Abstract
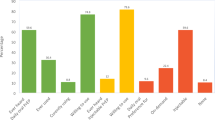
Pre-exposure prophylaxis (PrEP) is an effective tool in protecting persons from acquiring HIV infection through sex or injection drug use. However, awareness and willingness to use PrEP among Black gay, bisexual, and other men who have sex with men (BMSM) remain suboptimal compared to White MSM (WMSM) in the United States. Our aims were to (1) assess the factors associated with PrEP awareness and willingness to use PrEP among MSM and (2) compare the PrEP perceptions among BMSM versus non-Black MSM. Data were drawn from two cross-sectional behavioral surveys in Baltimore, MD: Behavioral Surveillance Research (BESURE) conducted in 2017, and Safe Spaces 4 Sexual Health (SS4SH), conducted in 2018 and 2019. Descriptive statistics were used to summarize the study population. We used Poisson regression models to identify variables associated with awareness of PrEP and willingness to use PrEP. PrEP perceptions were assessed via 13 items scored on a 5-point Likert scale. Finally, we conducted a post-hoc exploratory bivariate analysis of the relationship between PrEP perception and willingness to use PrEP, stratified by race/ethnicity. A total of 261 MSM participated in this study. Many of the participants were aware of PrEP (75.1%). Factors associated with greater PrEP awareness included having greater than a high school education (aRR 1.22, 95% CI 1.04, 1.43); and earning more than $25,000 annually (aRR 1.24, 95% CI 1.08, 1.42). Participants who had received money in exchange for sex one or more times were less likely to be aware of PrEP (aRR 0.59, 95% CI 0.36, 0.95). More than half of the participants were willing to use PrEP (55.3%). In bivariate and multivariable analyses, demographic or behavioral characteristics were not significantly associated with willingness to use PrEP. Higher agreement with the following statements was associated with lower willingness to use PrEP: “Having to take a pill every day is difficult” (RR 0.89, 95% CI 0.82–0.97) and, “I am concerned about the side effects of PrEP” (RR 0.89, 95% CI 0.82–0.96), and “PrEP is for people who have riskier sex lives than I do” (RR 0.86, 95% CI 0.78–0.95). Conversely, higher willingness to use PrEP was associated with comfortable having sex without a condom (RR 1.11, 95% CI 1.02–1.21), less anxious about sex (RR 1.12, 95% CI 1.02–1.24), and my friends think that I should take PrEP (RR 1.19, 95% CI 1.07–1.32). We found BMSM compared to non-Black MSM had higher mean scores related to taking a daily pill (p = 0.041), concerns about side effects (p = 0.012), concerns about people thinking they had HIV (p = 0.001), concerns about the financial costs of PrEP (p = 0.038) and caution when dealing with healthcare organizations/medical mistrust (p = 0.019). Perceptions with a statistically significant lower score among BMSM versus non-Black MSM included statements such as, comfortable having sex without a condom (p = 0.003) and less anxious about sex (p < 0.001). We conclude HIV prevention strategies, programs, and interventions should be cognizant of PrEP perceptions that facilitate or hinder PrEP uptake in Baltimore City, MD.
Similar content being viewed by others
Data Availability
Not applicable.
Code Availability
The dataset is not available for use.
References
Centers for disease control and prevention. HIV surveillance report. 2020;33. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Accessed 22 Feb 2024.
Baltimore city annual HIV epidemiological profile 2020. Center for HIV surveillance, epidemiology and evaluation, Maryland department of health, Baltimore, MD. 2021. HIV-Annual-Epidemiological-Profile-2019 https://maryland.gov. Accessed 26 Feb 2024.
Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV epidemic: a plan for the United States. JAMA. 2019;321(9):844–5. https://doi.org/10.1001/jama.2019.1343.
U.S. Department of Health and Human Services. 2021. HIV national strategic plan for the United States: a roadmap to end the epidemic 2021–2025. Washington, DC. https://files.hiv.gov/s3fs-public/HIV-National-Strategic-Plan-2021-2025.pdf. Accessed 02.19.2021
Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99. https://doi.org/10.1056/NEJMoa1011205.
Baeten JM, Donnell D, Ndase P, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410. https://doi.org/10.1056/NEJMoa1108524.
Thigpen MC, Kebaabetswe PM, Paxton LA, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367(5):423–34. https://doi.org/10.1056/NEJMoa1110711.
Centers for disease control and prevention. US public health service: preexposure prophylaxis for the prevention of HIV infection in the United States - 2021 Update: a clinical practice guideline. 2021. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf . Accessed 22 Feb 2024.
Choopanya K, Martin M, Suntharasamai P, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–90. https://doi.org/10.1016/S0140-6736(13)61127-7.
Food and Drug Administration. FDA approves first drug for reducing the risk of sexually acquired HIV infection. Silver Spring, MD: US Department of Health and Human Services, Food and Drug Administration; 2012. Truvada for PrEP Fact Sheet: Enduring Safe and Proper Use (fda.gov) Accessed 12.19.2022
Centers for Disease Control and Prevention: US Public Health Service: preexposure prophylaxis for the prevention of HIV infection in the United States—2021 Update: a clinical practice guideline. PrEP Guideline 2021 Update (cdc.gov) Accessed 01.142022
US Preventive Services Task Force, Owens DK, Davidson KW, et al. Preexposure prophylaxis for the prevention of HIV infection: US preventive services task force recommendation statement. JAMA. 2019;321(22):2203–13. https://doi.org/10.1001/jama.2019.6390.
Gilead sciences Inc. U.S. food and drug administration approves expanded indication for Truvada (emtricitabine and tenofovir disoproxil fumarate) for reducing the risk of acquiring HIV-1 in adolescents [Press release]. Foster City, CA: Gilead Sciences Inc.; 2018. https://www.gilead.com/news-and-press/press-room/press-releases/2018/5/us-food-and-drug-administration-approves-expanded-indication-for-truvada-emtricitabine-and-tenofovir-disoproxil-fumarate-for-reducing-the-risk-of. Accessed 26 Feb 2024.
Hosek SG, Landovitz RJ, Kapogiannis B, et al. Safety and feasibility of antiretroviral preexposure prophylaxis for adolescent men who have sex with men aged 15 to 17 years in the United States. JAMA Pediatr. 2017;171(11):1063–71. https://doi.org/10.1001/jamapediatrics.2017.2007.
Tanner MR, Miele P, Carter W, et al. (2020) Preexposure prophylaxis for prevention of HIV acquisition among adolescents: clinical considerations. MMWR Recomm Rep. 2020;69(3):1–12. Published 2020 Apr 24. https://doi.org/10.15585/mmwr.rr6903a1.
Centers for Disease Control and Prevention. HIV infection risk, prevention, and testing behaviors among men who have sex with men—national HIV behavioral surveillance, 13 U.S. Cities, 2021. HIV Surveillance Special Report 31. 2023. https://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Access 26 Feb 2024.
Kanny D, Jeffries WL 4th, Chapin-Bardales J, et al. (2019) Racial/ethnic disparities in HIV preexposure prophylaxis among men who have sex with men - 23 urban areas. MMWR Morb Mortal Wkly Rep. 2017;68(37):801–6. Published 2019 Sep 20.https://doi.org/10.15585/mmwr.
Hoots BE, Finlayson T, Nerlander L, Paz-Bailey G, National HIV Behavioral Surveillance Study Group. Willingness to take, use of, and indications for pre-exposure prophylaxis among men who have sex with men-20 US cities, 2014. Clin Infect Dis. 2016;63(5):672–677. https://doi.org/10.1093/cid/ciw367
Garnett M, Hirsch-Moverman Y, Franks J, Hayes-Larson E, El-Sadr WM, Mannheimer S. Limited awareness of pre-exposure prophylaxis among Black men who have sex with men and transgender women in New York city. AIDS Care. 2018;30(1):9–17. https://doi.org/10.1080/09540121.2017.1363364.
Arrington-Sanders R, Morgan A, Oidtman J, Qian I, Celentano D, Beyrer C. A medical care missed opportunity: preexposure prophylaxis and young Black men who have sex with men. J Adolesc Health. 2016;59(6):725–8. https://doi.org/10.1016/j.jadohealth.2016.08.006.
Fallon SA, Park JN, Ogbue CP, Flynn C, German D. Awareness and acceptability of pre-exposure HIV prophylaxis among men who have sex with men in Baltimore. AIDS Behav. 2017;21(5):1268–77. https://doi.org/10.1007/s10461-016-1619-z.
Mehta SA, Silvera R, Bernstein K, Holzman RS, Aberg JA, Daskalakis DC. Awareness of post-exposure HIV prophylaxis in high-risk men who have sex with men in New York city. Sex Transm Infect. 2011;87(4):344–8. https://doi.org/10.1136/sti.2010.046284.
Kellerman SE, Hutchinson AB, Begley EB, Boyett BC, Clark HA, Sullivan P. Knowledge and use of HIV pre-exposure prophylaxis among attendees of minority gay pride events, 2004. J Acquir Immune Defic Syndr. 2006;43(3):376–7. https://doi.org/10.1097/01.qai.0000234085.18914.d5.
Mustanski B, Johnson AK, Garofalo R, Ryan D, Birkett M. Perceived likelihood of using HIV pre-exposure prophylaxis medications among young men who have sex with men. AIDS Behav. 2013;17(6):2173–9. https://doi.org/10.1007/s10461-012-0359-y.
Rolle CP, Rosenberg ES, Luisi N, et al. Willingness to use pre-exposure prophylaxis among Black and White men who have sex with men in Atlanta. Georgia Int J STD AIDS. 2017;28(9):849–57. https://doi.org/10.1177/0956462416675095.
Crosby RA, Geter A, DiClemente RJ, Salazar LF. Acceptability of condoms, circumcision and PrEP among young Black men who have sex with men: a descriptive study based on effectiveness and cost. Vaccines. 2014;2(1):129–37. https://doi.org/10.3390/vaccines2010129.
Eaton LA, Kalichman SC, Price D, Finneran S, Allen A, Maksut J. Stigma and conspiracy beliefs related to pre-exposure prophylaxis (PrEP) and interest in using PrEP among Black and White men and transgender women who have sex with men. AIDS Behav. 2017;21(5):1236–46. https://doi.org/10.1007/s10461-017-1690-0.
Philbin MM, Parker CM, Parker RG, Wilson PA, Garcia J, Hirsch JS. The promise of pre-exposure prophylaxis for Black men who have sex with men: an ecological approach to attitudes, beliefs, and barriers. AIDS Patient Care STDS. 2016;30(6):282–90. https://doi.org/10.1089/apc.2016.0037.
Cahill S, Taylor SW, Elsesser SA, Mena L, Hickson D, Mayer KH. Stigma, medical mistrust, and perceived racism may affect PrEP awareness and uptake in Black compared to White gay and bisexual men in Jackson, Mississippi and Boston, Massachusetts. AIDS Care. 2017;29(11):1351–8. https://doi.org/10.1080/09540121.2017.1300633.
Thomann M, Grosso A, Zapata R, Chiasson MA. ‘WTF is PrEP?’: attitudes towards pre-exposure prophylaxis among men who have sex with men and transgender women in New York City. Cult Health Sex. 2018;20(7):772–86. https://doi.org/10.1080/13691058.2017.1380230.
Brooks RA, Allen VC Jr, Regan R, Mutchler MG, Cervantes-Tadeo R, Lee SJ. HIV/AIDS conspiracy beliefs and intention to adopt preexposure prophylaxis among Black men who have sex with men in Los Angeles. Int J STD AIDS. 2018;29(4):375–81. https://doi.org/10.1177/0956462417727691.
Fields EL, Thornton N, Long A, et al. Young Black MSM’s exposures to and discussions about PrEP while navigating geosocial networking apps. J LGBT Youth. 2021;18(1):23–39. https://doi.org/10.1080/19361653.2019.1700205.
Lelutiu-Weinberger C, Golub SA. Enhancing PrEP access for Black and Latino men who have sex with men. J Acquir Immune Defic Syndr. 2016;73(5):547–55. https://doi.org/10.1097/QAI.0000000000001140.
Mutchler MG, McDavitt B, Ghani MA, Nogg K, Winder TJ, Soto JK. Getting PrEPared for HIV prevention navigation: young Black gay men talk about HIV prevention in the biomedical era. AIDS Patient Care STDS. 2015;29(9):490–502. https://doi.org/10.1089/apc.2015.0002.
Behler RL, Cornwell BT, Schneider JA. Patterns of social affiliations and healthcare engagement among young, Black, men who have sex with men. AIDS Behav. 2018;22(3):806–18. https://doi.org/10.1007/s10461-016-1668-3.
Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among Black and White men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007;21(15):2083–91. https://doi.org/10.1097/QAD.0b013e3282e9a64b.
Oster AM, Wiegand RE, Sionean C, et al. Understanding disparities in HIV infection between Black and White MSM in the United States. AIDS. 2011;25(8):1103–12. https://doi.org/10.1097/QAD.0b013e3283471efa.
Sullivan PS, Rosenberg ES, Sanchez TH, et al. Explaining racial disparities in HIV incidence in Black and White men who have sex with men in Atlanta, GA: a prospective observational cohort study. Ann Epidemiol. 2015;25(6):445–54. https://doi.org/10.1016/j.annepidem.2015.03.006.
Centers for Disease Control and Prevention. HIV infection risk, prevention, and testing behaviors among men who have sex with men—national HIV behavioral surveillance, 23 U.S. Cities, 2017. HIV Surveillance Special Report 22. 2019. https://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Accessed 22 Feb 2024.
Centers for Disease Control and Prevention (CDC). Prevalence and awareness of HIV infection among men who have sex with men –- 21 cities, United States, 2008. MMWR Morb Mortal Wkly Rep. 2010;59(37):1201–7.
MacKellar DA, Gallagher KM, Finlayson T, Sanchez T, Lansky A, Sullivan PS. Surveillance of HIV risk and prevention behaviors of men who have sex with men--a national application of venue-based, time-space sampling. Public Health Rep. 2007;122 Suppl 1(Suppl 1):39–47. https://doi.org/10.1177/00333549071220S107
Ezennia O, Geter A, Smith DK. The PrEP care continuum and Black men who have sex with men: a scoping review of published data on awareness, uptake, adherence, and retention in PrEP care. AIDS Behav. 2019;23:2654–73. https://doi.org/10.1007/s10461-019-02641-2.
Fields EL, Long A, Silvestri F, Bademosi K, Benton Denny J, Granderson R, Schumacher CM, Chandran A, Greenbaum A, Jennings JM. #projectpresence: highlighting Black LGBTQ persons and communities to reduce stigma: a program evaluation. Eval Program Plann. 2022;1(90):101978. https://doi.org/10.1016/j.evalprogplan.2021.101978.
Long A, Jennings JM, Bademosi K, Granderson R, Chandran A, Sawyer S, Schumacher CM, Greenbaum A, Fields E. Storytelling to improve healthcare worker understanding, beliefs, and practices related to LGBTQ+ patients: a program evaluation. Eval Program Plann. 2022;1(90):101979. https://doi.org/10.1016/j.evalprogplan.2021.101979.
Fields EL, Long A, Bademosi K, Granderson R, Schumacher CM, Chandran A, Kingon Y, Jennings JM. Identifying community-informed language to promote HIV pre-exposure prophylaxis (PrEP) in Black LGBTQ communities in Baltimore. AIDS Educ Prev. 2020;32(2):152–68. https://doi.org/10.1521/aeap.2020.32.2.152.
Quinn KG, Christenson E, Spector A, et al. The influence of peers on PrEP perceptions and use among young Black gay, bisexual, and other men who have sex with men: a qualitative examination. Arch Sex Behav. 2020;49:2129–43. https://doi.org/10.1007/s10508-019-01593-x.
Maksut JL, Eaton LA, Siembida EJ, Fabius CD, Bradley AM. Health care discrimination, sex behavior disclosure, and awareness of pre-exposure prophylaxis among Black men who have sex with men. Stigma Health. 2018;3(4):330–7. https://doi.org/10.1037/sah0000102.
Russ S, Zhang C, Liu Y. Pre-exposure prophylaxis care continuum, barriers, and facilitators among Black men who have sex with men in the United States: a systematic review and meta-analysis. AIDS Behav. 2021;25:2278–88. https://doi.org/10.1007/s10461-020-03156-x.
Golub SA. PrEP stigma: implicit and explicit drivers of disparity. Curr HIV/AIDS Rep. 2018;15(2):190–7. https://doi.org/10.1007/s11904-018-0385-0.
Baltimore City Health Department. #PeopleWhoLookLikeMe. https://health.baltimorecity.gov/hivstd-services/peoplewholooklikeme. Accessed 29 Jan 2024.
Schumacher Christina, Tao Xueting, Chandran Aruna, et al. Reaching those most at risk for HIV acquisition: evaluating racial/ethnic disparities in the preexposure prophylaxis care continuum in Baltimore city, Maryland. J Acquir Immune Defic Syndr. 2021;87(5):1145–53. https://doi.org/10.1097/QAI.0000000000002712.
Mayer KH, Nelson L, Hightow-Weidman L, et al. The persistent and evolving HIV epidemic in American men who have sex with men. Lancet. 2021;397(10279):1116–26. https://doi.org/10.1016/S0140-6736(21)00321-4.
Fields EL, Thornton N, Huettner S, et al. Safe Spaces 4 Sexual Health: a status-neutral, mobile van, HIV/STI testing intervention using online outreach to reach MSM at high risk for HIV acquisition or transmission. J Acquir Immune Defic Syndr. 2022;90(S1):S84–9. https://doi.org/10.1097/QAI.0000000000002968.
Fields EL, Long A, Dangerfield DT, et al. There’s an app for that: using geosocial networking apps to access young Black gay, bisexual, and other MSM at risk for HIV. Am J Health Promot. 2020;34(1):42–51. https://doi.org/10.1177/0890117119865112.
Newcomb ME, Mongrella MC, Weis B, McMillen SJ, Mustanski B. Partner disclosure of PrEP use and undetectable viral load on geosocial networking apps: frequency of disclosure and decisions about condomless sex. J Acquir Immune Defic Syndr. 2016;71(2):200–6. https://doi.org/10.1097/QAI.0000000000000819.
Patel RR, Harrison LC, Patel VV, et al. HIV pre-exposure prophylaxis programs incorporating social applications can reach at-risk men who have sex with men for successful linkage to care in Missouri, USA. J Assoc Nurses AIDS Care. 2017;28(3):428–30. https://doi.org/10.1016/j.jana.2017.01.003.
Funding
This work was supported, in part, by the Centers for Disease Control and Prevention of the US Department of Health and Human Services (HHS) award U01PS005115.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by Nicole Thornton, Kimberly Evans, and Errol Fields. The first draft of the manuscript was written by Hope King, and all authors, Yomi Tadfor, Danielle German, Colin Flynn, and Jacky Jennings, commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The SS4SH and BESURE studies were reviewed and approved by the Institutional Review Board at the Johns Hopkins School of Medicine and the Johns Hopkins School of Public Health and the Maryland Department of Health, respectively.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Not required.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflict of Interest
Dr. Errol Fields has served on an advisory board for Gilead Sciences and Roche Diagnostics. All other authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
King, H., Thornton, N., Evans, K.N. et al. Factors Associated with the Awareness of and Willingness to Use HIV Pre-exposure Prophylaxis Among Gay, Bisexual, and Other Men Who Have Sex with Men, Baltimore, MD, 2017–2019. J. Racial and Ethnic Health Disparities (2024). https://doi.org/10.1007/s40615-024-01954-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40615-024-01954-w