Abstract
Purpose of Review
In this narrative review, we summarize the peer-reviewed literature published between 2017 and 2022 that evaluated ambient environmental risk factors for primary headache disorders, which affect more than half of the population globally. Primary headache disorders include migraine, tension-type headache (TTH), and trigeminal and autonomic cephalalgias (TAC).
Recent findings
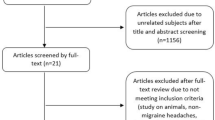
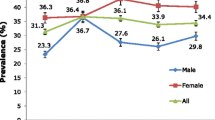
We identified 17 articles that met the inclusion criteria via PubMed or Google Scholar. Seven studies (41%) relied on data from US populations. The remaining studies were conducted in China, Taiwan, Germany, Ghana, Japan, the Netherlands, South Korea, and Turkey. Air pollution was the most frequently assessed environmental risk factor. Most studies were cross-sectional and focused on all-cause or migraine headaches; one study included TTH, and none included TAC. Short-term exposure to fine particulate matter (PM2.5) was not consistently associated with headache endpoints, but long-term exposure to PM2.5 was associated with migraine headache prevalence and severity across multiple studies. Elevated ambient temperature, changes in weather, oil and gas well exposure, and less natural greenspace, but not noise pollution, were also associated with headache. No studies considered water pollution, metal exposure, ultrafine particulate matter, or wildfire smoke exposure.
Summary
There is a need for ongoing research focused on headache and the environment. Study designs with the greatest explanatory power may include longitudinal studies that capture the episodic nature of headache and case-crossover analysis, which control for time-invariant individual-level confounders by design. There is also a clear need for research that considers comorbid psychiatric illness and socioeconomic position as powerful modifiers of the effect of the environment on headache.


Similar content being viewed by others
Data Availability
Not applicable.
References
Stovner LJ, Hagen K, Linde M, Steiner TJ. The global prevalence of headache: an update, with analysis of the influences of methodological factors on prevalence estimates. J Headache Pain. 2022;23(1):34.
Stovner LJ, Nichols E, Steiner TJ, et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17(11):954–76.
Stovner L, Hagen K, Jensen R, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27(3):193–210.
Burton WN, Conti DJ, Chen C-Y, Schultz AB, Edington DW. The economic burden of lost productivity due to migraine headache: a specific worksite analysis. J Occup Environ Med. 2002;44:523–9.
Malmberg-Ceder K, Vuorio T, Korhonen PE, Kautiainen H, Soinila S, Haanpää M. The impact of self-reported recurrent headache on absenteeism and Presenteeism at work among Finnish municipal female employees. J Pain Res. 2020;13:2135–42.
Michel P, Dartigues J, Duru G, Moreau J, Salamon R, Henry P. Incremental absenteeism due to headaches in migraine: results from the Mig-Access French national cohort. Cephalalgia. 1999;19(5):503–10.
Baigi K, Stewart WF. Headache and migraine: a leading cause of absenteeism. In: Handbook of clinical neurology. Elsevier. 2015;131:447–463.
Porter JK, Di Tanna GL, Lipton RB, Sapra S, Villa G. Costs of acute headache medication use and productivity losses among patients with migraine: insights from three randomized controlled trials. PharmacoEcon-open. 2019;3(3):411–7.
Finocchi C, Sivori G. Food as trigger and aggravating factor of migraine. Neurol Sci. 2012;33:77–80.
Chabriat H, Danchot J, Michel P, Joire J, Henry P. Precipitating factors of headache. A prospective study in a national control-matched survey in migraineurs and nonmigraineurs. Headache. 1999;39(5):335–8.
Spierings EL, Ranke AH, Honkoop PC. Precipitating and aggravating factors of migraine versus tension-type headache. Headache. 2001;41(6):554–8.
Wöber C, Holzhammer J, Zeitlhofer J, Wessely P, Wöber-Bingöl Ç. Trigger factors of migraine and tension-type headache: experience and knowledge of the patients. J Headache Pain. 2006;7(4):188–95.
Scharff L, Turk DC, Marcus DA. Triggers of headache episodes and coping responses of headache diagnostic groups. Headache. 1995;35(7):397–403.
Louis S, Carlson AK, Suresh A, et al. Impacts of climate change and air pollution on neurologic health, disease, and practice: a scoping review. Neurology. 2023;100(10):474–83.
Arnold M. Headache classification committee of the international headache society (IHS) the international classification of headache disorders. Cephalalgia. 2018;38(1):1–211.
Dodick DW. Diagnosing secondary and primary headache disorders. CONTINUUM: Lifelong Learn Neurol. 2021;27(3):572–85.
Loder E, Rizzoli P. Tension-type headache. BMJ. 2008;336(7635):88–92.
Nahas SJ. Cluster headache and other trigeminal autonomic cephalalgias. CONTINUUM: Lifelong Learn Neurol. 2021;27(3):633–51.
Hawkins K, Wang S, Rupnow MF. Indirect cost burden of migraine in the United States. J Occup Environ Med. 2007;49:368–74.
Bureau of Labor Statistics. CPI Inflation Calculator. https://www.bls.gov/data/inflation_calculator.htm. Published 2023. Accessed March 15, 2023.
Linde M, Gustavsson A, Stovner LJ, et al. The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol. 2012;19(5):703–11.
Fischera M, Marziniak M, Gralow I, Evers S. The incidence and prevalence of cluster headache: a meta-analysis of population-based studies. Cephalalgia. 2008;28(6):614–8.
Robbins MS. The psychiatric comorbidities of cluster headache. Curr Pain Headache Rep. 2013;17(2):313.
Ji Lee M, Cho S-J, Wook Park J, et al. Increased suicidality in patients with cluster headache. Cephalalgia. 2019;39(10):1249–56.
Friedman DI, De Ver Dye T. Migraine and the environment. Headache. 2009;49(6):941–52.
Yang AC, Fuh J-L, Huang NE, Shia B-C, Peng C-K, Wang S-J. Temporal associations between weather and headache: analysis by empirical mode decomposition. PLoS ONE. 2011;6(1): e14612.
Turner L, Molgaard C, Gardner C, Rothrock J, Stang P. Migraine trigger factors in a non-clinical Mexican-American population in San Diego county: implications for etiology. Cephalalgia. 1995;15(6):523–30.
von Mackensen S, Hoeppe P, Maarouf A, Tourigny P, Nowak D. Prevalence of weather sensitivity in Germany and Canada. Int J Biometeorol. 2005;49(3):156–66.
Szyszkowicz M, Kaplan G, Grafstein E, Rowe B. Emergency department visits for migraine and headache: a multi-city study. Int J Occup Med Environ Health. 2009;22(3):235–42.
Szyszkowicz M, Kousha T. Air pollution and emergency department visits for headache and migraine. Health Scope. 2016;5(3):e35122.
Szyszkowicz M, Rowe B, Kaplan G. Ambient sulphur dioxide exposure and emergency department visits for migraine in Vancouver, Canada. Int J Occup Med Environ Health. 2009;22(1):7–12.
Szyszkowicz, M., Stieb, D. M., & Rowe, B. H. Air pollution and daily ED visits for migraine and headache in Edmonton, Canada. Am J Emerg Med. 2009;27(4):391–96.
Silva-Néto R, Peres M, Valença M. Odorant substances that trigger headaches in migraine patients. Cephalalgia. 2014;34(1):14–21.
Silva-Néto RP, Rodrigues ÂB, Cavalcante DC, et al. May headache triggered by odors be regarded as a differentiating factor between migraine and other primary headaches? Cephalalgia. 2017;37(1):20–8.
Albanês Oliveira Bernardo A, Lys Medeiros F, Sampaio Rocha-Filho PA. Osmophobia and odor-triggered headaches in children and adolescents: prevalence, associated factors, and importance in the diagnosis of migraine. Headache. 2020;60(5):954–66.
Sjöstrand C, Savic I, Laudon-Meyer E, Hillert L, Lodin K, Waldenlind E. Migraine and olfactory stimuli. Curr Pain Headache Rep. 2010;14:244–51.
Maini K, Schuster NM. Headache and barometric pressure: a narrative review. Curr Pain Headache Rep. 2019;23:1–7.
Kilinç E, Schulz H, Kuiper GJ, et al. The procoagulant effects of fine particulate matter in vivo. Part Fibre Toxicol. 2011;8(1):1–3.
Calderón-Garcidueñas L, Solt AC, Henríquez-Roldán C, et al. Long-term air pollution exposure is associated with neuroinflammation, an altered innate immune response, disruption of the blood-brain barrier, ultrafine particulate deposition, and accumulation of amyloid β-42 and α-synuclein in children and young adults. Toxicol Pathol. 2008;36(2):289–310.
Chan C-C, Chuang K-J, Chien L-C, Chen W-J, Chang W-T. Urban air pollution and emergency admissions for cerebrovascular diseases in Taipei, Taiwan. Eur Heart J. 2006;27(10):1238–44.
Chen C-C, Tsai S-S, Yang C-Y. Association between fine particulate air pollution and daily clinic visits for migraine in a subtropical city: Taipei, Taiwan. Int J Environ Res Public Health. 2015;12(5):4697–708.
Chiu H-F, Weng Y-H, Chiu Y-W, Yang C-Y. Air pollution and daily clinic visits for headache in a subtropical city: Taipei, Taiwan. Int J Environ Res Public Health. 2015;12(2):2277–88.
Goadsby PJ, Edvinsson L. Human in vivo evidence for trigeminovascular activation in cluster headache Neuropeptide changes and effects of acute attacks therapies. Brain. 1994;117(3):427–34.
May A, Schwedt TJ, Magis D, Pozo-Rosich P, Evers S, Wang S-J. Cluster headache. Nat Rev Dis Prim. 2018;4(1):1–17.
Rozen TD, Fishman RS. Cluster headache in the United States of America: demographics, clinical characteristics, triggers, suicidality, and personal burden. Headache. 2012;52(1):99–113.
Kudrow L. The cyclic relationship of natural illumination to cluster period frequency. Cephalalgia. 1987;7(6_suppl):76–8.
Barloese M, Lund N, Petersen A, Rasmussen M, Jennum P, Jensen R. Sleep and chronobiology in cluster headache. Cephalalgia. 2015;35(11):969–78.
Naber WC, Fronczek R, Haan J, et al. The biological clock in cluster headache: a review and hypothesis. Cephalalgia. 2019;39(14):1855–66.
Lee H, Myung W, Cheong H-K, et al. Ambient air pollution exposure and risk of migraine: synergistic effect with high temperature. Environ Int. 2018;121:383–91.
Cui L, Conway GA, Jin L, et al. Increase in medical emergency calls and calls for central nervous system symptoms during a severe air pollution event, January 2013, Jinan City, China. Epidemiology. 2017;28:S67–73.
Li W, Bertisch SM, Mostofsky E, Buettner C, Mittleman MA. Weather, ambient air pollution, and risk of migraine headache onset among patients with migraine. Environ Int. 2019;132: 105100.
Yamaguchi H, Nozu K, Ishiko S, et al. Multivariate analysis of the impact of weather and air pollution on emergency department visits for night-time headaches among children: retrospective, clinical observational study. BMJ Open. 2021;11(4): e046520.
Zock J-P, Verheij R, Helbich M, et al. The impact of social capital, land use, air pollution and noise on individual morbidity in Dutch neighbourhoods. Environ Int. 2018;121:453–60.
Hong S-Y, Wan L, Lin H-J, Lin C-L, Wei C-C. Long-term ambient air pollutant exposure and risk of recurrent headache in children: a 12-year cohort study. Int J Environ Res Public Health. 2020;17(23):9140.
Amegah AK, Dakuu G, Mudu P, Jaakkola JJ. Particulate matter pollution at traffic hotspots of Accra, Ghana: levels, exposure experiences of street traders, and associated respiratory and cardiovascular symptoms. J Eposure Sci Environ Epidemiol. 2022;32(2):333–42.
Pressman A, Jacobson A, Eguilos R, et al. Prevalence of migraine in a diverse community—electronic methods for migraine ascertainment in a large integrated health plan. Cephalalgia. 2016;36(4):325–34.
Elser H, Morello-Frosch R, Jacobson A, et al. Air pollution, methane super-emitters, and oil and gas wells in Northern California: the relationship with migraine headache prevalence and exacerbation. Environ Health. 2021;20(1):1–14.
Prince PB, Rapoport AM, Sheftell FD, Tepper SJ, Bigal ME. The effect of weather on headache. Headache. 2004;44(6):596–602.
Lee M, Ohde S, Urayama KY, Takahashi O, Fukui T. Weather and health symptoms. Int J Environ Res Public Health. 2018;15(8):1670.
Sheridan SC. The redevelopment of a weather-type classification scheme for North America. Int J Climatol. 2002;22(1):51–68.
Elcik C, Fuhrmann CM, Sheridan SC, Mercer AE, Sherman, Morris K. Geographical variability in the relationship between synoptic weather type and emergency department visits for pain across North Carolina. Int J Biometeorol. 2021;66:559–572.
Akgün N, Demirel EA, Açikgöz M, Çelebi U, Köktürk F, Atasoy HT. The effect of weather variables on the severity, duration, and frequency of headacheattacks in the cases of episodic migraine and episodic tension-type headache. Turk J Med Sci. 2021;51(3):1406–12.
Olesen J. International classification of headache disorders. Lancet Neurol. 2018;17(5):396–7.
van Casteren DS, Verhagen IE, Onderwater GL, MaassenVanDenBrink A, Terwindt GM. Sex differences in prevalence of migraine trigger factors: a cross-sectional study. Cephalalgia. 2021;41(6):643–8.
Alkhalawi E, Orban E, Schramm S, Katsarava Z, Hoffmann B, Moebus S. Residential traffic noise exposure and headaches: results from the population-based heinz nixdorf recall study. Noise Health. 2021;23(108):1.
Ma J, Li C, Kwan M-P, Chai Y. A multilevel analysis of perceived noise pollution, geographic contexts and mental health in Beijing. Int J Environ Res Public Health. 2018;15(7):1479.
Schreurs, E., Jabben, J., & Verheijen, E. STAMINA‑model description: standard model instrumentation for noise assessments. National Instiute for Public Health and the Environment; 2010.
EIA U. The Distribution of US Oil and Natural Gas Wells by Production Rate. Washington, DC: US Department of Energy; 2019.
Casey JA, Savitz DA, Rasmussen SG, et al. Unconventional natural gas development and birth outcomes in Pennsylvania, USA. Epidemiology. 2016;27(2):163.
Tustin AW, Hirsch AG, Rasmussen SG, Casey JA, Bandeen-Roche K, Schwartz BS. Associations between unconventional natural gas development and nasal and sinus, migraine headache, and fatigue symptoms in Pennsylvania. Environ Health Perspect. 2017;125(2):189–97.
Remy LL, Clay T, Byers V, Rosenfeld PE. Hospital, health, and community burden after oil refinery fires, Richmond, California 2007 and 2012. Environ Health. 2019;18:1–14.
Hazeu, G.W. Operational land cover and land use mapping in the Netherlands. In: Land use and land cover mapping in europe: practices & trends. Elsevier. 2014;18:283–296.
Chetty-Mhlanga S, Fuhrimann S, Basera W, Eeftens M, Röösli M, Dalvie MA. Association of activities related to pesticide exposure on headache severity and neurodevelopment of school-children in the rural agricultural farmlands of the Western Cape of South Africa. Environ Int. 2021;146: 106237.
Win-Shwe T-T, Fujimaki H. Nanoparticles and neurotoxicity. Int J Mol Sci. 2011;12(9):6267–80.
Costa LG, Cole TB, Coburn J, Chang Y-C, Dao K, Roqué PJ. Neurotoxicity of traffic-related air pollution. Neurotoxicology. 2017;59:133–9.
Woodhouse A, Drummond PD. Mechanisms of increased sensitivity to noise and light in migraine headache. Cephalalgia. 1993;13(6):417–21.
Martin PR, Reece J, Forsyth M. Noise as a trigger for headaches: relationship between exposure and sensitivity. Headache. 2006;46(6):962–72.
Woimant F, Trocello J-M. Disorders of heavy metals. Handb Clin Neurol. 2014;120:851–64.
Tanner CM, Goldman SM, Ross GW, Grate SJ. The disease intersection of susceptibility and exposure: chemical exposures and neurodegenerative disease risk. Alzheimers Dement. 2014;10:S213–25.
Mostafalou S, Abdollahi M. The link of organophosphorus pesticides with neurodegenerative and neurodevelopmental diseases based on evidence and mechanisms. Toxicology. 2018;409:44–52.
Sánchez-Santed F, Colomina MT, Hernández EH. Organophosphate pesticide exposure and neurodegeneration. Cortex. 2016;74:417–26.
Rocha-Filho PAS, Marques KS, Torres RCS, Leal KNR. Osmophobia and headaches in primary care: prevalence, associated factors, and importance in diagnosing migraine. Headache. 2015;55(6):840–5.
Silva-Néto RP, Peres MFP, Valença MM. Accuracy of osmophobia in the differential diagnosis between migraine and tension-type headache. J Neurol Sci. 2014;339(1–2):118–22.
Zanchin G, Dainese F, Mainardi F, Mampreso E, Perin C, Maggioni F. Osmophobia in primary headaches. J Headache Pain. 2005;6:213–5.
Guadalupe-Fernandez V, De Sario M, Vecchi S, et al. Industrial odour pollution and human health: a systematic review and meta-analysis. Environ Health. 2021;20(1):1–21.
Afata TN, Mekonen S, Shekelifa M, Tucho GT. Prevalence of pesticide use and occupational exposure among small-scale farmers in Western Ethiopia. Environ Health Insights. 2022;16:11786302211072950.
Afshari M, Poorolajal J, Assari MJ, Rezapur-Shahkolai F, Karimi-Shahanjarini A. Acute pesticide poisoning and related factors among farmers in rural Western Iran. Toxicol Ind Health. 2018;34(11):764–77.
Bhandari G, Atreya K, Yang X, Fan L, Geissen V. Factors affecting pesticide safety behaviour: the perceptions of Nepalese farmers and retailers. Sci Total Environ. 2018;631:1560–71.
Buralli RJ, Ribeiro H, Iglesias V, et al. Occupational exposure to pesticides and health symptoms among family farmers in Brazil. Revista de Saúde Pública. 2020;54(133):1–13.
Evaristo A, Pedroso DO, Rech NL, et al. Pesticides and farmers’ health: an analysis of variables related to management and property. An Acad Bras Ciênc. 2022;94: e20211335.
Memon QUA, Wagan SA, Chunyu D, Shuangxi X, Jingdong L, Damalas CA. Health problems from pesticide exposure and personal protective measures among women cotton workers in southern Pakistan. Sci Total Environ. 2019;685:659–66.
Mwabulambo SG, Mrema EJ, Ngowi AV, Mamuya S. Health symptoms associated with pesticides exposure among flower and onion pesticide applicators in Arusha region. Ann Glob Health. 2018;84(3):369.
Nankongnab N, Kongtip P, Tipayamongkholgul M, Bunngamchairat A, Sitthisak S, Woskie S. Difference in accidents, health symptoms, and ergonomic problems between conventional farmers using pesticides and organic farmers. J Agromed. 2020;25(2):158–65.
Sai MVS, Revati GD, Ramya R, Swaroop AM, Maheswari E, Kumar MM. Knowledge and perception of farmers regarding pesticide usage in a rural farming village, Southern India. Indian J Occup Environ Med. 2019;23(1):32.
Sonchieu J, Akono EN, Ngwamitang CT, Ngassoum BM. Heath risk among pesticide sellers in Bamenda (Cameroon) and peripheral areas. Environ Sci Pollut Res. 2018;25:9454–60.
Tiwari S, Sapkota N, Tiwari S, Sapkota B. Association between pesticide exposure and neurobehavioral performance of agricultural workers: a cross-sectional study. Brain Behav. 2022;12(7): e2641.
Elser H, Rowland ST, Marek MS, et al. Wildfire smoke exposure and emergency department visits for headache: a case-crossover analysis in California, 2006–2020. Headache. 2023;63(1):94–103.
Silberstein S, Tfelt-Hansen P, Dodick D, et al. Guidelines for controlled trials of prophylactic treatment of chronic migraine in adults. Cephalalgia. 2008;28(5):484–95.
Penzien DB, Andrasik F, Freidenberg BM, et al. Guidelines for trials of behavioral treatments for recurrent headache: American Headache Society Behavioral Clinical Trials Workgroup. Headache. 2005;45:S110–32.
Luedtke K, Basener A, Bedei S, et al. Outcome measures for assessing the effectiveness of non-pharmacological interventions in frequent episodic or chronic migraine: a Delphi study. BMJ Open. 2020;10(2): e029855.
Andrasik F, Lipchik GL, McCrory DC, Wittrock DA. Outcome measurement in behavioral headache research: headache parameters and psychosocial outcomes. Headache. 2005;45(5):429–37.
Haywood KL, Mars TS, Potter R, Patel S, Matharu M, Underwood M. Assessing the impact of headaches and the outcomes of treatment: a systematic review of patient-reported outcome measures (PROMs). Cephalalgia. 2018;38(7):1374–86.
Lipton RB, Dodick D, Sadovsky R, et al. A self-administered screener for migraine in primary care: the ID migraine™ validation study. Neurology. 2003;61(3):375–82.
Angrist JD, Pischke J-S. Parallel worlds: fixed effects, differences-in-differences, and panel data. In: Mostly harmless econometrics. Princeton University Press; 2008:221–248.
Sheridan P, McElroy S, Casey J, Benmarhnia T. Using the generalized synthetic control method to estimate the impact of extreme weather events on population health. Epidemiology. 2022;33(6):788–96.
Casey JA, Schwartz BS, Stewart WF, Adler NE. Using electronic health records for population health research: a review of methods and applications. Annu Rev Public Health. 2016;37:61–81.
Beghi E, Bussone G, D’Amico D, et al. Headache, anxiety and depressive disorders: the HADAS study. J Headache Pain. 2010;11:141–50.
Baskin SM, Lipchik GL, Smitherman TA. Mood and anxiety disorders in chronic headache. Headache. 2006;46:S76–87.
Breslau N, Schultz L, Stewart W, Lipton R, Lucia V, Welch K. Headache and major depression: is the association specific to migraine? Neurology. 2000;54(2):308–308.
Louter MA, Wilbrink LA, Haan J, et al. Cluster headache and depression. Neurology. 2016;87(18):1899–906.
Peterlin BL, Tietjen GE, Brandes JL, et al. Posttraumatic stress disorder in migraine. Headache. 2009;49(4):541–51.
De Leeuw R, Schmidt JE, Carlson CR. Traumatic stressors and post-traumatic stress disorder symptoms in headache patients. Headache. 2005;45(10):1365–74.
Casey JA, Wilcox HC, Hirsch AG, Pollak J, Schwartz BS. Associations of unconventional natural gas development with depression symptoms and disordered sleep in Pennsylvania. Sci Rep. 2018;8(1):1–10.
Hirsch JK, Bryant Smalley K, Selby-Nelson EM, et al. Psychosocial impact of fracking: a review of the literature on the mental health consequences of hydraulic fracturing. Int J Ment Heal Addict. 2018;16(1):1–15.
Elser H, Goldman-Mellor S, Morello-Frosch R, Deziel NC, Ranjbar K, Casey JA. Petro-riskscapes and environmental distress in West Texas: community perceptions of environmental degradation, threats, and loss. Energy Res Soc Sci. 2020;70: 101798.
Casey, JA, Goldman-Mellor, S, Catalano, R. Association between Oklahoma earthquakes and anxiety-related google search episodes. Environ Epidemio. 2018;2(2):e016.
Elser H, Kempinsky A, Goldman-Mellor S, et al. Manmade earthquakes and healthcare visits for anxiety disorders in Oklahoma, 2010–2019. Environ Epidemiol. 2023;7(1): e232.
Fan S-J, Heinrich J, Bloom MS, et al. Ambient air pollution and depression: a systematic review with meta-analysis up to 2019. Sci Total Environ. 2020;701: 134721.
Power MC, Kioumourtzoglou M-A, Hart JE, Okereke OI, Laden F, Weisskopf MG. The relation between past exposure to fine particulate air pollution and prevalent anxiety: observational cohort study. BMJ. 2015;350:h1111.
Arcaya MC, Lowe SR, Asad AL, Subramanian S, Waters MC, Rhodes J. Association of posttraumatic stress disorder symptoms with migraine and headache after a natural disaster. Health Psychol. 2017;36(5):411.
Zhang Y, Zhang J, Ren R, Tang X. Bidirectional associations of insomnia symptoms with somatic complaints and posttraumatic stress disorder in child and adolescent earthquake survivors: a longitudinal study. Sleep Breath. 2020;24:311–20.
Carmassi C, Dell’Oste V, Barberi FM, et al. Do somatic symptoms relate to PTSD and gender after earthquake exposure? A cross-sectional study on young adult survivors in Italy. CNS Spectr. 2021;26(3):268–74.
Hagen K, Vatten L, Stovner L, Zwart J, Krokstad S, Bovim G. Low socio-economic status is associated with increased risk of frequent headache: a prospective study of 22718 adults in Norway. Cephalalgia. 2002;22(8):672–9.
Stewart WF, Lipton RB, Celentano DD, Reed ML. Prevalence of migraine headache in the United States: relation to age, income, race, and other sociodemographic factors. JAMA. 1992;267(1):64–9.
Winter AC, Berger K, Buring JE, Kurth T. Associations of socioeconomic status with migraine and non-migraine headache. Cephalalgia. 2012;32(2):159–70.
Lipfert, FW. Air pollution and poverty: does the sword cut both ways? Journal of Epidemiology and Community Health. 2004;58:2–3.
Josey KP, Delaney SW, Wu X, et al. Air pollution and mortality at the intersection of race and social class. N Engl J Med. 2023;388(15):1396–1404.
Casey JA, Morello-Frosch R, Mennitt DJ, Fristrup K, Ogburn EL, James P. Race/ethnicity, socioeconomic status, residential segregation, and spatial variation in noise exposure in the contiguous United States. Environ Health Perspect. 2017;125(7): 077017.
Nardone A, Rudolph KE, Morello-Frosch R, Casey JA. Redlines and greenspace: the relationship between historical redlining and 2010 greenspace across the United States. Environ Health Perspect. 2021;129(1): 017006.
Das GM. Population, poverty, and climate change. World Bank Res Observ. 2014;29(1):83–108.
Berberian AG, Gonzalez DJ, Cushing LJ. Racial disparities in climate change-related health effects in the United States. Curr Environ Health Report. 2022;9(3):451–64.
U.S. Environmental Protection Agency. Climate Change and Social Vulnterability in the United States: A Focus on Six Impacts. https://www.epa.gov/system/files/documents/2021-09/climate-vulnerability_september-2021_508.pdf. Published 2021. Accessed April 18, 2023.
Acknowledgements
The editors would like to thank Molly Kile for handling the review of this manuscript.
Funding
J.A.C. was supported by the National Institute of Environmental Health Sciences grant R00-ES0207023. The conclusions expressed are solely those of the authors.
Ethics declarations
Ethical Approval
Not applicable.
Conflict of Interest
The authors declare competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Elser, H., Kruse, C.F.G., Schwartz, B.S. et al. The Environment and Headache: a Narrative Review. Curr Envir Health Rpt 11, 184–203 (2024). https://doi.org/10.1007/s40572-024-00449-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40572-024-00449-4