Abstract
Purpose
The aim of the study was to describe the spontaneous TSH level variations and levothyroxine dose adjustments in athyreotic patients with differentiated thyroid cancer (DTC) in real-life practice.
Methods
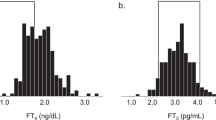
Patients with DTC were retrospectively evaluated at a tertiary referral center between October 2006 and November 2013. Hormone measurements (TSH and FT4 serum levels), L-T4 prescription information (dose per kg per day) and other medications were recorded at 1 month and 3, 12, 24, 36 and 48 months after primary treatment (surgery ± radioiodine therapy).
Results
The cohort was composed of 452 patients; about 20% of patients with stable levothyroxine dose have clinically meaningful spontaneous TSH variations (defined as ΔTSH > 2 mcUI/mL) at yearly follow-up visit. Furthermore, about 25% of athyreotic DTC patients with stable dose have a ΔTSH > 1.5 mcUI/mL and about 40% a ΔTSH > 1 mcUI/mL during each follow-up visit. We further investigated whether this TSH variation would lead to subsequent dose changes. About 19.9–37.7% of DTC patients on stable LT4 dose on the previous visit had their levothyroxine dose reduced, while 7.8–14.9% increased due to TSH variations. We further evaluated the decision to change the dose in relation with the age-specific TSH range. Up to 77.2% of patients had their dose adjusted due to TSH falling below the age-specific range.
Conclusions
Spontaneous serum TSH variations determine levothyroxine replacement therapy in athyreotic patients with DTC, requiring multiple dose changes.
Similar content being viewed by others
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
References
Jonklaas J, Bianco AC, Bauer AJ et al (2014) Guidelines for the treatment of hypothyroidism: prepared by the american thyroid association task force on thyroid hormone replacement. Thyroid 24:1670–1751. https://doi.org/10.1089/thy.2014.0028
Del Duca SC, Santaguida MG, Brusca N et al (2015) Individually-tailored thyroxine requirement in the same patients before and after thyroidectomy: a longitudinal study. Eur J Endocrinol 173:351–357. https://doi.org/10.1530/EJE-15-0314
Lamartina L, Grani G, Durante C, Filetti S (2018) Recent advances in managing differentiated thyroid cancer [version 1; referees: 2 approved]. F1000Research 7:86. https://doi.org/10.12688/f1000research.12811.1
Ernst FR, Barr P, Elmor R et al (2017) The economic impact of levothyroxine dose adjustments: the CONTROL HE study. Clin Drug Investig 37:71–83. https://doi.org/10.1007/s40261-016-0462-3
Taylor PN, Iqbal A, Minassian C et al (2014) Falling threshold for treatment of borderline elevated thyrotropin levels-balancing benefits and risks: evidence from a large community-based study. JAMA Intern Med 174:32–39. https://doi.org/10.1001/jamainternmed.2013.11312
Lamartina L, Durante C, Lucisano G et al (2017) Are evidence-based guidelines reflected in clinical practice? An analysis of prospectively collected data of the italian thyroid cancer observatory. Thyroid 27:1490–1497. https://doi.org/10.1089/thy.2017.0299
Zatelli MC, Lamartina L, Meringolo D et al (2018) Thyroid nodule recurrence following lobo-isthmectomy: incidence, patient’s characteristics, and risk factors. J Endocrinol Invest 41:1469–1475. https://doi.org/10.1007/s40618-018-0946-5
Lamartina L, Montesano T, Falcone R et al (2019) Is it worth suppressing TSH in low- and intermediate-risk papillary thyroid cancer patients before the first disease assessment? Endocr Pract 25:165–169. https://doi.org/10.4158/EP-2018-0393
Lamartina L, Grani G, Durante C et al (2018) Follow-up of differentiated thyroid cancer—what should (and what should not) be done. Nat Rev Endocrinol 14:538–551. https://doi.org/10.1038/s41574-018-0068-3
Roelfsema F, Pereira AM, Veldhuis JD et al (2009) Thyrotropin secretion profiles are not different in men and women. J Clin Endocrinol Metab 94:3964–3967. https://doi.org/10.1210/jc.2009-1155
Sviridonova MA, Fadeyev VV, Sych YP, Melnichenko GA (2013) Clinical significance of TSH circadian variability in patients with hypothyroidism. Endocr Res 38:24–31. https://doi.org/10.3109/07435800.2012.710696
Ehrenkranz J, Bach PR, Snow GL et al (2015) Circadian and circannual rhythms in thyroid hormones: determining the TSH and free T4 reference intervals based upon time of day, age, and sex. Thyroid 25:954–961. https://doi.org/10.1089/thy.2014.0589
Gullo D, Latina A, Frasca F et al (2017) Seasonal variations in TSH serum levels in athyreotic patients under l-thyroxine replacement monotherapy. Clin Endocrinol (Oxf) 87:207–215. https://doi.org/10.1111/cen.13351
Andersen S, Pedersen KM, Bruun NH, Laurberg P (2002) Narrow individual variations in serum T(4) and T(3) in normal subjects: a clue to the understanding of subclinical thyroid disease. J Clin Endocrinol Metab 87:1068–1072
Vadiveloo T, Donnan PT, Murphy MJ, Leese GP (2013) Age- and gender-specific TSH reference intervals in people with no obvious thyroid disease in Tayside, Scotland: the Thyroid Epidemiology, Audit, and Research Study (TEARS). J Clin Endocrinol Metab 98:1147–1153. https://doi.org/10.1210/jc.2012-3191
Klein Hesselink EN, Klein Hesselink MS, de Bock GH et al (2013) Long-term cardiovascular mortality in patients with differentiated thyroid carcinoma: an observational study. J Clin Oncol 31:4046–4053. https://doi.org/10.1200/jco.2013.49.1043
Samuels MH (2014) Thyroid disease and cognition. Endocrinol Metab Clin N Am 43:529–543. https://doi.org/10.1016/j.ecl.2014.02.006
Pollock MA, Sturrock A, Marshall K et al (2001) Thyroxine treatment in patients with symptoms of hypothyroidism but thyroid function tests within the reference range: randomised double blind placebo controlled crossover trial. BMJ 323:891–895
Walsh JP, Ward LC, Burke V et al (2006) Small changes in thyroxine dosage do not produce measurable changes in hypothyroid symptoms, well-being, or quality of life: results of a double-blind, randomized clinical trial. J Clin Endocrinol Metab 91:2624–2630. https://doi.org/10.1210/jc.2006-0099
Jorde R, Waterloo K, Storhaug H et al (2006) Neuropsychological function and symptoms in subjects with subclinical hypothyroidism and the effect of thyroxine treatment. J Clin Endocrinol Metab 91:145–153. https://doi.org/10.1210/jc.2005-1775
Samuels MH, Kolobova I, Niederhausen M et al (2018) Effects of altering levothyroxine (L-T4) doses on quality of life, mood, and cognition in L-T4 treated subjects. J Clin Endocrinol Metab 103:1997–2008. https://doi.org/10.1210/jc.2017-02668
Santini F, Pinchera A, Marsili A et al (2005) Lean body mass is a major determinant of levothyroxine dosage in the treatment of thyroid diseases. J Clin Endocrinol Metab 90:124–127
Torlontano M, Durante C, Torrente I et al (2008) Type 2 deiodinase polymorphism (threonine 92 alanine) predicts l-thyroxine dose to achieve target thyrotropin levels in thyroidectomized patients. J Clin Endocrinol Metab 93:910–913. https://doi.org/10.1210/jc.2007-1067
Loh JA, Wartofsky L, Jonklaas J, Burman KD (2009) The magnitude of increased levothyroxine requirements in hypothyroid pregnant women depends upon the etiology of the hypothyroidism. Thyroid 19:269–275. https://doi.org/10.1089/thy.2008.0413
Baehr KM, Lyden E, Treude K et al (2012) Levothyroxine dose following thyroidectomy is affected by more than just body weight. Laryngoscope 122:834–838. https://doi.org/10.1002/lary.23186
Younis IR, Ahmed MA, Burman KD et al (2018) Stable isotope pharmacokinetic studies provide insight into effects of age, sex, and weight on levothyroxine metabolism. Thyroid 28:41–49. https://doi.org/10.1089/thy.2017.0380
Acknowledgements
GG, VR and RF and contributed to this paper as part of their PhD studies in Biotechnologies and Clinical Medicine at the University of Rome, Sapienza. The study was supported by the Fondazione Umberto Di Mario ONLUS and Banca d’ Italia.
Funding
The study was supported by the Fondazione Umberto Di Mario ONLUS and Banca d’ Italia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional ethics committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Thyroid cancer patient data were collected at our site, after obtaining the informed consent of the patients and approval of the local ethics committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Grani, G., Tumino, D., Ramundo, V. et al. Changes in TSH levels in athyreotic patients with differentiated thyroid cancer during levothyroxine therapy: influence on dose adjustments. J Endocrinol Invest 42, 1485–1490 (2019). https://doi.org/10.1007/s40618-019-01074-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-019-01074-x