Abstract
Introduction
The objective of this analysis was to assess disease activity metrics using a variety of disease outcome measures following methotrexate (MTX) withdrawal in ORAL Shift, a phase 3b/4 study of tofacitinib with/without MTX, in patients with rheumatoid arthritis (RA) achieving Clinical Disease Activity Index (CDAI)-defined low disease activity (LDA).
Methods
Patients aged ≥ 18 years with active RA and an inadequate response to MTX received open-label tofacitinib modified-release 11 mg once daily plus MTX for 24 weeks. In the double-blind MTX withdrawal phase, those who had achieved CDAI LDA (≤ 10) at week 24 were randomised 1:1 to receive tofacitinib monotherapy or continued tofacitinib plus MTX. Efficacy analyses were performed in subgroups defined by whether remission and/or LDA had been achieved at week 24 with: Disease Activity Score in 28 joints, erythrocyte sedimentation rate [DAS28-4(ESR)], Routine Assessment of Patient Index Data 3 (RAPID3), CDAI and Simplified Disease Activity Index (SDAI); or DAS28-4[C-reactive protein(CRP)] < 2.4/ < 2.6/ < 2.9/ ≤ 3.2.
Results
Five hundred and thirty patients received treatment in the double-blind MTX withdrawal phase. Proportions of patients achieving each disease activity criterion at week 24 varied by metric. Across disease activity metrics [excluding DAS28-4(ESR) remission], 58–89% of patients per group, and numerically more patients receiving tofacitinib plus MTX, achieved the same criterion at week 48 as at week 24. Differences between groups in least squares mean change from baseline (Δ) DAS28-4(ESR) from week 24–48 favoured tofacitinib plus MTX (nominal p values < 0.05). RAPID3 and DAS28-4(CRP) estimated a higher proportion of patients with acceptable disease state versus DAS28-4(ESR), CDAI remission and SDAI remission.
Conclusion
Response rates at the beginning of the double-blind phase varied across metrics. A consistent trend towards higher response rates with tofacitinib plus MTX was observed across metrics after randomisation, with nominal differences in DAS28-4(ESR) responses. Compared with continued combination therapy, MTX withdrawal did not lead to a clinically meaningful reduction in the response to tofacitinib. DAS28-4(CRP) and RAPID3 were the least stringent metrics.
Trial Registration
ClinicalTrials.gov identifier: NCT02831855.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
In ORAL Shift, discontinuation of methotrexate (MTX) in patients with rheumatoid arthritis (RA) who had achieved Clinical Disease Activity Index (CDAI)-defined low disease activity (LDA) after receiving tofacitinib plus MTX for 24 weeks, resulted in a nominal difference in Disease Activity Score in 28 joints, erythrocyte sedimentation rate [DAS28-4(ESR)] between treatment groups after a further 24 weeks; however, the difference was small and not deemed clinically meaningful. |
This post hoc analysis evaluated the performance of other disease activity metrics, including the Simplified Disease Activity Index (SDAI), Disease Activity Score in 28 joints, C-reactive protein [DAS28-4(CRP)] and Routine Assessment of Patient Index Data 3 (RAPID3), to understand how treatment response rates can vary depending on the measurement used. |
What was learned from the study? |
Following MTX discontinuation, most patients receiving tofacitinib monotherapy after achieving CDAI LDA maintained disease control based on achievement of each disease activity criterion at both week 24 and week 48. |
This post hoc analysis demonstrated variability across RA disease activity metrics in terms of classification into LDA or remission, and as such, should be considered in clinical scenarios. |
Introduction
Rheumatoid arthritis (RA) is a chronic, autoimmune disease primarily affecting the joints, with resultant decline in patient physical function and quality of life [1]. Various treatment guidelines support the use of ‘treat-to-target’, a strategy that involves monitoring RA disease activity systematically over time using validated disease activity metrics and encourages modification of treatment to allow patients to reach a specific pre-defined treatment goal, usually remission, although low disease activity (LDA) is reasonable if remission cannot be achieved [2, 3].
Tofacitinib is an oral Janus kinase inhibitor for the treatment of RA. The phase 3b/4 ORAL Shift study was the first to assess the efficacy and safety of tofacitinib monotherapy with the modified-release 11 mg once daily (QD) formulation, following methotrexate (MTX) withdrawal, versus continued combination therapy, in patients with RA who achieved Clinical Disease Activity Index (CDAI)-defined LDA with tofacitinib plus MTX at week 24 [4]. Tofacitinib monotherapy demonstrated non-inferiority to continued tofacitinib plus MTX, as assessed by the primary endpoint, change from baseline (Δ) in Disease Activity Score in 28 joints, erythrocyte sedimentation rate [DAS28-4(ESR)] from week 24 to week 48, with safety findings consistent with the established safety profile of tofacitinib [4, 5]. The study concluded that withdrawal of MTX may be considered in patients who achieve CDAI LDA over 24 weeks of combination therapy, although a numerically greater proportion of patients maintained DAS28-4(ESR) LDA with continued combination therapy at week 48 [4].
Given that a considerable number of patients with RA discontinue MTX due to intolerance and/or preference [6,7,8], understanding the effectiveness of tofacitinib monotherapy in maintaining disease control following MTX withdrawal is of clinical relevance. ORAL Shift defined the achievement of LDA by utilising CDAI, while the primary endpoint at the end of the double-blind MTX withdrawal phase was the maintenance of LDA utilising DAS28-4(ESR). This raised the question of whether the results would have been different if either CDAI or DAS28-4(ESR) were utilised for both the achievement and maintenance of LDA. In addition, many rheumatologists use other metrics (recommended by the American College of Rheumatology [ACR] [9]) to measure patient response to therapy, including the Simplified Disease Activity Index (SDAI), Routine Assessment of Patient Index Data 3 (RAPID3) and DAS28-4, C-reactive protein (CRP), and it is therefore relevant to understand how these various disease activity metrics would have performed within the context of the ORAL Shift study.
The objective of this post hoc analysis was to assess how the results of the study with these alternative metrics [based on LDA and remission criteria, and also DAS28-4(CRP) < 2.6 and ≤ 3.2] at randomisation (week 24) and week 48 in ORAL Shift would compare with those of the original study.
Methods
Study Design and Patients
Details of the study design and patients of ORAL Shift (NCT02831855) have been published previously [4, 5]. Briefly, ORAL Shift was a 48-week, phase 3b/4, non-inferiority MTX withdrawal study in adult patients with moderate-to-severe RA and an inadequate response to MTX. The study included a screening phase (30 days), an open-label run-in phase (24 weeks), and a randomised, double-blind, placebo-controlled, non-inferiority MTX withdrawal phase (24 weeks), with baseline being defined as day 1 of the open-label phase.
In the open-label phase, patients received tofacitinib modified-release 11 mg QD with MTX. In the double-blind phase, patients were randomised (1:1) to tofacitinib modified-release 11 mg QD plus placebo (tofacitinib monotherapy) or continued with tofacitinib plus MTX until week 48. The mean MTX dose was 16.7 mg/week at baseline and was similar to the baseline values of the tofacitinib monotherapy and tofacitinib plus MTX groups that entered the double-blind phase (16.4 and 16.9 mg/week, respectively) [4].
Achievement of CDAI LDA (≤ 10) at week 24 was the criterion for entry into the double-blind MTX withdrawal phase. Patients who did not achieve CDAI LDA at week 24 were discontinued from the study.
The study was conducted in accordance with the Guidelines for Good Clinical Practice (International Conference on Harmonisation), the Declaration of Helsinki, and local regulatory requirements and laws. The study protocol, any amendments and informed consent documents were reviewed and approved by the institutional review boards and the independent ethics committees of each study centre. All patients provided written informed consent to participate in the study.
Patient and Public Involvement
Patients or the public were not involved in the design, conduct, reporting or dissemination plans of our research.
Disease Activity Metrics and Outcomes
The primary population for this analysis was the full analysis set comprising all patients who had achieved CDAI LDA ≤ 10 at the end of the open-label phase, who were randomised to the double-blind phase and had received at least one dose of study medication.
Eleven disease activity metrics were assessed, as depicted in Fig. 1. These included DAS28-4(CRP) < 2.4 and < 2.9 which have been demonstrated to be equivalent to the DAS28-4(ESR) cut-off points for remission and LDA [10, 11], as well as DAS28-4(CRP) < 2.6 and ≤ 3.2 which have not been validated but are commonly used in rheumatology as the ‘remission’ and ‘LDA’ cut-off points. Validated metrics of LDA were defined as DAS28-4(ESR) ≤ 3.2, SDAI ≤ 11 and RAPID3 ≤ 6, and for remission were defined as (ACR and the European League Against Rheumatism [ACR-EULAR] Boolean remission criteria [12]) DAS28-4(ESR) < 2.6, SDAI ≤ 3.3, CDAI ≤ 2.8 and RAPID3 ≤ 3. For each disease activity metric, the proportion of patients who achieved (and who did not achieve) LDA or remission at weeks 24 and 48 (as defined by the same metric as at week 24), stratified by treatment group, are reported. Continuous metrics were assessed and/or calculated for each study visit as previously described [4]. Binary metrics (e.g. LDA, remission) were derived from the continuous metrics. Non-responder imputation was used for missing data arising from patients who discontinued during the double-blind phase.
Study design. Owing to protocol deviations, six patients who had not achieved CDAI LDA at week 24 were randomised and received treatment. LDA and remission cut-off points for DAS28-4(CRP) (≤ 3.2 and < 2.6, respectively) have not been validated, but are commonly used in rheumatology. CDAI Clinical Disease Activity Index, DAS28-4(CRP) Disease Activity Score in 28 joints, C-reactive protein, DAS28-4(ESR) Disease Activity Score in 28 joints, erythrocyte sedimentation rate, LDA low disease activity, MTX methotrexate, PBO placebo, RAPID3 Routine Assessment of Patient Index Data 3, SDAI Simplified Disease Activity Index
The difference between treatment groups in DAS28-4(ESR) from week 24 to week 48 was also calculated.
Statistical Methods
For each of the 11 disease activity metrics, the proportion of patients in each treatment group achieving that criterion at week 48, a point estimate for the treatment difference, and associated 95% confidence intervals (CIs) were estimated using the normal approximation to the binomial distribution, and nominal p values were calculated with no adjustment for multiplicity. A similar calculation was conducted for the subgroup of patients who did not meet the criterion at week 24 but who did achieve the criterion at week 48.
For the difference between treatment groups in least squares (LS) mean ΔDAS28-4(ESR) from week 24 to week 48, 95% CIs were calculated using a mixed model for repeated measures, which included DAS28-4(ESR) at baseline (defined as the last non-missing measurement on or prior to the first day of tofacitinib dosing in the open-label phase of ORAL Shift) and the use of biologic disease-modifying antirheumatic drugs prior to baseline as covariates, and fixed effects for treatment, visit and treatment by visit interaction. Subject was included as a random effect with an unstructured covariance matrix, and the denominator degrees of freedom were estimated using the Kenward–Roger method [13]. For a given metric, the analysis was carried out for patients meeting the criterion at week 24, and was repeated for patients not meeting the criterion at week 24.
Results
Patients
In total, 694 patients entered the open-label phase of ORAL Shift to receive tofacitinib modified-release 11 mg QD plus MTX for 24 weeks. Of these, 530 patients were randomised and treated in the double-blind phase; 264 patients had MTX withdrawn and replaced with placebo, and 266 patients continued to receive tofacitinib plus MTX (Fig. 1).
Demographics and patient baseline characteristics (measured on day 1 of the open-label phase) have been published previously, and were similar between patients enrolled in the open-label phase, those who achieved CDAI LDA at week 24 and those randomised into the double-blind phase [4]. Briefly, in patients with active RA (and an inadequate response to MTX) receiving tofacitinib monotherapy and tofacitinib plus MTX in the double-blind phase, respectively, mean (standard deviation) DAS28-4(ESR) was 6.0 (0.9) and 6.1 (1.0), DAS28-4(CRP) was 5.2 (0.9) and 5.3 (0.9), CDAI was 33.1 (11.4) and 33.9 (11.6), SDAI was 34.3 (11.7) and 35.0 (12.2), and RAPID3 was 5.3 (1.9) and 5.4 (1.9) at baseline.
Response Rates for Disease Activity Metrics at Week 24
For each disease activity metric, the proportion of patients achieving or not achieving LDA or remission at week 24 as defined above was similar between patients who received tofacitinib plus MTX and patients who received tofacitinib monotherapy (Fig. 2). Of interest, and highlighting the variance of different metrics, only ~ 50% of patients achieving CDAI LDA at week 24 also achieved DAS28-4(ESR) LDA.
Week 24 response rate for each disease activity metric, stratified by treatment group. Proportions calculated based on all patients who were randomised and received treatment in the double-blind phase of ORAL Shift, including six patients who had not achieved CDAI LDA at week 24 but were included due to protocol deviations. The percentages of patients meeting or not meeting criteria at week 24 may not add up to 100% due to missing data. LDA and remission cut-off points for DAS28-4(CRP) (≤ 3.2 and < 2.6, respectively) have not been validated, but are commonly used in rheumatology. CDAI Clinical Disease Activity Index, DAS28-4(CRP) Disease Activity Score in 28 joints, C-reactive protein, DAS28-4(ESR) Disease Activity Score in 28 joints, erythrocyte sedimentation rate, LDA low disease activity, MTX methotrexate, PBO placebo, RAPID3 Routine Assessment of Patient Index Data 3, SDAI Simplified Disease Activity Index
At week 24, over 80% of patients entering the double-blind phase who achieved CDAI LDA also achieved DAS28-4(CRP) ≤ 3.2, SDAI LDA, RAPID3 LDA or RAPID3 remission. Of importance, at week 24, while approximately 55% of patients achieved DAS28-4(CRP) < 2.6 and approximately 80% achieved RAPID3 remission, ≤ 30% of patients achieved DAS28-4(ESR), CDAI or SDAI remission (Fig. 2).
Response Rates for Disease Activity Metrics at Week 48
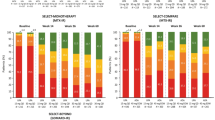
In each treatment group, most patients, who met each disease activity criterion at week 24 also met the same criterion at week 48. Across disease activity metrics [excluding DAS28-4(ESR) remission], 58–89% of patients across the groups achieved the same criterion at week 48 as at week 24; response rates were lower for DAS28-4(ESR) remission (44–54%). Response rates followed the same trend for both treatment groups, across metrics (Fig. 3a).
Week 48 response rate for each disease activity criterion in patients who met the corresponding criterion at week 24 (a), and patients who did not meet the corresponding criterion at week 24 (b), stratified by treatment group. Error bars show 95% CIs estimated using the normal approximation to the binomial distribution; *p < 0.05, **p < 0.01, ***p < 0.001 (nominal p values, not adjusted for multiplicity). Data for DAS28-4(CRP) ≤ 3.2, SDAI (≤ 11.0) and RAPID3 (≤ 6) are not shown in panel (b), due to low patient numbers (N < 30 in each treatment group). LDA and remission cut-off points for DAS28-4(CRP) (≤ 3.2 and < 2.6, respectively) have not been validated, but are commonly used in rheumatology. CDAI Clinical Disease Activity Index, CI confidence interval, DAS28-4(CRP) Disease Activity Score in 28 joints, C-reactive protein, DAS28-4(ESR) Disease Activity Score in 28 joints, erythrocyte sedimentation rate, LDA low disease activity, MTX methotrexate, PBO placebo, RAPID3 Routine Assessment of Patient Index Data 3, SDAI Simplified Disease Activity Index
A high number of patients achieved RAPID3 LDA and remission cut-off points compared with all other metrics. In addition, as has been shown previously [10, 11], more patients achieved the cut-off points of < 2.6 and ≤ 3.2 with DAS28-4(CRP) compared with DAS28-4(ESR) (Fig. 3a).
Numerically more patients receiving tofacitinib plus MTX compared with tofacitinib monotherapy who met each disease activity criterion at week 24 continued to meet the criterion at week 48 (Fig. 3a). Differences between treatment groups were greatest for DAS28-4(CRP) ≤ 3.2, CDAI LDA, SDAI LDA and RAPID3 remission (nominal p value < 0.05).
Among patients who did not meet disease activity criteria at week 24, generally, a minority met these criteria at week 48 (Fig. 3b). Numerically more patients receiving tofacitinib plus MTX compared with tofacitinib monotherapy who did not meet disease activity criteria at week 24, met them at week 48 (Fig. 3b).
Differences Between Treatment Groups in DAS28-4 from Week 24 to Week 48
Among patients who met each disease activity criterion at week 24, in each subgroup, differences between treatment groups in LS mean ΔDAS28-4(ESR) (Fig. 4) from week 24 to week 48 favoured tofacitinib plus MTX compared with tofacitinib monotherapy (nominal p value < 0.05). However, in all instances the differences between treatment groups were smaller than 0.6, and less than the minimal clinically important difference of 1.2 for DAS28-4(ESR) [14].
Difference between treatment groups in LS mean ΔDAS28-4(ESR) from week 24 to week 48, stratified by disease activity criterion met at week 24. Nominal p values were calculated for tofacitinib plus placebo (PBO) versus tofacitinib plus MTX, with no adjustment for multiplicity. LS mean ΔDAS28-4(ESR) from week 24 to week 48 and 95% CIs for the difference between treatment groups were calculated using a mixed model for repeated measures. Δ change from baseline, CDAI Clinical Disease Activity Index, CI confidence interval, DAS28-4(CRP) Disease Activity Score in 28 joints, C-reactive protein, DAS28-4(ESR) Disease Activity Score in 28 joints, erythrocyte sedimentation rate, LDA low disease activity, LS least squares, MTX methotrexate, PBO placebo, RAPID3 Routine Assessment of Patient Index Data 3, SDAI Simplified Disease Activity Index
Discussion
ORAL Shift previously demonstrated that withdrawal of MTX may be considered in patients who achieve CDAI LDA after receiving tofacitinib modified-release 11 mg QD plus MTX, without loss of clinical effectiveness [4].
The use of CDAI to define achievement of LDA in ORAL Shift enabled investigators to rapidly assess disease activity at randomisation without a requirement for laboratory-based assessments. This post hoc analysis explored whether the results of ORAL Shift would have been different if other disease activity metrics, including DAS28-4(ESR), DAS28-4(CRP), CDAI, SDAI and RAPID3, had been utilised for both the achievement and maintenance of LDA. Regardless of the disease activity criterion met at week 24, most patients achieved the corresponding criterion at week 48 with or without continued MTX treatment, with the exception of DAS28-4(ESR) remission in patients receiving tofacitinib monotherapy. This finding suggests that the results of ORAL Shift would be valid if any of the above metrics had been used. Consistent with the trend reported in the primary analysis [4], numerically more patients receiving tofacitinib plus MTX achieved each criterion compared with those receiving tofacitinib monotherapy at week 48.
It is important to note that there was a difference in the proportions of patients achieving LDA and remission between different disease activity metrics. The least stringent metrics were RAPID3 and DAS28-4(CRP), and the most stringent were DAS28-4(ESR), CDAI remission and SDAI remission. To achieve the goal of reducing disease activity to the lowest level possible [15, 16], these results suggest that utilising the metrics of DAS28-4(ESR) or CDAI or SDAI remission is preferable to utilising RAPID3 or DAS28-4(CRP), particularly when applying the validated cut-offs for DAS28-4(ESR) to DAS28-4(CRP) scores. Another study has also shown that DAS28(CRP) ‘remission’ is less stringent than SDAI/CDAI remission [17]. Furthermore, variability between the disease activity metrics suggests that the same instrument should be used over time.
Of the patients who achieved LDA at week 24 and week 48, the proportion achieving DAS28-4(ESR) LDA was lower compared with the proportion achieving DAS28-4(CRP) ≤ 3.2, CDAI LDA and SDAI LDA, consistent with a previous analysis from the tofacitinib clinical trials database [18]. Of note, it is known that DAS28-4(CRP) overestimates disease control when applying remission and LDA cut-off points that were previously validated for DAS28-4(ESR) in patients with RA, regardless of treatment [11]. Further analyses should explore the reason for the variance between CDAI and DAS28-4(ESR). Preliminarily, this may be due to the substantial differences between DAS28-4(ESR) and CDAI, such as not including an acute phase reactant and the equal weighting of each of the four components in the CDAI, in contrast to the inclusion of an acute phase reactant and the unequal weighting of the components in DAS28-4(ESR) [19].
Notably, for patients with CDAI LDA but not DAS28-4(ESR) LDA at week 24, approximately 30% achieved LDA by week 48, whether MTX was discontinued or not. DAS28-4(ESR) remission was consistent with the proportion of patients achieving CDAI and SDAI remission.
Among patients who did not meet disease activity criterion at week 24, generally, a minority met the criterion at week 48, irrespective of whether MTX had been withdrawn. This analysis did not evaluate whether patients had continual, but slower improvement, from week 0 to week 24 (e.g. CDAI improved but was ≤ 10 at week 24). Therefore, these patients most likely had further improvement from week 24 to week 48.
Differences between treatment groups in LS mean ΔDAS28-4(ESR) from week 24 to week 48 favoured tofacitinib plus MTX, and were consistent with the primary data from ORAL Shift [4]. However, in patients who met each disease activity criterion at week 24, differences in LS mean ΔDAS28-4(ESR) between tofacitinib monotherapy and tofacitinib plus MTX were < 0.6, which is less than the minimal clinically important difference of 1.2 for DAS28-4(ESR) [14].
A strength of this post hoc analysis was the ability to assess alternative disease activity metrics, expanding upon the published data [4, 5]. The limitations of this analysis were the post hoc nature, the small patient numbers in some groups and that the inference for the double-blind phase was, out of necessity, limited to the randomised cohort based on patients achieving CDAI LDA, limiting data analysis and interpretation to that randomised cohort. Response rates for each treatment group would have likely varied had patients been selected for randomisation in the double-blind phase based on any one of the metrics considered. However, it is not clear for which metrics this would have resulted in a clinically meaningful difference between patients who continued on tofacitinib plus MTX versus those on tofacitinib monotherapy.
Conclusions
This post hoc analysis of data from randomised patients with active RA in ORAL Shift demonstrated that, regardless of the metric used for the disease activity state at randomisation, generally, most patients in both treatment groups met the same disease control criteria at week 48. We have further shown that disease state response rates varied across metrics. A consistent trend towards higher response rates with tofacitinib plus MTX compared with tofacitinib monotherapy was observed across metrics after randomisation, with nominal differences in DAS28-4(ESR) responses. Compared with continued combination therapy, withdrawal of MTX did not, however, lead to a clinically meaningful reduction in the response to tofacitinib. Based on the current analysis with tofacitinib in a randomised MTX withdrawal context, DAS28-4(ESR), CDAI remission and SDAI remission are the metrics most likely to reflect actual disease activity, and are therefore the preferred metrics to use, compared with DAS28-4(CRP) [particularly when using the DAS28-4(ESR) validated cut-offs] and RAPID3.
References
Smolen JS, Aletaha D, McInnes IB. Rheumatoid arthritis. Lancet. 2016;388:2023–38.
Fraenkel L, Bathon JM, England BR, et al. 2021 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Rheumatol. 2021;73:1108–23.
Smolen JS, Landewé RBM, Bijlsma JWJ, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis. 2020;79:685–99.
Cohen SB, Pope J, Haraoui B, et al. Methotrexate withdrawal in patients with rheumatoid arthritis who achieve low disease activity with tofacitinib modified-release 11 mg once daily plus methotrexate (ORAL Shift): a randomised, phase 3b/4, non-inferiority trial. Lancet Rheumatol. 2019;1:E23–34.
Cohen SB, Pope J, Haraoui B, et al. Efficacy and safety of tofacitinib modified-release 11 mg once daily plus methotrexate in adult patients with rheumatoid arthritis: 24-week open-label phase results from a phase 3b/4 methotrexate withdrawal non-inferiority study (ORAL Shift). RMD Open. 2021;7:e001673.
DiBenedetti DB, Zhou X, Reynolds M, Ogale S, Best JH. Assessing methotrexate adherence in rheumatoid arthritis: a cross-sectional survey. Rheumatol Ther. 2015;2:73–84.
Galloway J, Dikranian A, Koehn CL, Gruben D, Woolcott J, Strengholt S. AB0247 Insights into adherence and patient-initiated monotherapy for rheumatoid arthritis via a global survey of patients, caregivers and physicians [abstract]. Ann Rheum Dis. 2019;78:A1580.
Curtis JR, Bykerk VP, Aassi M, Schiff M. Adherence and persistence with methotrexate in rheumatoid arthritis: a systematic review. J Rheumatol. 2016;43:1997–2009.
Anderson J, Caplan L, Yazdany J, et al. Rheumatoid arthritis disease activity measures: American College of Rheumatology recommendations for use in clinical practice. Arthritis Care Res (Hoboken). 2012;64:640–7.
Fleischmann RM, van der Heijde D, Gardiner PV, Szumski A, Marshall L, Bananis E. DAS28-CRP and DAS28-ESR cut-offs for high disease activity in rheumatoid arthritis are not interchangeable. RMD Open. 2017;3:e000382.
Fleischmann R, van der Heijde D, Koenig AS, et al. How much does Disease Activity Score in 28 joints ESR and CRP calculations underestimate disease activity compared with the Simplified Disease Activity Index? Ann Rheum Dis. 2015;74:1132–7.
Felson DT, Smolen JS, Wells G, et al. American College of Rheumatology/European League Against Rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Arthritis Rheum. 2011;63:573–86.
Kenward MG, Roger JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53:983–97.
Ward MM, Guthrie LC, Alba MI. Clinically important changes in individual and composite measures of rheumatoid arthritis activity: thresholds applicable in clinical trials. Ann Rheum Dis. 2015;74:1691–6.
Smolen JS, Breedveld FC, Burmester GR, et al. Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international task force. Ann Rheum Dis. 2016;75:3–15.
Ramiro S, Landewe RB, van der Heijde D, et al. Is treat-to-target really working in rheumatoid arthritis? A longitudinal analysis of a cohort of patients treated in daily practice (RA BIODAM). Ann Rheum Dis. 2020;79:453–9.
Klarenbeek NB, Koevoets R, van der Heijde DM, et al. Association with joint damage and physical functioning of nine composite indices and the 2011 ACR/EULAR remission criteria in rheumatoid arthritis. Ann Rheum Dis. 2011;70:1815–21.
Smolen JS, Aletaha D, Gruben D, Zwillich SH, Krishnaswami S, Mebus C. Remission rates with tofacitinib treatment in rheumatoid arthritis: a comparison of various remission criteria. Arthritis Rheumatol. 2017;69:728–34.
Anderson JK, Zimmerman L, Caplan L, Michaud K. Measures of rheumatoid arthritis disease activity: Patient (PtGA) and Provider (PrGA) Global Assessment of Disease Activity, Disease Activity Score (DAS) and Disease Activity Score with 28-Joint Counts (DAS28), Simplified Disease Activity Index (SDAI), Clinical Disease Activity Index (CDAI), Patient Activity Score (PAS) and Patient Activity Score-II (PASII), Routine Assessment of Patient Index Data (RAPID), Rheumatoid Arthritis Disease Activity Index (RADAI) and Rheumatoid Arthritis Disease Activity Index-5 (RADAI-5), Chronic Arthritis Systemic Index (CASI), Patient-Based Disease Activity Score with ESR (PDAS1) and Patient-Based Disease Activity Score without ESR (PDAS2), and Mean Overall Index for Rheumatoid Arthritis (MOI-RA). Arthritis Care Res (Hoboken). 2011;63(Suppl 11):S14–36.
Fleischmann R, Haraoui B, Buch M, et al. POS0086 Analysis of disease activity measures in the context of a methotrexate withdrawal study among patients with rheumatoid arthritis treated with tofacitinib 11 mg once daily + methotrexate: post hoc analysis of data from ORAL Shift [abstract]. Ann Rheum Dis. 2021;80:251.
Acknowledgements
The authors would like to thank the patients and study investigators for their contributions.
Funding
This study was sponsored by Pfizer Inc, New York, NY, USA. Pfizer Inc funded the journal’s Rapid Service Fee.
Medical Writing Assistance
Medical writing support, under the direction of the authors, was provided by Kimberley Haines, MSc, CMC Connect, a division of IPG Health Medical Communications, funded by Pfizer Inc, New York, NY, USA in accordance with Good Publication Practice (GPP 2022) guidelines (Ann Intern Med 2022; 175(9):1298–1304).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole and have given their approval for this version to be published.
Author Contributions
All authors contributed to the data interpretation, critically reviewed the manuscript and approved the final version for submission. Boulos Haraoui, David Gold, Gosford Sawyerr, Harry Shi, Annette Diehl and Kristen Lee also contributed to the study conception and design. Roy Fleischmann, Gosford Sawyerr, Harry Shi, Annette Diehl and Kristen Lee also contributed to the data acquisition. Roy Fleischmann, David Gold, Gosford Sawyerr, Harry Shi, Annette Diehl and Kristen Lee also contributed to the data analysis.
Prior Presentation
This work was previously presented at EULAR European Congress of Rheumatology, 2021 [20].
Disclosures
Roy Fleischmann has received grants and/or research support from AbbVie, Amgen, AstraZeneca, Bristol Myers Squibb, Eli Lilly, Galvani, Genentech, Gilead, GlaxoSmithKline, Horizon, Janssen, Novartis, Pfizer Inc, Samumed, Sanofi-Aventis, TEVA, UCB, Viela and VORSO; has acted as a consultant for AbbVie, Amgen, Bristol Myers Squibb, Eli Lilly, Galvani, Gilead, GlaxoSmithKline, Janssen, Novartis, Pfizer Inc, Sanofi-Aventis and UCB; and has participated in a speakers’ bureau for AbbVie and Pfizer Inc. Boulos Haraoui has received grants and/or research support from AbbVie; has acted as a consultant for AbbVie, Amgen, Eli Lilly, Merck, Pfizer Inc and UCB; and has participated in speakers’ bureaus for Amgen, Pfizer Inc and UCB. Maya H. Buch has received grants and/or research support from Gilead, Pfizer Inc and UCB; has acted as a consultant for AbbVie, Eli Lilly, Gilead, MSD and Pfizer Inc; has participated in a speakers’ bureau for AbbVie (paid to host institution); and is in receipt of a National Institute of Health and Care Research (NIHR) Senior Investigator Award (Disclaimer: The views expressed are those of the author and not necessarily those of the NIHR or the Department of Health and Social Care). David Gold, Harry Shi, Annette Diehl and Kristen Lee are employees and shareholders of Pfizer Inc. Gosford Sawyerr is an employee of Syneos Health Inc, which was a paid contractor to Pfizer Inc in the development of this manuscript.
Compliance with Ethics Guidelines
The study was conducted in accordance with the Guidelines for Good Clinical Practice (International Conference on Harmonisation), the Declaration of Helsinki and local regulatory requirements and laws. The study protocol, any amendments and informed consent documents were reviewed and approved by the institutional review boards and the independent ethics committees of each study centre. Further ethical approval was not required for this post hoc analysis. All patients provided written informed consent to participate in the study.
Data Availability
Upon request, and subject to review, Pfizer will provide the data that support the findings of this study. Subject to certain criteria, conditions and exceptions, Pfizer may also provide access to the related individual de-identified participant data. See https://www.pfizer.com/science/clinical-trials/trial-data-and-results for more information.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Fleischmann, R., Haraoui, B., Buch, M.H. et al. Analysis of Disease Activity Metrics in a Methotrexate Withdrawal Study among Patients with Rheumatoid Arthritis Treated with Tofacitinib plus Methotrexate. Rheumatol Ther 10, 375–386 (2023). https://doi.org/10.1007/s40744-022-00511-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-022-00511-3