Abstract
Background
Antithyroid drugs (ATDs) are first-line treatment for Graves’ hyperthyroidism worldwide, but relapses are frequent. The reliability of individual risk factors to predict at baseline subsequent relapse is poor. Predictive scores grouping single risk factors might help to select the best treatment (pharmacological vs. ablative).
Objective
To assess the predictivity of a recently developed score (Clinical Severity Score, CSS) and to compare it with another score (GREAT score).
Patients
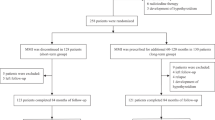
A retrospective observational, single-center study was conducted of 387 consecutive, newly diagnosed Graves’ patients, who completed an 18–24 months ATD course and were followed for at least 2 years.
Results
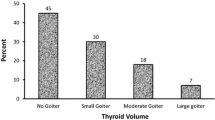
Hyperthyroidism relapsed in 185 patients (48%). At diagnosis and before treatment, the relapse group had higher serum TSH-receptor antibody and free thyroxine levels and larger goiters than the remission group, with no differences in Graves’ orbitopathy prevalence and severity. In the multivariate analyses, only large goiter size was significantly associated with an increased recurrence hazard ratio. Using CSS, the risk of relapse increased from 36% in the mild category and 49% in the moderate category to 59% in the severe category, with quite a good area under the curve (AUC) (0.60; 95% CI: 0.55; 0.66). GREAT score showed an increase in relapse from 34% for class I (mild) and 49% for class II (moderate) to 64% for class III (severe) (AUC, 0.63; CI: 0.58; 0.68).
Conclusions
Both CSS and GREAT score are useful, although imperfect, tools to predict at baseline relapse of hyperthyroidism after treatment. In real life they may help the clinician to tailor a treatment for newly diagnosed Graves’ hyperthyroidism.



Similar content being viewed by others
References
Bartalena L (2013) Diagnosis and management of Graves disease: a global overview. Nat Rev Endocrinol 9(12):724–734
Smith TJ, Hegedus L (2016) Graves’ disease. N Engl J Med 375(16):1552–1565
Burch HB, Burman KD, Cooper DS (2012) A 2011 survey of clinical practice patterns in the management of Graves’ disease. J Clin Endocrinol Metab 97(12):4549–4558
Bartalena L, Burch HB, Burman KD, Kahaly GJ (2016) A 2013 European survey of clinical practice patterns in the management of Graves’ disease. Clin Endocrinol (Oxf) 84(1):115–120
Brito Jp, Schilz S, Singh Ospina N, Rodriguez-Gutierrez R, Maraka S, Sangaralingham LR, Montori VM (2016) Antithyroid drugs the most common treatment for Graves’ disease in the United States: a nationwide population-based study. Thyroid 26(8):1144–1445
Bartalena L, Chiovato L, Vitti P (2016) Management of hyperthyroidism due to Graves’ disease: frequently asked questions and answers (if any). J Endocrinol Invest 39(10):1105–1114
Piantanida E, Lai A, Sassi L, Gallo D, Spreafico E, Tanda ML, Bartalena L (2015) Outcome prediction of treatment of Graves’ hyperthyroidism with antithyroid drugs. Horm Metab Res 47(10):767–772
Struja T, Fehlberg H, Kutz A, Guebelin L, Degen C, Muller B, Schuez P (2017) Can we predict relapse in Graves’ disease? Results from a systematic review and meta-analysis. Eur J Endocrinol 176(1):87–97
Vos XG, Endert E, Zwinderman AH, Tijssen JGP, Wiersinga WM (2016) Predicting the risk of recurrence before the start of antithyroid drug therapy in patients with Graves’ hyperthyroidism. J Clin Endocrinol Metab 101(4):1381–1389
Struja T, Kaeslin M, Boesiger F, Jutzi R, Imahorn N, Kutz A, Bernasconi L, Mundwiler E, Mueller B, Christ-Crain M, Meinenberg F, Ebrahimi F, Henzen C, Fischli S, Kraenzlin M, Meier C, Schuetz P (2017) External validation of the GREAT score to predict relapse risk in Graves’ disease: results from a multicenter, retrospective study with 741 patients. Eur J Endocrinol 176(4):413–419
Bartalena L, Masiello E, Magri F, Veronesi G, Bianconi E, Zerbini F, Gaiti M, Spreafico E, Gallo D, Premoli P, Piantanida E, Tanda ML, Ferrario M, Vitti P, Chiovato L (2016) The phenotype of newly diagnosed Graves’ disease in Italy in recent years is milder than in the past: results of a large observational longitudinal study. J Endocrinol Invest 39(12):1445–1451
Bartalena L, Baldeschi L, Boboridis K, Eckstein A, Kahaly GJ, Marcocci C, Perros P, Salvi M, Wiersinga WM on behalf of the European Group on Graves’ Orbitopathy (EUGOGO) (2016) The 2016 European Thyroid Association/European Group on Graves’ orbitopathy guidelines for the management of Graves’ orbitopathy. Eur Thyroid J 5(1):9–26
Vitti P, Rago T, Chiovato L, Pallini S, Santini S, Fiore E, Rocchi R, Martino E, Pinchera A (1997) Clinical features of patients with Graves’ disease undergoing remission after antithyroid drug treatment. Thyroid 7(3):369–375
Hussain YS, Hookman JCm, Allahabadia A, Balasubramanian SP (2017) Epidemiology, management and outcomes of Graves’ disease real life data. Endocrine 56(3):568–578
Acknowledgements
This study was partly supported by grants from the Ministry of Education, University and Research (MIUR, Rome; PRIN 2015HPMLFY-009 and PRIN 2012Z3F7HE-006) to Luigi Bartalena.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors state that they have no conflict of interest.
Ethical approval
All procedures performed during this retrospective study were in accordance with the ethical standards of institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The ethical committee approval is not required for retrospective studies.
Informed consent
For this type of retrospective study formal consent is not required. Data were anonymized.
Rights and permissions
About this article
Cite this article
Masiello, E., Veronesi, G., Gallo, D. et al. Antithyroid drug treatment for Graves’ disease: baseline predictive models of relapse after treatment for a patient-tailored management. J Endocrinol Invest 41, 1425–1432 (2018). https://doi.org/10.1007/s40618-018-0918-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-018-0918-9