Abstract
Introduction
Perioperative pain may have deleterious effects for all patients. We aim to examine disparities in pain management for children in the perioperative period to understand whether any racial and ethnic groups are at increased risk of poor pain control.
Methods
Medical records from children ≤ 18 years of age who underwent surgery from May 2014 to May 2018 were reviewed. The primary outcome was total intraoperative morphine equivalents. The secondary outcomes were intraoperative non-opioid analgesic administration and first conscious pain score. The exposure was race and ethnicity. The associations of race and ethnicity with outcomes of interest were modeled using linear or logistic regression, adjusted for preselected confounders and covariates. Bonferroni corrections were made for multiple comparisons.
Results
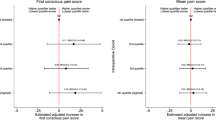
A total of 21,229 anesthetics were included in analyses. In the adjusted analysis, no racial and ethnic group received significantly more or less opioids intraoperatively than non-Hispanic (NH) whites. Asians, Hispanics, and Pacific Islanders were estimated to have significantly lower odds of receiving non-opioid analgesics than NH whites: odds ratio (OR) = 0.83 (95% confidence interval (CI): 0.70, 0.97); OR = 0.84 (95% CI: 0.74, 0.97), and OR = 0.53 (95% CI: 0.33, 0.84) respectively. Asians were estimated to have significantly lower odds of reporting moderate-to-severe pain on awakening than NH whites: OR = 0.80 (95% CI: 0.66, 0.99).
Conclusions
Although children of all races and ethnicities investigated received similar total intraoperative opioid doses, some were less likely to receive non-opioid analgesics intraoperatively. Asians were less likely to report moderate-severe pain upon awakening. Further investigation may delineate how these differences lead to disparate patient outcomes and are influenced by patient, provider, and system factors.


Similar content being viewed by others
Abbreviations
- LPCH:
-
Lucile Packard Children’s Hospital Stanford
- EMR:
-
Electronic medical record
- OR:
-
Operating room
- ASA:
-
American Society of Anesthesiologists physical status classification
- FLACC:
-
Face, Legs, Activity, Cry, Consolability pain scale
- PACU:
-
Post-anesthesia care unit
- OSA:
-
Obstructive sleep apnea
- ICD:
-
International Classification of Diseases
- LTR:
-
Likelihood ratio test
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- SD:
-
Standard deviation
- NH whites:
-
Non-Hispanic whites
References
Berdahl TA, Friedman BS, McCormick MC, Simpson L. Annual report on health care for children and youth in the United States: trends in racial/ethnic, income, and insurance disparities over time, 2002-2009. Acad Pediatr. 2013;13(3):191–203.
Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O II. Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003;118(4):293–302.
Flores G, R. Committee On Pediatric. Technical report--racial and ethnic disparities in the health and health care of children. Pediatrics. 2010;125(4):e979–e1020.
Lange EMS, Rao S, Toledo P. Racial and ethnic disparities in obstetric anesthesia. Semin Perinatol. 2017;41(5):293–8.
Peterson K, Anderson J, Boundy E, Ferguson L, McCleery E, Waldrip K. Mortality disparities in racial/ethnic minority groups in the Veterans Health Administration: an evidence review and map. Am J Public Health. 2018;108(3):e1–e11.
van Gulik L, Ahlers SJGM, van de Garde EMW, Bruins P, van Boven WJ, Tibboel D, et al. Remifentanil during cardiac surgery is associated with chronic thoracic pain 1 yr after sternotomy. Br J Anaesth. 2012;109(4):616–22.
Fletcher D, Martinez V. Opioid-induced hyperalgesia in patients after surgery: a systematic review and a meta-analysis. Br J Anaesth. 2014;112(6):991–1004.
Lee LA, Caplan RA, Stephens LS, Posner KL, Terman GW, Voepel-Lewis T, et al. Postoperative opioid-induced respiratory depression: a closed claims analysis. Anesthesiology. 2015;122(3):659–65.
Long DR, Lihn AL, Friedrich S, Scheffenbichler FT, Safavi KC, Burns SM, et al. Association between intraoperative opioid administration and 30-day readmission: a pre-specified analysis of registry data from a healthcare network in New England. Br J Anaesth. 2018;120(5):1090–102.
von Dincklage F, Jakuscheit A, Weth J, Lichtner G, Jurth C, Rehberg-Klug B. Higher doses of intraoperative analgesia are associated with lower levels of persistent pain and less analgesic consumption six months after total hip arthroplasty. Eur J Pain. 2018;22(4):691–9.
Joshi GP, Ogunnaike BO. Consequences of inadequate postoperative pain relief and chronic persistent postoperative pain. Anesthesiol Clin North Am. 2005;23(1):21–36.
Baratta JL, Schwenk ES, Viscusi ER. Clinical consequences of inadequate pain relief: barriers to optimal pain management. Plast Reconstr Surg. 2014;134(4 Suppl 2):15S–21S.
Pavlin DJ, Chen C, Penaloza DA, Buckley FP. A survey of pain and other symptoms that affect the recovery process after discharge from an ambulatory surgery unit. J Clin Anesth. 2004;16(3):200–6.
Fortier J, Chung F, Su J. Unanticipated admission after ambulatory surgery--a prospective study. Can J Anaesth. 1998;45(7):612–9.
Pavlin DJ, et al. Pain as a factor complicating recovery and discharge after ambulatory surgery. Anesth Analg. 2002;95(3):627–34 table of contents.
Pavlin DJ, et al. Factors affecting discharge time in adult outpatients. Anesth Analg. 1998;87(4):816–26.
Jimenez N, et al. Perioperative analgesic treatment in Latino and non-Latino pediatric patients. J Health Care Poor Underserved. 2010;21(1):229–36.
Nafiu OO, Chimbira WT, Stewart M, Gibbons K, Porter LK, Reynolds PI. Racial differences in the pain management of children recovering from anesthesia. Paediatr Anaesth. 2017;27(7):760–7.
Rosenbloom JM, Senthil K, Long AS, Robinson WR, Peeples KN, Fiadjoe JE, et al. A limited evaluation of the association of race and anesthetic medication administration: a single-center experience with appendectomies. Paediatr Anaesth. 2017;27(11):1142–7.
Jimenez N, Anderson GD, Shen DD, Nielsen SS, Farin FM, Seidel K, et al. Is ethnicity associated with morphine’s side effects in children? Morphine pharmacokinetics, analgesic response, and side effects in children having tonsillectomy. Paediatr Anaesth. 2012;22(7):669–75.
Committee, S.S., NQF-Endorsed measures for surgical procedures, 2015-2017, H.a.H. Services, Editor. 2017, National Quality Forum: 1030 15th St NW, Suite 800 Washington, DC 20005.
Hall, M.J., et al., Ambulatory surgery data from hospitals and ambulatory surgery centers: United States, 2010. Natl Health Stat Report, 2017(102): p. 1–15.
National Center for Health Statistics (U.S.), National hospital discharge survey: 2010 table, procedures by selected patient characteristics - number by procedure category and age, in DHHS publication. 2010, U.S. Dept. of Health and Human Services, Centers for Disease Control and Prevention: Hyattsville, Md. p. v.
Section on, A. and M. Pain. The pediatrician’s role in the evaluation and preparation of pediatric patients undergoing anesthesia. Pediatrics. 2014;134(3):634–41.
Jimenez N, Jackson DL, Zhou C, Ayala NC, Ebel BE. Postoperative pain management in children, parental English proficiency, and access to interpretation. Hosp Pediatr. 2014;4(1):23–30.
Berry JG, et al. Pediatrics. 2019:143(4).
Kain ZN, Mayes LC, Caldwell-Andrews AA, Karas DE, McClain BC. Preoperative anxiety, postoperative pain, and behavioral recovery in young children undergoing surgery. Pediatrics. 2006;118(2):651–8.
Rony RY, et al. Parental postoperative pain management: attitudes, assessment, and management. Pediatrics. 2010;125(6):e1372–8.
Rosenberg RE, Clark RA, Chibbaro P, Hambrick HR, Bruzzese JM, Feudtner C, et al. Factors predicting parent anxiety around infant and toddler postoperative and pain. Hosp Pediatr. 2017;7(6):313–9.
Schwenk ES, Mariano ER. Designing the ideal perioperative pain management plan starts with multimodal analgesia. Korean J Anesthesiol. 2018;71(5):345–52.
Butwick AJ, Blumenfeld YJ, Brookfield KF, Nelson LM, Weiniger CF. Racial and ethnic disparities in mode of anesthesia for cesarean delivery. Anesth Analg. 2016;122(2):472–9.
Glance LG, Wissler R, Glantz C, Osler TM, Mukamel DB, Dick AW. Racial differences in the use of epidural analgesia for labor. Anesthesiology. 2007;106(1):19–25 discussion 6-8.
King MR, de Souza E, Rosenbloom JM, Wang E, Anderson TA. Association between race and ethnicity in the delivery of regional anesthesia for pediatric patients: a single-center study of 3189 regional anesthetics in 25,664 surgeries. Anesth Analg. 2020;131(1):255–62.
Memtsoudis SG, Besculides MC, Swamidoss CP. Do race, gender, and source of payment impact on anesthetic technique for inguinal hernia repair? J Clin Anesth. 2006;18(5):328–33.
Memtsoudis SG, Poeran J, Zubizarreta N, Rasul R, Opperer M, Mazumdar M. Anesthetic care for orthopedic patients: is there a potential for differences in care? Anesthesiology. 2016;124(3):608–23.
Disparities in health care quality among racial and ethnic minority groups: selected findings from the 2010 national healthcare quality and disparities reports, A.f.H.R.a. Quality, Editor. 2011: Rockville, MD p 4.
Pinheiro PS, Callahan KE, Boscoe FP, Balise RR, Cobb TR, Lee DJ, et al. Cancer site-specific disparities in New York, including the 1945-1965 birth cohort’s impact on liver cancer patterns. Cancer Epidemiol Biomark Prev. 2018;27(8):917–27.
Ahonen J, Olkkola KT, Hynynen M, Seppälä T, Ikävalko H, Remmerie B, et al. Comparison of alfentanil, fentanyl and sufentanil for total intravenous anaesthesia with propofol in patients undergoing coronary artery bypass surgery. Br J Anaesth. 2000;85(4):533–40.
Zhu A, Benzon HA, Anderson TA. Evidence for the efficacy of systemic opioid-sparing analgesics in pediatric surgical populations: a systematic review. Anesth Analg. 2017;125(5):1569–87.
Aldrete JA, Kroulik D. A postanesthetic recovery score. Anesth Analg. 1970;49(6):924–34.
Boonstra AM, et al. Cut-off points for mild, moderate, and severe pain on the numeric rating scale for pain in patients with chronic musculoskeletal pain: variability and influence of sex and catastrophizing. Front Psychol. 2016;7:1466.
Gerbershagen HJ, Rothaug J, Kalkman CJ, Meissner W. Determination of moderate-to-severe postoperative pain on the numeric rating scale: a cut-off point analysis applying four different methods. Br J Anaesth. 2011;107(4):619–26.
Hirschfeld G, Zernikow B. Variability of “optimal” cut points for mild, moderate, and severe pain: neglected problems when comparing groups. Pain. 2013;154(1):154–9.
Schoenfeld AJ, Nwosu K, Jiang W, Yau AL, Chaudhary MA, Scully RE, et al. Risk factors for prolonged opioid use following spine surgery, and the association with surgical intensity, among opioid-naive patients. J Bone Joint Surg Am. 2017;99(15):1247–52.
Cron DC, Englesbe MJ, Bolton CJ, Joseph MT, Carrier KL, Moser SE, et al. Preoperative opioid use is independently associated with increased costs and worse outcomes after major abdominal surgery. Ann Surg. 2017;265(4):695–701.
Flegal KM, Cole TJ. Construction of LMS parameters for the Centers for Disease Control and Prevention 2000 growth charts. Natl Health Stat Report. 2013(63):1–3.
Statistics, N.C.f.H CDC growth charts: percentile data files with LMS values. 2000 08/04/2009 [cited 2019 07/20/2019]; Available from: https://www.cdc.gov/growthcharts/percentile_data_files.htm.
Unequal treatment: confronting racial and ethnic disparities in health care, B.D. Smedley, A.Y. Stith, and A.R. Nelson, Editors. 2003: Washington (DC).
Kim EJ, Kim T, Paasche-Orlow MK, Rose AJ, Hanchate AD. Disparities in hypertension associated with limited English proficiency. J Gen Intern Med. 2017;32(6):632–9.
Pain, T.F.o.T.o.t.I.A.f.t.S.o., Classification of chronic pain: descriptions of chronic pain sydromes and definitions of pain terms. 2nd ed, ed. H. Merskey and N. Bogduk. 1994, Seattle, WA 98105: International Association for the Study of Pain. 238.
Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–60.
Liu W, Liu J, Tan X, Wang S. Ultrasound-guided lower forearm median nerve block in open surgery for trigger thumb in 1- to 3-year-old children: a randomized trial. Paediatr Anaesth. 2018;28(2):134–41.
Luo M, Liu X, Ning L, Sun Y, Cai Y, Shen S’. Comparison of ultrasonography-guided bilateral intercostal nerve blocks and conventional patient-controlled intravenous analgesia for pain control after the Nuss procedure in children: a prospective randomized study. Clin J Pain. 2017;33(7):604–10.
Friedrichsdorf SJ, Postier A, Eull D, Weidner C, Foster L, Gilbert M, et al. Pain outcomes in a US Children’s hospital: a prospective cross-sectional survey. Hosp Pediatr. 2015;5(1):18–26.
Harrison D, Joly C, Chretien C, Cochrane S, Ellis J, Lamontagne C, et al. Pain prevalence in a pediatric hospital: raising awareness during Pain Awareness Week. Pain Res Manag. 2014;19(1):e24–30.
Taylor EM, Boyer K, Campbell FA. Pain in hospitalized children: a prospective cross-sectional survey of pain prevalence, intensity, assessment and management in a Canadian pediatric teaching hospital. Pain Res Manag. 2008;13(1):25–32.
Walther-Larsen S, Pedersen MT, Friis SM, Aagaard GB, Rømsing J, Jeppesen EM, et al. Pain prevalence in hospitalized children: a prospective cross-sectional survey in four Danish university hospitals. Acta Anaesthesiol Scand. 2017;61(3):328–37.
Segerdahl M, et al. Children in day surgery: clinical practice and routines. The results from a nation-wide survey. Acta Anaesthesiol Scand. 2008;52(6):821–8.
Dixon S, et al. Behavioral effects of circumcision with and without anesthesia. J Dev Behav Pediatr. 1984;5(5):246–50.
Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res. 2017;10:2287–98.
Sinatra R. Causes and consequences of inadequate management of acute pain. Pain Med. 2010;11(12):1859–71.
Weisman SJ, Bernstein B, Schechter NL. Consequences of inadequate analgesia during painful procedures in children. Arch Pediatr Adolesc Med. 1998;152(2):147–9.
Michelet D, Andreu-Gallien J, Bensalah T, Hilly J, Wood C, Nivoche Y, et al. A meta-analysis of the use of nonsteroidal antiinflammatory drugs for pediatric postoperative pain. Anesth Analg. 2012;114(2):393–406.
Afman CE, Welge JA, Steward DL. Steroids for post-tonsillectomy pain reduction: meta-analysis of randomized controlled trials. Otolaryngol Head Neck Surg. 2006;134(2):181–6.
Cho HK, Kim KW, Jeong YM, Lee HS, Lee YJ, Hwang SH. Efficacy of ketamine in improving pain after tonsillectomy in children: meta-analysis. PLoS One. 2014;9(6):e101259.
Dahmani S, Michelet D, Abback PS, Wood C, Brasher C, Nivoche Y, et al. Ketamine for perioperative pain management in children: a meta-analysis of published studies. Paediatr Anaesth. 2011;21(6):636–52.
Lambert P, et al. Clonidine premedication for postoperative analgesia in children. Cochrane Database Syst Rev. 2014;1:CD009633.
Bellon M, le Bot A, Michelet D, Hilly J, Maesani M, Brasher C, et al. Efficacy of intraoperative dexmedetomidine compared with placebo for postoperative pain management: a meta-analysis of published studies. Pain Ther. 2016;5(1):63–80.
Schnabel A, Reichl SU, Poepping DM, Kranke P, Pogatzki-Zahn EM, Zahn PK. Efficacy and safety of intraoperative dexmedetomidine for acute postoperative pain in children: a meta-analysis of randomized controlled trials. Paediatr Anaesth. 2013;23(2):170–9.
Russell P, von Ungern-Sternberg BS, Schug SA. Perioperative analgesia in pediatric surgery. Curr Opin Anaesthesiol. 2013;26(4):420–7.
Singhal NR, Jones J, Semenova J, Williamson A, McCollum K, Tong D, et al. Multimodal anesthesia with the addition of methadone is superior to epidural analgesia: a retrospective comparison of intraoperative anesthetic techniques and pain management for 124 pediatric patients undergoing the Nuss procedure. J Pediatr Surg. 2016;51(4):612–6.
Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006;367(9522):1618–25.
Rove KO, Edney JC, Brockel MA. Enhanced recovery after surgery in children: promising, evidence-based multidisciplinary care. Paediatr Anaesth. 2018;28(6):482–92.
Shinnick JK, Short HL, Heiss KF, Santore MT, Blakely ML, Raval MV. Enhancing recovery in pediatric surgery: a review of the literature. J Surg Res. 2016;202(1):165–76.
Aviram J, Samuelly-Leichtag G. Efficacy of cannabis-based medicines for pain management: a systematic review and meta-analysis of randomized controlled trials. Pain Physician. 2017;20(6):E755–96.
Kim HJ, Yang GS, Greenspan JD, Downton KD, Griffith KA, Renn CL, et al. Racial and ethnic differences in experimental pain sensitivity: systematic review and meta-analysis. Pain. 2017;158(2):194–211.
Rahim-Williams B, Riley JL III, Williams AKK, Fillingim RB. A quantitative review of ethnic group differences in experimental pain response: do biology, psychology, and culture matter? Pain Med. 2012;13(4):522–40.
Lu Q, Zeltzer L, Tsao J. Multiethnic differences in responses to laboratory pain stimuli among children. Health Psychol. 2013;32(8):905–14.
Estimated population ages 0–17, by race/ethnicity (e.g., an estimated 419,938 multiracial children lived in California in 2018). C.D.o. Finance, Editor. 2018, U.S. Census Bureau.
Funding
Dr. Rosenbloom’s work was supported by the National Institutes of Health T32 GM007592 grant (Research Training for Anesthetists). All other support was provided from institutional and/or departmental sources.
Author information
Authors and Affiliations
Contributions
Christine G. Jette: This author helped with research conceptualization and design, data analysis, data interpretation, writing, and final approval of the manuscript.
Julia M. Rosenbloom: This author helped with research conceptualization and design, writing and final approval of the manuscript.
Ellen Wang: This author helped with research conceptualization and design, patient recruitment, data collection, data interpretation, writing, and final approval of the manuscript.
Elizabeth De Souza: This author helped with research conceptualization and design, data analysis, data interpretation, writing, and final approval of the manuscript.
T. Anthony Anderson: This author helped with research conceptualization and design, patient recruitment, data collection, data interpretation, writing, and final approval of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have potential conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jette, C.G., Rosenbloom, J.M., Wang, E. et al. Association Between Race and Ethnicity with Intraoperative Analgesic Administration and Initial Recovery Room Pain Scores in Pediatric Patients: a Single-Center Study of 21,229 Surgeries. J. Racial and Ethnic Health Disparities 8, 547–558 (2021). https://doi.org/10.1007/s40615-020-00811-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-020-00811-w