relatively easier to know how much calorie the child is consuming in each meal and how much is missing. This family was one of the frequent app users, and the mother kept following the record on a regular basis. She added that the activity tracker and energy intake interface amazed them most to be motivated.
Discussion
The study findings imply that participants have shown continuous interest to use the app delightfully even if they did not receive any incentives. Data collected in relation to preferences of the app features demonstrates that usability of a product plays an imperative role to shape user experiences. We argue that usability of a system and user experience depends on each other. For example, version A had fewer objects in comparison with version B, and parents (users) get less opportunity to accumulate all records they needed to upload into the database. Consequently, the user experience asserts appA with an inadequate satisfaction and preference and drives them towards version B in most cases. Our observation validates the view that end-users consciously choose appB not only because of modified and user-friendly interfaces, but also because the fulfillment of missing requirements in appA was a coherent motive. In addition, the usability assessment result demonstrates that the context of current usability status leads to a sustainable idea for mHealth app designers.
Due to the inconsistent effect of large-scale mHealth projects that have been observed in previous studies (Aranda-Jan et al. 2014), communication technologies and mobility of information in healthcare have attracted the attention of practitioners, academic researchers, and policymakers globally (Free et al. 2013; Leslie et al. 2011; Steinhubl et al. 2015; Waegemann 2010). There has been an inconclusive debate about participant (mainly parents) engagement during mHealth app design and interventions to establish health indicators (Kohl et al. 2013). Concomitantly, the existing accounts have significantly failed to represent an adequate evidence on high-quality usability evaluation (Singh et al. 2016). Our study undertook a rigorous usability evaluation through a viable empirical data presentation that identifies the magnitude of user (parents) engagement in app design and intervention process. Therefore, on logical grounds, there is compelling reason to argue that the usability assessment tool, under the phrase “safety-enhanced design” of the study, demonstrates a progressive impact on end-users’ daily food habit and physical activities.
Together with three basic queries regarding academic contribution, our study has deepened the mHealth research periphery. Firstly, what is known about the topic? Nutrition and diet apps are offering the possibility of delivering behavior change interventions. However, the engagement of theoretical framework based on nutrition education within primary care interventions is still inadequate. Secondly, what does our study add? To our knowledge, none of the previous research accumulates parental role in behavior change and user-centered design to raise awareness on eating behavior and sedentary lifestyle together. The study significantly demonstrated that interactive interface (e.g., regular physical activities) is more effective than exclusively providing training and disseminating health-related information. Finally, what are the implications? The user’ experience might be supportive in the development of a user-friendly interface for intuitive interaction between the service providers and the service receivers.
This study has several limitations that must be acknowledged. First, the app is limited to a particular healthcare-based service. Second, participants were selected by the organization with the help of pediatricians who seemed reluctant to say something that might be considered too obvious.
Conclusion
With the contribution of a multidisciplinary team in the development of interfaces and incorporating contemporary healthy lifestyle guideline makes the app more compatible and congruent for study participants. Distinguished feedback from the parents regarding food intake, behavior monitoring, and information provision highlighted a significant advance over the functionality of the app. The most weighty finding emerged from this study is to ensure user engagement in mHealth app design. It can be a viable way to secure and maximize the effectiveness of an app. Our findings also determine the influences of parents' awareness of and motivation to change children's healthy lifestyle behaviors.
We are about to face a highly digitally skillful generation with an improved technological expertise in hand (Ben-Zeev et al. 2014). The future communities with a full range of capability to adopt the advanced level of sophisticated technologies could increase the potential impact on mHealth interventions. This is, therefore, a definite need to raise questions about the nature of effectiveness of a mHealth app in respect to comprehend the reciprocity between user experiences, and user engagement. Further research may emphasis on a validated model of user engagment while prototyping the app. Thus, the service providers would get insight into which pertinent aspects can draw parents attention and encourage towards a sustainable use of the app. Finally this study highlights the interactivity, novelty, and tailoring of app content as a considerable way to help increase parents and family's engagement with the app.
References
Allen, I. E., & Seaman, C. A. J. Q. p. (2007). Likert scales and data analyses., 40(7), 64–65.
Aranda-Jan, C. B., Mohutsiwa-Dibe, N., & Loukanova, S. (2014). Systematic review on what works, what does not work and why of implementation of mobile health (mHealth) projects in Africa. J BMC Public Health, 14(1), 188.
Arntzen, B. C., Brown, G. G., Harrison, T. P., & Trafton, L. L. (1995). Global supply chain management at Digital Equipment Corporation. J Interfaces, 25(1), 69–93.
Avis, J. L., Holt, N. L., Maximova, K., van Mierlo, T., Fournier, R., Padwal, R., … Ball, G. D. (2016). The development and refinement of an e-health screening, brief intervention, and referral to treatment for parents to prevent childhood obesity in primary care. J Telemedicine e-Health, 22(5), 385–394.
Bangor, A., Kortum, P. T., & Miller, J. T. (2008). An empirical evaluation of the system usability scale. International Journal of Human–Computer Interaction, 24(6), 574–594.
Ben-Zeev, D., Brenner, C. J., Begale, M., Duffecy, J., Mohr, D. C., & Mueser, K. T. (2014). Feasibility, acceptability, and preliminary efficacy of a smartphone intervention for schizophrenia. Schizophrenia Bulletin, 40(6), 1244–1253.
Bevan, N. (1995). Usability is quality of use. J Advances in Human Factors Ergonomics, 20, 349–349.
Bevan, N., Carter, J., & Harker, S. (2015). ISO 9241-11 revised: what have we learnt about usability since 1998? Paper presented at the International Conference on Human-Computer Interaction.
Braun, V., Clarke, V., & Terry, G. (2014). Thematic analysis. Qualitative Research in Clinical and Health Psychology, 24, 95–114.
Brooke, J. (1996). SUS—a quick and dirty usability scale. J Usability Evaluation in Industry, 189(194), 4–7.
Brooke, J. (2013). SUS: a retrospective. Journal of Usability Studies, 8(2), 29–40.
CDC (2017). Childhood Obesity Facts. Retrived from https://www.cdc.gov/healthyschools/obesity/facts.htm
Cortazzi, M. (2014). Narrative analysis. Routledge.
Curtis, K. E., Lahiri, S., & Brown, K. E. (2015). Targeting parents for childhood weight management: development of a theory-driven and user-centered healthy eating app. JMIR mHealth uHealth, 3(2).
DiClemente, C. (2015). Change is a process not a product: reflections on pieces to the puzzle. J Substance Use & Misuse, 50(8–9), 1225–1228.
Dietz, W. H., Baur, L. A., Hall, K., Puhl, R. M., Taveras, E. M., Uauy, R., & Kopelman, P. (2015). Management of obesity: improvement of health-care training and systems for prevention and care. The Lancet, 385(9986), 2521–2533.
Fernandez, A. C., Amoyal, N. R., Paiva, A. L., & Prochaska, J. O. (2016). Motivation for HPV vaccination among young adult men: validation of TTM decisional balance and self-efficacy constructs. American Journal of Health Promotion, 30(3), 163–171.
Finney Rutten, L. J., Davis, T., Beckjord, E. B., Blake, K., Moser, R. P., & Hesse, B. W. (2012). Picking up the pace: changes in method and frame for the health information national trends survey (2011–2014). Journal of Health Communication, 17(8), 979–989.
Flood, T. L., Zhao, Y.-Q., Tomayko, E. J., Tandias, A., Carrel, A. L., & Hanrahan, L. P. (2015). Electronic health records and community health surveillance of childhood obesity. American Journal of Preventive Medicine, 48(2), 234–240.
Free, C., Phillips, G., Watson, L., Galli, L., Felix, L., Edwards, P., … Haines, A. (2013). The effectiveness of mobile-health technologies to improve health care service delivery processes: a systematic review and meta-analysis. PLoS Medicine, 10(1), e1001363.
Hingle, M. D., O’Connor, T. M., Dave, J. M., & Baranowski, T. (2010). Parental involvement in interventions to improve child dietary intake: a systematic review. Journal Preventive Medicine, 51(2), 103–111.
Johnson, R. B., Onwuegbuzie, A. J., & Turner, L. A. (2007). Toward a definition of mixed methods research. Journal of Mixed Methods Research, 1(2), 112–133.
King, D., Rahman, E., Potter, A., & Van Teijlingen, E. (2018). NoObesity apps—from approach to finished app. Paper presented at the Proceedings of the Future Technologies Conference.
Kohl, L. F., Crutzen, R., & de Vries, N. K. (2013). Online prevention aimed at lifestyle behaviors: a systematic review of reviews. J Journal of medical Internet research, 15(7).
Kortum, P., & Sorber, M. (2015). Measuring the usability of mobile applications for phones and tablets. International Journal of Human-Computer Interaction, 31(8), 518–529.
Leslie, I., Sherrington, S., Dicks, D., Gray, N., & Chang, T. (2011). Mobile communications for medical care: a study of current and future healthcare and health promotion applications, and their use in China and elsewhere. Cambridge: University of Cambridge.
Lewis, J. R., & Sauro, J. (2018). Item benchmarks for the system usability scale. Journal of Usability Studies, 13(3).
Lowry, S. Z., Quinn, M. T., Ramaiah, M., Brick, D., Patterson, E. S., Zhang, J., … Implementation. (2013). A human factors guide to enhance EHR usability of critical user interactions when supporting pediatric patient care (nistir 7865). J Electronic Health Records: Challenges in Design, 79.
Michie, S., Van Stralen, M. M., & West, R. (2011). The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation Science, 6(1), 42.
Michie, S. F., West, R., Campbell, R., Brown, J., & Gainforth, H. (2014). ABC of behaviour change theories. Silverback Publishing.
Ogden, C. L., Carroll, M. D., Fryar, C. D., & Flegal, K. M. (2015). Prevalence of obesity among adults and youth: United States, 2011–2014. US Department of Health and Human Services, Centers for Disease Control and Prevention.
Oh, B., Cho, B., Han, M. K., Choi, H., Lee, M. N., Kang, H.-C., et al. (2015). The effectiveness of mobile phone-based care for weight control in metabolic syndrome patients: randomized controlled trial. JMIR mHealth & uHealth, 3(3).
Popkin, B. M., & Doak, C. M. (1998). The obesity epidemic is a worldwide phenomenon. Nutrition Reviews, 56(4), 106–114.
Prochaska, J. O., & Velicer, W. F. (1997). The transtheoretical model of health behavior change. American Journal of Health Promotion, 12(1), 38–48.
Sahoo, K., Sahoo, B., Choudhury, A. K., Sofi, N. Y., Kumar, R., Bhadoria, A. S., & care, p. (2015). Childhood obesity: causes and consequences. Journal of family medicine, 4(2), 187.
Sallis, J. F., Owen, N., & Fisher, E. (2015). Ecological models of health behavior. Health Behavior: Theory, Research, Practice, (5), 43–64.
Schnall, R., Rojas, M., Bakken, S., Brown, W., III, Carballo-Dieguez, A., Carry, M., et al. (2016). A user-centered model for designing consumer mobile health (mHealth) applications (apps). Journal of Biomedical Informatics, 60, 243–251.
Schoffman, D. E., Turner-McGrievy, G., Jones, S. J., & Wilcox, S. (2013). Mobile apps for pediatric obesity prevention and treatment, healthy eating, and physical activity promotion: just fun and games? Translational Behavioral Medicine, 3(3), 320–325.
Singh, K., Drouin, K., Newmark, L. P., Lee, J., Faxvaag, A., Rozenblum, R., et al. (2016). Many mobile health apps target high-need, high-cost populations, but gaps remain. Health Affairs, 35(12), 2310–2318.
Steinhubl, S. R., Muse, E. D., & Topol, E. J. (2015). The emerging field of mobile health. Science Translational Medicine, 7(283), 283rv283–283rv283.
Tate, E. B., Spruijt-Metz, D., O’Reilly, G., Jordan-Marsh, M., Gotsis, M., Pentz, M. A., & Dunton, G. F. (2013). mHealth approaches to child obesity prevention: successes, unique challenges, and next directions. Translational Behavioral Medicine, 3(4), 406–415.
Waegemann, C. P. (2010). mHealth: the next generation of telemedicine? Telemedicine & e-Health, 16(1), 23–26.
WHO (2017). What is overweight and obesity? Retrieved from https://www.who.int/dietphysicalactivity/childhood_what/en/
Acknowledgements
We gratefully acknowledge all the participants in this study. The authors also thank FBK eHealth unit, Trento, Italy, Rosa Maimone, Silvia Fornasini, and Marco Dianti for their support with the study’s implementation and data acquisition. The corresponding author is especially thankful to Prof. Kim Usher, University of New England for her valuable comments, and A/Prof. Renato Troncon, University of Trento for his advice and feedback during the research work. The research team is especially thankful to Christopher Clancy for his proofreading, constructive feedback, and time.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Even though the community and patients agree to participate willingly, the study has followed an appropriate informed consent or assent procedures for data collection and was approved by the institutional review board at the University of Trento for Smart Community Design and Management (SCoDeM).
Competing Interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Rahman, A., Jahan, Y. Childhood Weight Management: the Development and Refinement of an mHealth Intervention in Primary Care. J. technol. behav. sci. 4, 309–317 (2019). https://doi.org/10.1007/s41347-019-00096-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41347-019-00096-9