Abstract
Limited research has examined racial differences in the quality of staff-resident care interactions in long-term care settings. The quality of care interactions can significantly affect resident quality of life and psychological well-being among nursing home residents living with dementia. Limited research has assessed racial or facility differences in the quality of care interactions. The purpose of the present study was to determine if there were differences in the quality of care interactions among nursing home residents with dementia between Maryland nursing home facilities with and without Black residents. It was hypothesized that after controlling for age, cognition, comorbidities, and function, the quality of care interactions would be better in facilities with Black residents versus those in which there were only White residents. Baseline data from the Evidence Integration Triangle for Behavioral and Psychological Symptoms of Dementia (EIT-4-BPSD) intervention study was used and included 276 residents. The results indicated that facilities in Maryland with Black residents had a 0.27 increase (b = 0.27, p < .05) in the quality of care interaction score compared to facilities without Black residents. The findings from this study will be used to inform future interventions to aid in reducing quality of care disparities in nursing home facilities with and without Black nursing home residents. Future work should continue to examine staff, resident, and facility characteristics associated with the quality of care interactions to improve quality of life among all nursing home residents regardless of race or ethnicity.
Similar content being viewed by others
References
Harris-Kojetin L, Sengupta M, Lendon J, Rome V, Valverde R, Caffrey C. Long-term care providers and services users in the United States, 2015–2016. Vital Health Stat. National Center for Health Statistics; 2019. https://www.cdc.gov/nchs/data/series/sr_03/sr03_43-508.pdf
National Institute on Aging. Residential facilities, assisted living, and nursing homes. 2017. https://www.nia.nih.gov/health/residential-facilities-assisted-living-and-nursing-homes. Accessed 25 Jan 2023.
Feng Z, Fennell ML, Tyler DA, Clark M, Mor V. Growth of racial and ethnic minorities in US nursing homes driven by demographics and possible disparities in options. Health Aff. 2011;30:1358–65.
Travers JL, Dick AW, Wu B, Grabowski DC, Robison J, Agarwal M, et al. A profile of Black and Latino older adults receiving care in nursing homes. J Am Med Dir Assoc. 2022;23:1833–7. https://doi.org/10.1016/j.jamda.2022.04.010.
Fashaw SA, Thomas KS, McCreedy E, Mor V. Thirty-year trends in nursing home composition and quality since the passage of the Omnibus Reconciliation Act. J Am Med Dir Assoc. 2020;21:233–9.
Sengupta M, Lendon JP, Caffrey C, Melekin A, Singh P. Post-acute and long-term care providers and services users in the United States, 2017-2018. National Center for Health Statistics; 2022. https://doi.org/10.15620/cdc:115346.
Dean R, Proudfoot R, Lindesay J. The quality of interactions schedule (QUIS): Development, reliability and use in the evaluation of two domus units. Int J Geriatr Psychiatry. 1993;8:819–26.
Machiels M, Metzelthin SF, Hamers JPH, Zwakhalen SMG. Interventions to improve communication between people with dementia and nursing staff during daily nursing care: a systematic review. Int J Nurs Stud. 2017;66:37–46. https://doi.org/10.1016/j.ijnurstu.2016.11.0170020-7489/.
Clark P, Bowling A. Observational study of quality of life in nHS nursing homes and a long-stay ward for the elderly. Ageing Soc. 1989;9:123–48.
Alzheimer’s Association. 2021 Alzheimer’s disease facts and figures. In: Alzheimer’s and Dementia. Alzheimer’s Association; 2021.
Centers for Medicare & Medicaid Services. Nursing home data compendium 2015. Centers for Medicare & Medicaid Services; 2016. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/Downloads/nursinghomedatacompendium_508-2015.pdf
Rivera-Hernandez M, Kumar A, Epstein-Lubow G, Thomas KS. Disparities in nursing home use and quality among African American, Hispanic, and White Medicare residents with Alzheimer’s disease and related dementias. J Aging Health. 2019;31:1259–77. https://doi.org/10.1177/0898264318767778.
Fabius CD, Thomas KS. Examining Black-White disparities among medicare beneficiaries in assisted living settings in 2014. J Am Med Dir Assoc. 2019;20:703–9. https://doi.org/10.1016/j.jamda.2018.09.032.
Haugan G. The relationship between nurse-patient interaction and meaning-in-life in cognitively intact nursing home patients. J Adv Nurs. 2014;70:107–20. https://doi.org/10.1111/jan.12173.
Haugan G. Nurse-patient interaction is a resource for hope, meaning in life and self-transcendence in nursing home patients. Scand J Caring Sci. 2014;28:74–88.
Haugan G, Innstrand ST, Moksnes UK. The effect of nurse-patient interaction on anxiety and depression in cognitively intact nursing home patients. J Clin Nurs. 2013;22:2192–205. https://doi.org/10.1111/jocn.12072.
Jao YL, Loken E, MacAndrew M, van Haitsma K, Kolanowski A. Association between social interaction and affect in nursing home residents with dementia. Aging Ment Health. 2018;22:778–83. https://doi.org/10.1080/13607863.2017.1304526.
Sprangers S, Dijkstra K, Romijn-Luijten A. Communication skills training in a nursing home: effects of a brief intervention on residents and nursing aides. Clin Interv Aging. 2015;10:311–9.
Williams K, Perkhounkova Y, Herman R, Bossen A. A communication intervention to reduce resistiveness in dementia care: a cluster randomized controlled trial. Gerontologist. 2017;57:707–18. https://academic.oup.com/gerontologist/article-abstract/57/4/707/2631994
Bridges J, Griffiths P, Oliver E, Pickering RM. Hospital nurse staffing and staff-patient interactions: an observational study. BMJ Qual Saf. 2019;28:706–13. http://qualitysafety.bmj.com/
Adlbrecht L, Bartholomeyczik S, Hildebrandt C, Mayer H. Social interactions of persons with dementia living in special care units in long-term care: a mixed-methods systematic review. Dementia. 2021;20:967–84.
Fauth EB, Meyer KV, Rose C. Co-occurrence of positive staff interactions and positive affect in memory-care residents: an observational study. Int J Geriatr Psychiatry. 2020;35:759–68. https://onlinelibrary.wiley.com/doi/abs/10.1002/gps.5299
van Manen AS, Aarts S, Metzelthin SF, Verbeek H, Hamers JPH, Zwakhalen SMG. A communication model for nursing staff working in dementia care: results of a scoping review. Int J Nurs Stud. 2021;113:1–15. https://doi.org/10.1016/j.ijnurstu.2020.103776.
Kovach CR, Noonan PE, Schlidt AM, Wells T. A model of consequences of need-driven, dementia-compromised behavior. J Nurs Scholarsh. 2005;37:140.
Backhouse T, Dudzinski E, Killett A, Mioshi E. Strategies and interventions to reduce or manage refusals in personal care in dementia: a systematic review. Int J Nurs Stud. 2020;109:103640.
Spigelmyer PC, Hupcey J, Kitko L. A concept analysis of resistiveness to care. Clin Nurs Res. 2021;30:50–8.
Morgan DG, Cammer A, Stewart NJ, Crossley M, D’Arcy C, Forbes DA, et al. Nursing aide reports of combative behavior by residents with dementia: results from a detailed prospective incident diary. J Am Med Dir Assoc. 2012;13:220–7.
Ball MM, Lepore ML, Perkins MM, Hollingsworth C, Sweatman M. They are the reason I come to work: the meaning of resident-staff relationships in assisted living. J Aging Stud. 2009;23:37–47. https://doi.org/10.1016/j.jaging.2007.09.006.
Dodson L, Zincavage RM. “It’s like a family”: caring labor, exploitation, and race in nursing homes. Gend Soc. 2007;21:905–28.
Lachs MS, Rosen T, Teresi JA, Eimicke JP, Ramirez M, Silver S, et al. Verbal and physical aggression directed at nursing home staff by residents. J Gen Intern Med. 2013;28:660–7.
PHI. Workforce Data Center. 2023 https://phinational.org/policy-research/workforce-data-center/.
Gallois C, Ogay T, Giles H. Communication accommodation theory: a look back and a look ahead. In: Gudykunst WB, editor. Theorizing about intercultural communication. Thousand Oaks: Sage; 2005. p. 121–48.
Giles H. Language and Social Psychology. Oxford, UK: Blackwell Publishing; 1979.
Barker V, Giles H, Harwood J. Inter- and intragroup perspectives on intergenerational communication. In: Nussbaum JF, Coupland J, editors. Handbook of communication and aging research. 2nd ed. Mahwah, New Jersey: Lawrence Erlbaum Associates; 2004. p. 159–86. https://www.taylorfrancis.com/books/9781135639822/chapters/10.4324/9781410610171-14.
Maryland Health Care Commission. Nursing home resident profile: Maryland. 2020. https://mhcc.maryland.gov/mhcc/pages/hcfs/hcfs_ltc/documents/Routine_Reports_All_Tables_6_30_2021.pdf. Accessed 27 Jan 2023.
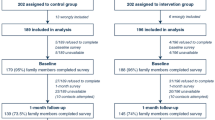
Resnick B, Kolanowski A, van Haitsma K, Galik E, Boltz M, Ellis J, et al. Testing the evidence integration triangle for implementation of interventions to manage behavioral and psychological symptoms associated with dementia: protocol for a pragmatic trial. Res Nurs Health. 2018;41:228–42. https://doi.org/10.1002/nur.21866.
Chodosh J, Edelen MO, Buchanan JL, Yosef JA, Ouslander JG, Berlowitz DR, et al. Nursing home assessment of cognitive impairment: development and testing of a brief instrument of mental status. J Am Geriatr Soc. 2008;56:2069–75. https://doi.org/10.1111/j.1532-5415.2008.01944.x.
Mansbach WE, Mace RA, Clark KM. Differentiating levels of cognitive functioning: a comparison of the Brief Interview for Mental Status (BIMS) and the Brief Cognitive Assessment Tool (BCAT) in a nursing home sample. Aging Ment Health. 2014;18:921–8. https://doi.org/10.1080/13607863.2014.899971.
Mahoney F, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61–5. https://pubmed.ncbi.nlm.nih.gov/14258950/
Bouwstra H, Smit EB, Wattel EM, van der Wouden JC, Hertogh CMPM, Terluin B, et al. Measurement properties of the Barthel index in geriatric rehabilitation. J Am Med Dir Assoc. 2019;20:420–425.e1.
Hsueh IP, Lee MM, Hsieh CL. Psychometric characteristics of the barthel activities of daily living index in stroke patients. J Formos Med Assoc. 2001;100:526–58.
Linn BS, Linn MW, Gurel L. Cumulative illness rating scale. J Am Geriatr Soc. 1968;16:622–6.
Parmelee PA, Thuras PD, Katz IR, Lawton MP. Validation of the cumulative illness rating scale in a geriatric residential population. J Am Geriatr Soc. 1995;43:130–7.
Resnick B, Galik E, Paudel A, McPherson R, van Haitsma K, Boltz M, et al. Reliability and validity testing of the quantified quality of interaction scale (QuIS). J Nurs Meas. 2021;29 https://doi.org/10.1891/JNM-D-19-00101.
Jenkins H, Allen C. Relationship between staff burnout/distress and interactions with residents in two residential homes for older people. Int J Geriatr Psychiatry. 1998;13:466–72. https://onlinelibrary.wiley.com/doi/full/10.1002/%28SICI%291099-1166%28199807%2913%3A7%3C466%3A%3AAID-GPS799%3E3.0.CO%3B2-V
McLean C, Griffiths P, Mesa-Eguiagaray I, Pickering RM, Bridges J. Reliability, feasibility, and validity of the quality of interactions schedule (QuIS) in acute hospital care: an observational study. BMC Health Serv Res. 2017;17:380.
Hefele JG, Ritter GA, Bishop CE, Acevedo A, Ramos C, Nsiah-Jefferson LA, et al. Examining racial and ethnic differences in nursing home quality. Jt Comm J Qual Patient Saf. 2017;43:554–64. https://doi.org/10.1016/j.jcjq.2017.06.003.
Ryvicker M. Staff-resident interaction in the nursing home: an ethnographic study of socio-economic disparities and community contexts. J Aging Stud. 2011;25:295–304.
McPherson R, Resnick B, Galik E, Gruber-baldini AL, Holmes S, Kusmaul N. The association between engagement in activities of daily living and care interactions for residents living with dementia. J Nurs Care Qual. 2022;38(2):E18–24.
Achterberg W, Lautenbacher S, Husebo B, Erdal A, Herr K. Pain in dementia. Pain Rep. 2020;5:1–8. https://doi.org/10.1097/PR9.0000000000000803.
Van Beek APA, Frijters DHM, Wagner C, Groenewegen PP, Ribbe MW. Social engagement and depressive symptoms of elderly residents with dementia: a cross-sectional study of 37 long-term care units. Int Psychogeriatr. 2011;23:625–33.
Williams K, Herman RE. Linking resident behavior to dementia care communication: effects of emotional tone. Behav Ther. 2011;42:42–6. https://doi.org/10.1016/j.beth.2010.03.003.
Harrad R, Sulla F. Factors associated with and impact of burnout in nursing and residential home care workers for the elderly. Acta Biomedica. 2018;89:60–9.
Paudel A, Galik E, Resnick B, Doran K, Boltz M, Zhu S. Factors associated with the quality of staff-resident interactions in assisted living. J Nurs Care Qual. 2021;37(2):168–75.
Centers for Medicare & Medicaid Services. Five-star quality rating system 2021 https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/FSQRS
Paul D, Godby T, Saldanha S, Valle J, Coustasse A. Quality of care and profitability in not-for-profit versus for-profit nursing homes. In: Sanchez J, editor. Proceedings of the business and health administration association annual conference. Chicago, IL; 2016. p. 90–97.
Gould LJ, Griffiths P, Barker HR, Libberton P, Mesa-Eguiagaray I, Pickering RM, et al. Compassionate care intervention for hospital nursing teams caring for older people: A pilot cluster randomised controlled trial. BMJ Open. 2018;8:18563. https://bmjopen.bmj.com/content/8/2/e018563
Williams K. Improving outcomes of nursing home interactions. Res Nurs Health. 2006;29:121–33. https://doi.org/10.1002/nur.20117.
Ballard C, Corbett A, Orrell M, Williams G, Moniz-Cook E, Romeo R, et al. Impact of person-centred care training and person-centred activities on quality of life, agitation, and antipsychotic use in people with dementia living in nursing homes: A cluster-randomised controlled trial. PLoS Med. 2018;15(2):e1002500. https://doi.org/10.1371/journal.pmed.1002500.
Kim H, Woods DL, Mentes JC, Martin JL, Moon A, Phillips LR. The nursing assistants’ communication style and the behavioral symptoms of dementia in Korean-American nursing home residents. Geriatr Nurs. 2014;35:S11–6. https://doi.org/10.1016/j.gerinurse.2014.02.016.
Williams K, Coleman CK, Perkhounkova Y, Beachy T, Hein M, Shaw CA, et al. Moving online: a pilot clinical trial of the changing talk online communication education for nursing home staff. Gerontologist. 2021;61(8):1338–45. https://academic.oup.com/gerontologist/advance-article/doi/10.1093/geront/gnaa210/6042577
Xiao LD, Willis E, Harrington A, Gillham D, de Bellis A, Morey W, et al. Improving socially constructed cross-cultural communication in aged care homes: a critical perspective. Nurs Inq. 2018;25:e12208. https://doi.org/10.1111/nin.12208.
Paudel A, Galik E, Resnick B, Doran K, Boltz M, Zhu S. Pilot testing of the promoting positive care interactions intervention in assisted living. J Gerontol Nurs. 2022;48:17–25. https://journals.healio.com/doi/10.3928/00989134-20220629-04
Availability of Data and Material
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Code Availability
Not applicable
Funding
The parent study was funded by the National Institutes of Health (NIH) (1R01NR015982-01A1).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Dr. Rachel McPherson and Dr. Barbara Resnick. The first draft of the manuscript was written by Dr. Rachel McPherson, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The parent study was approved by the University of Maryland Baltimore Institutional Review Board, and the study was performed in accordance with the ethical standards in the 1964 Declaration of Helsinki.
Consent to Participate
Informed consent was obtained by all participants or by their legally authorized representatives when applicable.
Consent for Publication
Not applicable
Conflicts of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
McPherson, R., Resnick, B. & Wallace, B.H. Differences in Staff-Resident Care Interactions by Nursing Home Racial Composition: a Preliminary Analysis. J. Racial and Ethnic Health Disparities (2023). https://doi.org/10.1007/s40615-023-01673-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40615-023-01673-8