Abstract
Introduction
Anemia and malnutrition are recognized indicators of suboptimal physical condition in chronic inflammatory diseases. This study aimed to examine the association between anemia, low body mass index (BMI), and clinical outcomes in axial spondyloarthritis (axSpA).
Method
This cross-sectional analysis utilized data from the multicenter ChinaSpA cohort. A total of 4146 participants with axSpA were categorized into four groups based on BMI and hemoglobin levels: those with both anemia and low BMI, those with anemia only, those with low BMI only, and those with neither condition. Logistic regression analyses were performed to analyze the association between anemia, low BMI, inflammation status, functional impairment, and disease activity.
Results
Anemia was present in 13.94%, low BMI in 11.99%, and both conditions in 2.15% of axSpA participants. Those with both anemia and low BMI showed significantly higher levels of inflammation (hypersensitive C-reactive protein [hsCRP] 30.60 mg/L vs. 8.44 mg/L), functional impairment (Bath Ankylosing Spondylitis Functional Index [BASFI] 3.80 vs. 2.10), and disease activity (Bath Ankylosing Spondylitis Disease Activity Index [BASDAI] 4.52 ± 2.04 vs. 3.67 ± 2.21; Ankylosing Spondylitis Disease Activity Score calculated with C-reactive protein [ASDAS_CRP] 3.51 ± 1.10 vs. 2.62 ± 1.21) compared to those without these conditions. After adjusting for sex and age, significant associations were observed between elevated hsCRP levels and the presence of low BMI (odds ratio [OR] 1.44, 95% CI 1.17–1.78), anemia (OR 1.91, 95% CI 1.56–2.32), and their concurrent presence (OR 3.59, 95% CI 2.22–5.80). Similarly, increased BASFI was significantly associated with low BMI (OR 1.57, 95% CI 1.25–1.97), anemia (OR 1.47, 95% CI 1.19–1.80), and their combination (OR 3.11, 95% CI 2.02–4.78).
Conclusion
All-cause anemia and low BMI are prevalent complications in patients with axSpA, exhibiting a significant correlation with elevated inflammation status and functional impairment. The simultaneous occurrence of anemia and low BMI particularly exacerbates clinical outcomes, emphasizing the critical role of comprehensive nutritional assessment and management in the therapeutic strategy for axSpA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Despite the acknowledged importance of anemia and malnutrition as indicators of suboptimal nutritional condition in chronic inflammatory diseases like axial spondyloarthritis (axSpA), there is a scarcity of comprehensive documentation on the reported prevalence of these conditions among patients with axSpA, leaving a gap in understanding their clinical implications. |
In patients with axSpA, we hypothesize that the co-occurrence of anemia and low BMI is associated with heightened inflammation, limited function, and increased disease activity compared to individuals without these conditions. |
What was learned from the study? |
Anemia and low BMI represent commonly observed complications among individuals with axSpA, demonstrating a noteworthy association with heightened inflammation status and impaired function. |
Notably, when both anemia and low BMI coexisted, the associations grew more pronounced. |
Our findings underscore the significance of incorporating both indicators into disease assessments, highlighting the imperative for regular screening and management of anemia and low BMI in patients with axSpA to optimize outcomes, and emphasizing the potential benefits of addressing these nutritional factors as integral components of the comprehensive treatment approach deserving significant attention. |
Introduction
Axial spondyloarthritis (axSpA) is a chronic inflammatory disease involving the sacroiliac joint and spine, potentially resulting in severe impairment of spinal mobility and physical function, thereby adversely affecting quality of life [1]. Ankylosing spondylitis (AS) is considered to be the prototype of axSpA, with a prevalence of between 0.2% and 0.4% in China [2].
Anemia and malnutrition, which encompass factors such as low body mass index (BMI), insufficient vitamin and mineral intake, overweight, and obesity, serve as discernible indicators of compromised nutritional condition, and their correlation with chronic inflammatory diseases has been established through various studies [3,4,5,6]. However, reports on the prevalence and clinical significance of anemia in patients with axSpA are scarce and often derive from limited small-scale studies with considerable variability in findings, ranging from 5.6% to 47.9% [7,8,9,10,11,12]. Furthermore, a study conducted on a small sample size indicated an association between anemia and disease activity [12]. However, to validate these findings, further studies encompassing a more diverse population are warranted.
BMI is defined as the weight in kilograms divided by the square of the height in meters. A low BMI, defined as less than 18.5 kg/m2 [13, 14], has been variably prevalent in the axSpA population, with reports ranging from 3.6% to 39.0% [15, 16]. Previous investigations regarding BMI in chronic inflammatory rheumatic diseases have primarily focused on the overweight and obese population, given that obesity and overweight account for a significant proportion of the nutritional burden in developed nations like the USA. In fact, the prevalence of obesity reached 35.5% among adult men and 35.8% among adult women in America in 2009–2010 [17], with a mere 1.6% of US adults aged 20 and over classified as underweight [18]. However, in low-income countries, low BMI remains a pressing nutritional challenge [19]. For example, the prevalence of low BMI in Southeast Asia varies widely, highlighting a nutritional issue that is especially pertinent in these regions. In Southeast Asian nations, the prevalence of low BMI ranges from 5.5% in Thailand to 26.7% in Sri Lanka among young adolescents aged 12–15 [20]. In Bangladesh, the prevalence of low BMI reaches a staggering 30.4% [21]. In China, approximately 4.6% of adults are classified as low BMI [22], while among individuals over 75 years of age, the prevalence of low BMI stands at 5.2% in urban areas and 10.9% in rural areas [23]. Consequently, the role of low BMI in the context of inflammatory diseases warrants significant attention, particularly in Asia, where a considerable portion of the population grapples with the burden of being underweight.
In this study, we delineate the prevalence of anemia and low BMI in the ChinaSpA cohort, consisting of over 4000 individuals with axSpA. This cross-sectional study embarks on a novel investigation into the association between nutritional status—reflected by anemia and low BMI—and outcomes of axSpA including inflammation status, disease activity, and functional impairment.
Methods
Source of Data
Data were sourced from the Chinese Rheumatology Data Center (CRDC) from August 1, 2018 to March 31, 2020, and collected from 300 registries in China [24]. The study was approved by the ethics committee of Peking Union Medical College Hospital (PUMCH), and the study was conducted according to the Declaration of Helsinki. All patients signed an informed consent.
Inclusion and Exclusion Criteria
The main inclusion criteria of the ChinaSpA registry were to have a clinical diagnosis of axSpA. In addition, participants needed to fulfill the Assessment in SpondyloArthritis international Society (ASAS) criteria for axSpA [25]. The age of participants was greater than or equal to 18 years old. Participants without information on hemoglobin (Hb) and BMI were excluded.
Data Collection
Patients with a clinical diagnosis of axSpA were approached by local investigators to determine their eligibility for the study. After eligible patients consented, their clinical and laboratory information was collected via the CRDC registration platform.
At baseline, the following clinical information was collected from participants:
-
1.
Demographic information, including sex, age, height, and body weight.
-
2.
Clinical presentation, including age of onset, age of diagnosis, presence of inflammatory back pain, dactylitis, peripheral arthritis, and enthesitis. Comorbidities, including the presence of psoriasis, iritis, and inflammatory bowel disease (IBD), which was defined as ulcerative colitis or Crohn’s disease diagnosed by a physician. Time of symptom onset was defined as the time when first clinical symptom occurred, including inflammatory back pain, peripheral arthritis, Achilles tendinitis, dactylitis, psoriasis, uveitis, and IBD. Time of diagnosis was defined as the time when a definitive diagnosis of axSpA was made.
-
3.
Physical examinations, including tender and swollen joint counts and Maastricht Ankylosing Spondylitis Enthesitis Score for enthesitis (MASES) [26].
-
4.
Family history of SpA or SpA-related diseases.
-
5.
Past medical history of fragility fracture and joint replacement.
-
6.
Laboratory tests, including human leukocyte antigen B27 (HLA-B27) positivity, hypersensitive C-reactive protein (hsCRP) levels, and Hb levels.
-
7.
Past or current treatments, including nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying anti-rheumatic drugs (DMARDs) such as sulfasalazine and methotrexate, and biologics such as tumor necrosis factor inhibitors (TNFi).
Several disease activity and functional assessments were measured to report patient outcomes. Disease activity in participants with axSpA was evaluated using the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) [27] or the Ankylosing Spondylitis Disease Activity Score calculated with C-reactive protein (ASDAS_CRP) [28]. Functional impairment was evaluated utilizing the Bath Ankylosing Spondylitis Functional Index (BASFI) [29].
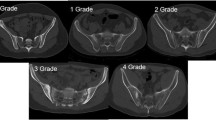
BMI was calculated as the body mass divided by the square of body height and classified into distinct categories: low BMI (BMI < 18.5 kg/m2), normal BMI (BMI 18.5–24.9 kg/m2), overweight (BMI 25–29.9 kg/m2), and obese (BMI ≥ 30 kg/m2) [13, 14]. Anemia was defined as Hb levels below 130 g/L in men or below 120 g/L in women [30, 31]. Elevated hsCRP was identified as hsCRP levels ≥ 10 mg/L, serving as an indicative marker of heightened inflammatory status.
Data Analysis
The participants with axSpA were categorized into four groups: the combined group, consisting of individuals with both anemia and low BMI; the anemic group, comprising those with anemia only; the low BMI group, comprising those with low BMI only; and the control group, consisting of individuals with axSpA who were neither anemic nor low BMI. Descriptive statistics were calculated to summarize the characteristics of all participants. For numerical variables, means and standard deviations (SD) were reported for normally distributed data, while median values along with the 25th and 75th percentiles (q25, q75) were used for non-normally distributed data. Categorical variables were presented as counts and percentages. Group comparisons were conducted using chi-square tests, Kruskal–Wallis tests, or analysis of variance (ANOVA), and for multiple comparisons, Dwass-Steel-Critchlow-Fligner (DSCF) tests and Bonferroni tests were employed. Bivariate logistic regression analyses were performed, using BASDAI (< 4 vs. ≥ 4), ASDAS_CRP (< 2.1 vs. ≥ 2.1), BASFI (< 4 vs. ≥ 4), or hsCRP (< 10 vs. ≥ 10 mg/L) as dependent variables, to calculate adjusted odds ratios (ORs) and their corresponding 95% confidence intervals (95% CI), while controlling for sex and age. Statistical significance was determined using a p value threshold of < 0.05, and all statistical analyses were conducted using SAS 9.4 software (SAS Institute, Cary, NC, USA).
Results
Clinical Characteristics of the Study Population
A total of 4146 participants with axSpA were enrolled in the study, of which 3112 (75.06%) were male. The mean age of the study population was 34.06 ± 10.59 years old, and the mean BMI was 23.51 ± 5.74. Participants had a mean age of onset of 26.93 ± 9.55 years old, a mean age of diagnosis of 30.41 ± 10.59 years old. Among the participants, 88.54% (n = 3671) tested positive for HLA-B27.
Within the enrolled participants, 48.63% (n = 2016) had elevated levels of hsCRP (≥ 10 mg/L), 44.96% (n = 1864) had BASDAI ≥ 4, 28.73% (n = 1191) had BASFI ≥ 4, and 66.28% (n = 2748) had ASDAS_CRP ≥ 2.1. Furthermore, 13.19% of participants received treatment with TNFi alone.
Distribution of Participants with Anemia and Low BMI
In the ChinaSpA cohort, 11.99% of participants had a low BMI, 13.94% exhibited anemia, and 2.15% presented with both low BMI and anemia. When stratified by sex, the prevalence of low BMI, anemia, and the combination of low BMI and anemia was 9.0%, 12.5%, and 2.0% in men, and 12.3%, 9.7%, and 2.5% in women, respectively (Fig. 1).
Comparatively, the low BMI group displayed a higher proportion (10.57% vs. 9.15%) of individuals with elevated inflammation status (hsCRP ≥ 10 mg/L) compared to those with low inflammation status (hsCRP < 10 mg/L). Similar patterns were observed in the anemic group and the combined group (15.03% vs. 8.73% and 3.22% vs. 1.13%, respectively). Similarly, among individuals with functional impairment (BASFI ≥ 4), the proportions of the low BMI, anemia, and combined group were greater compared to those with normal function (BASFI < 4) (10.92% vs. 9.41%, 14.78% vs. 10.59%, and 3.61% vs. 1.56%) (Fig. 2).
Distribution of anemia and low BMI according to inflammation status (a), disease activity (c, d), and functional impairment (b). ASDAS_CRP Ankylosing Spondylitis Disease Activity Score calculated with C-reactive protein, BASDAI Bath Ankylosing Spondylitis Disease Activity Index, BASFI Bath Ankylosing Spondylitis Functional Index, BMI body mass index, hsCRP hypersensitive C-reactive protein
Among participants with elevated inflammation status (hsCRP ≥ 10 mg/L), the combined group exhibited the highest proportion. This pattern remained consistent among participants with heightened disease activity (BASDAI ≥ 4 or ASDAS_CRP ≥ 2.1) and impaired physical function (BASFI ≥ 4) (Fig. 3).
Distribution of anemia and low BMI in patients with a high inflammatory status, high disease activity, and impaired function. ASDAS_CRP Ankylosing Spondylitis Disease Activity score calculated with C-reactive protein, BASDAI Bath Ankylosing Spondylitis Disease Activity Index, BASFI Bath Ankylosing Spondylitis Functional Index, BMI body mass index, hsCRP hypersensitive C-reactive protein
Characteristics of Participants with Anemia, Low BMI, or both
The characteristics of participants in the low BMI group, the anemic group, and the combined group are presented in Table 1. Participants in the low BMI group had an earlier age of onset and diagnosis and a higher prevalence of peripheral joint involvement than controls.
Compared with the control, participants in the anemic group exhibited higher levels of inflammation as measured by hsCRP [15.00 (5.00, 39.80) mg/L vs. 8.44 (3.00, 21.00) mg/L], poorer function assessed by BASFI [2.90 (1.10, 5.30) vs. 2.10 (0.50, 4.00)], higher disease activity measured by ASDAS_CRP [3.00 ± 1.25 vs. 2.62 ± 1.21], and a higher prevalence of enthesitis (67.08% vs. 64.25%). Notably, among the four groups, participants solely affected by anemia had the highest age at onset and age at diagnosis.
Participants in the combined group exhibited an earlier age at onset (22.75 ± 8.10 vs. 27.25 ± 9.28 years) and age at diagnosis (26.26 ± 8.68 vs. 30.82 ± 10.40 years), higher levels of inflammation measured by hsCRP [30.60 (8.85, 59.60) mg/L vs. 8.44 (3.00, 21.00) mg/L], functional impairment measured by BASFI [3.80 (2.00, 6.10) vs. 2.10 (0.50, 4.00)], and higher disease activity measured by BASDAI [4.52 ± 2.04 vs. 3.67 ± 2.21] and ASDAS_CRP [3.51 ± 1.10 vs. 2.62 ± 1.21] compared to controls. Additionally, participants in the combined group had a higher proportion of BASDAI ≥ 4, BASFI ≥ 4, ASDAS_CRP ≥ 2.1, and hsCRP ≥ 10 mg/L compared to the low BMI group.
Association Analysis
In the logistic regression model adjusted for sex and age, all three groups—low BMI, anemic, and combined—exhibited an association with elevated hsCRP levels compared to the control group, with odds ratios (ORs) of 1.44 [95% confidence interval (95% CI) 1.17–1.78], 1.91 (95% CI 1.56–2.32), and 3.59 (95% CI 2.22–5.80), respectively (Table 2).
Similarly, all three groups demonstrated an association with functional impairment, which was exemplified by the BASFI [low BMI group, OR 1.57 (95% CI 1.25–1.97); anemic group, OR 1.47 (95% CI 1.19–1.80); combined group, OR 3.11 (95% CI 2.02–4.78)].
Moreover, when compared to the control group, the combination of anemia and low BMI was linked to higher disease activity as measured by BASDAI [OR 2.14 (95% CI 1.39–3.31)] and ASDAS_CRP [OR 3.73 (95% CI 2.18–6.37)].
Discussion
In this large-scale, national, multicenter, cross-sectional study, we have elucidated the prevalence of all-cause anemia and low BMI among patients with axSpA, and explored the association between these conditions and key dimensions of axSpA assessment, namely inflammatory status, disease activity, and functional impairment. Inflammatory status was assessed by hsCRP levels, functional impairment by BASFI, and disease activity by BASDAI and ASDAS_CRP. Our findings indicate that all-cause anemia and low BMI are prevalent comorbidities in patients with axSpA, and both are linked to increased inflammatory status and functional impairment. Notably, in cases where all-cause anemia and low BMI co-occurred, albeit in a smaller subset of patients, these associations were pronounced, also demonstrating an association with heightened disease activity.
Among the 4146 participants with axSpA in the ChinaSpA cohort, the prevalence of anemia was 13.94%. Anemia is frequently observed as a comorbidity in individuals with inflammatory rheumatic diseases. Previous reports have presented a wide range of anemia frequencies. For instance, in a clinical series involving 212 patients with AS during the late 1950s, anemia was found in only 12 cases (5.6%) [7]. In 1989, 47.5% of 40 Mexican Mestizos with AS had Hb values below the normal limits [8]. More recent studies conducted over the past decade have reported prevalence rates of anemia ranging from 15% to 28.8% [9,10,11,12]. Notably, these investigations were based on small sample sizes, whereas our results are derived from the largest population to date, thereby providing a more reliable estimation of anemia prevalence among Chinese patients with axSpA. Anemia associated with chronic diseases (ACD) and anemia secondary to gastrointestinal blood loss induced by NSAIDs are considered significant contributors to axSpA-related anemia. Zviahina et al. reported that 28.8% of 118 patients with AS had anemia, of which 44.1% had ACD, 29.4% had ACD with iron deficiency, and 23.5% had iron deficiency anemia [12]. Another study found that 15% (n = 356) of patients with AS experienced anemia, with 25% of these cases attributed to ACD [32].
In this study, patients with axSpA with anemia showed higher levels of inflammatory biomarkers and more severe functional impairments. In 2009, a prospective study found that the improvement of Hb in patients with AS treated with TNFi for 6 months was significantly and independently associated with improvements in BASFI [4]. In another study, infliximab-treated patients with elevated CRP or interleukin-6 (IL-6) levels at baseline were more likely to have an improvement in Hb levels than those with lower levels [10]. In 2012, Bes et al. reported that after 52 weeks of treatment with TNFi, the improvement in Hb was related to a resolution in inflammation [11]. However, none of these studies have provided direct evidence regarding the association of anemia with inflammatory status and functional impairment. Our findings are consistent with those reported by Zviahina et al. in 2020, who found an association between anemia and inflammatory biomarkers (CRP and IL-6) [12]. Alternately, this could be interpreted via reverse causality—inflammation and other related diseases could lead to anemia. Thus, further prospective studies are warranted to elucidate the temporal relationship between these two conditions in individuals with axSpA and to understand the impact of anemia on disease progression.
On the other hand, our study revealed that 11.99% of patients with axSpA were classified as having a low BMI, which is higher than the prevalence of low BMI among the general Chinese adult population (4.6%) [22]. Interestingly, we found that low BMI was associated with elevated levels of inflammatory status and impaired function. The link between low BMI and inflammation can be attributed to the impact of inflammatory factors on muscle and fat cells, leading to increased energy expenditure [33]. It is noteworthy that the distribution of low BMI among individuals with SpA and its association with inflammatory status and function impairment have been largely overlooked, with only a limited number of studies investigating this aspect. In the SPACE cohort, 3.6% of the 168 patients with axSpA had a low BMI [15]. Additionally, Zhao et al. reported that among patients with AS requiring total hip arthroplasty, 39% were identified as having a low BMI [16]. Our study addresses this gap in the literature, highlighting that a low BMI is not uncommon within the Chinese axSpA population.
The significance of our study lies in revealing all-cause anemia and low BMI as prevalent complications in axSpA, which are associated with increased inflammatory status and functional impairment. The low BMI population in axSpA has been mostly neglected in previous studies compared to the obese and overweight population, and our study underscored the fact that nutritional management of patients with low BMI is also worthy of attention. Furthermore, by proposing a novel perspective on the role of nutritional factors, including all-cause anemia and low BMI, in axSpA, our study paves the way for a more integrated treatment approach that includes nutritional management as a pivotal component of comprehensive patient care.
A limitation of this study is that anemia was not further classified; therefore, the question of whether ACD is more strongly associated with inflammation than all-cause anemia remains elusive. In a study exploring the effect of golimumab treatment on Hb levels in patients with inflammatory arthritis including rheumatoid arthritis (RA), psoriatic arthritis (PsA), and AS, it was found that in patients with RA, there was a significant negative association between disease activity and Hb improvement in inflammatory anemia, mixed anemia, and all-cause anemia subgroups, and this association was found to be stronger in inflammatory anemia and mixed anemia subgroups than in all-cause anemia subgroups. As a result of the small sample size, conclusive results were not obtained for the AS group [32]. In the future, further studies are needed to investigate the association between different types of anemia and disease burden in axSpA. In addition, it has been shown in RA studies that patients respond better to drugs if anemia is successfully treated [34]. Therefore, in the future, further research is needed to determine whether patients with axSpA and different types of anemia can obtain a better prognosis by adding treatment to correct anemia on the basis of regular therapy. Another limitation of this paper is that we were unable to obtain data such as iron intake, socioeconomic status, and education level, which could have biased our conclusions as unmeasured confounders.
Conclusion
In Chinese patients with axial axSpA, all-cause anemia and low BMI emerged as prevalent complications, both demonstrating associations with heightened inflammation status and functional impairment. Notably, the impact of these indicators on inflammation and functional impairment was magnified when patients presented with both all-cause anemia and low BMI simultaneously. These findings emphasize the importance of considering both indicators when conducting disease assessments and the need for routine screening and management of all-cause anemia and low BMI in patients with axSpA to optimize disease outcomes. Conclusively, the potential benefits of addressing these nutritional factors as part of the overall treatment approach for axSpA is noteworthy.
Data Availability
The datasets generated during and/or analyzed during the current study are available in the Chinese Rheumatology Information Platform repository, http://emr.criponline.com/public/login/index.
References
Sieper J, Poddubnyy D. Axial spondyloarthritis. Lancet. 2017;390(10089):73–84.
Zhang S, Peng L, Li Q, et al. Spectrum of spondyloarthritis among Chinese populations. Curr Rheumatol Rep. 2022;24(8):247–58.
Weiss G, Goodnough LT. Anemia of chronic disease. N Engl J Med. 2005;352(10):1011–23.
Weiss G, Schett G. Anaemia in inflammatory rheumatic diseases. Nat Rev Rheumatol. 2013;9(4):205–15.
Cho SH, Lee H, Kwon H, et al. Association of underweight status with the risk of tuberculosis: a nationwide population-based cohort study. Sci Rep. 2022;12(1):16207.
de Heredia FP, Gómez-Martínez S, Marcos A. Obesity, inflammation and the immune system. Proc Nutr Soc. 2012;71(2):332–8.
Wilkinson M, Bywaters EG. Clinical features and course of ankylosing spondylitis; as seen in a follow-up of 222 hospital referred cases. Ann Rheum Dis. 1958;17(2):209–28.
Burgos-Vargas R, Naranjo A, Castillo J, Katona G. Ankylosing spondylitis in the Mexican mestizo: patterns of disease according to age at onset. J Rheumatol. 1989;16(2):186–91.
Niccoli L, Nannini C, Cassarà E, Kaloudi O, Cantini F. Frequency of anemia of inflammation in patients with ankylosing spondylitis requiring anti-TNFα drugs and therapy-induced changes. Int J Rheum Dis. 2012;15(1):56–61.
Braun J, van der Heijde D, Doyle MK, et al. Improvement in hemoglobin levels in patients with ankylosing spondylitis treated with infliximab. Arthritis Rheum. 2009;61(8):1032–6.
Bes C, Yazici A, Soy M. Monoclonal anti-TNF antibodies can elevate hemoglobin level in patients with ankylosing spondylitis. Rheumatol Int. 2013;33(6):1415–8.
Zviahina OV, Shevchuk SV, Kuvikova IP, Segeda IS. Anemia in patients with ankylosing spondylitis, association with the activity of the inflammatory process and the severity of the disease. Wiad Lek. 2020;73(4):715–21.
World Health Organisation. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894(i–xii):1–253.
Tan KC. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–63.
Rubio Vargas R, van den Berg R, van Lunteren M, et al. Does body mass index (BMI) influence the ankylosing spondylitis disease activity score in axial spondyloarthritis? Data from the space cohort. RMD Open. 2016;2(1):e000283.
Zhao J, Li J, Zheng W, Liu D, Sun X, Xu W. Low body mass index and blood loss in primary total hip arthroplasty: results from 236 consecutive ankylosing spondylitis patients. Biomed Res Int. 2014;2014: 742393.
Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–7.
Fryar CD, Carroll MD, Afful J. Prevalence of underweight among adults aged 20 and over: United States, 1960–1962 through 2017–2018. NCHS Health E-Stats. 2020. https://www.cdc.gov/nchs/data/hestat/underweight-adult-17-18/underweight-adult.htm
Moore S, Hall JN, Harper S, Lynch JW. Global and national socioeconomic disparities in obesity, overweight, and underweight status. J Obesity. 2010;2010: 514674.
Yang L, Bovet P, Ma C, Zhao M, Liang Y, Xi B. Prevalence of underweight and overweight among young adolescents aged 12–15 years in 58 low-income and middle-income countries. Pediatr Obes. 2019;14(3):e12468.
Biswas T, Garnett SP, Pervin S, Rawal LB. The prevalence of underweight, overweight and obesity in Bangladeshi adults: data from a national survey. PLoS ONE. 2017;12(5):e0177395.
Gao B, Zhang L, Zhao M. Underweight but metabolically abnormal phenotype: metabolic features and its association with cardiovascular disease. Eur J Intern Med. 2016;29:46–51.
Song P, Man Q, Li Y, et al. Trends of underweight malnutrition among chinese residents aged 60 years and above—China, 1992–2015. China CDC Wkly. 2021;3(11):232–6.
Su J, Wang R, Duan X, et al. Clinical characteristics of axial spondyloarthritis patients in China: results from ChinaSpA, the Chinese spondyloarthritis registry. Clin Exp Rheumatol. 2022;40(3):544–50.
Rudwaleit M, van der Heijde D, Landewé R, et al. The development of Assessment of Spondyloarthritis International Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis. 2009;68(6):777–83.
Heuft-Dorenbosch L, Spoorenberg A, van Tubergen A, et al. Assessment of enthesitis in ankylosing spondylitis. Ann Rheum Dis. 2003;62(2):127–32.
Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin A. A new approach to defining disease status in ankylosing spondylitis: the Bath ankylosing spondylitis disease activity index. J Rheumatol. 1994;21(12):2286–91.
Lukas C, Landewé R, Sieper J, et al. Development of an ASAS-endorsed disease activity score (ASDAS) in patients with ankylosing spondylitis. Ann Rheum Dis. 2009;68(1):18–24.
Calin A, Jones SD, Garrett SL, Kennedy LG. Bath ankylosing spondylitis functional index. Br J Rheumatol. 1995;34(8):793–4.
Anaemias NU. Report of a WHO scientific group. World Health Organ Tech Rep Ser. 1968;405:5–37.
World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Geneva: WHO; 2011. Contract No.: WHO/NMH/NHD/MNM/11.1.
Furst DE, Kay J, Wasko MC, et al. The effect of golimumab on haemoglobin levels in patients with rheumatoid arthritis, psoriatic arthritis or ankylosing spondylitis. Rheumatology (Oxford). 2013;52(10):1845–55.
Argilés JM, Busquets S, Stemmler B, López-Soriano FJ. Cancer cachexia: understanding the molecular basis. Nat Rev Cancer. 2014;14(11):754–62.
Wilson A, Yu HT, Goodnough LT, Nissenson AR. Prevalence and outcomes of anemia in rheumatoid arthritis: a systematic review of the literature. Am J Med. 2004;116(Suppl 7A):50s-s57.
Acknowledgements
The authors would like to thank Dr. Runsheng Wang for her advice on the paper. And the authors thank all the 225 centers contributing ChinaSpA registry database as well as all members in ChinaSpA.
Funding
This study, including fees for publication, was supported by Natural Science Foundation of Xinjiang Uygur Autonomous Region (2021D01C136), CAMS Innovation Fund for Medical Sciences (CIFMS) (2021-I2M-1-005), National High Level Hospital Clinical Research Funding (2022-PUMCH-B-013), the Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (2021-RW320-013), Key Research and Development Program of Xinjiang Uygur Autonomous Region (2022B03002-3).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conceptualization, design, and definition of intellectual content. Data acquisition and analysis were performed by HL, QL, XD, SZ, LW, JX, QL, ZW, MY, SL, JS, ML, XZ, and XG. Statistical analyses were performed by YW and JS. The first draft of the manuscript was written by HL, QL, XD, SZ, JS, and ML, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
Hailong Li, Qingyang Li, Xinwang Duan, Shangzhu Zhang, Yanhong Wang, Jian Xu, Qin Li, Lijun Wu, Zhenbiao Wu, Min Yang, Shengyun Liu, Jinmei Su, Mengtao Li, Xiaofeng Zeng and Xiang Gao declare that they have no competing interests.
Ethical Approval
The study was approved by the ethics committee of Peking Union Medical College Hospital, and the study was conducted according to the Helsinki Declaration of 1964 and its later amendments. All participants signed informed consent forms.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Li, H., Li, Q., Duan, X. et al. Anemia and Low Body Mass Index in Axial Spondyloarthritis: Results from ChinaSpA, the Chinese Spondyloarthritis Registry. Rheumatol Ther 11, 397–409 (2024). https://doi.org/10.1007/s40744-024-00646-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-024-00646-5