Abstract
Purpose of Review
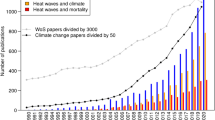
Climate change will affect mortality associated with both ambient temperature and air pollution. Because older adults have elevated vulnerability to both non-optimal ambient temperature (heat and cold) and air pollution, population aging can amplify future population vulnerability to these stressors through increasing the number of vulnerable older adults. We aimed to review recent evidence on projections of temperature- or air pollution-related mortality burden (i.e., number of deaths) under combined climate change and population aging scenarios, with a focus on evaluating the role of population aging in assessing these health impacts of climate change. We included studies published between 2014 and 2019 with age-specific population projections.
Recent Findings
We reviewed 16 temperature projection studies and 15 air pollution projection studies. Nine of the temperature studies and four of the air pollution studies took population aging into account by performing age-stratified analyses that utilized age-specific relationships between temperature or air pollution exposures and mortality (i.e., age-specific exposure-response functions (ERFs)). Population aging amplifies the projected mortality burden of temperature and air pollution under a warming climate. Compared with a constant population scenario, population aging scenarios lead to less reduction or even increases in cold-related mortality burden, resulting in substantial net increases in future overall (heat and cold) temperature-related mortality burden.
Summary
There is strong evidence suggesting that to accurately assess the future temperature- and air pollution-related mortality burden of climate change, investigators need to account for the amplifying effect of population aging. Thus, all future studies should incorporate age-specific population size projections and age-specific ERFs into their analyses. These studies would benefit from refinement of age-specific ERF estimates.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Smith KR, Woodward A, Campbell-Lendrum D, Chadee DD, Honda Y, Liu Q, et al. Human health: impacts, adaptation and co-benefits. In: Field CB, Barros VR, Dokken DJ, Mach KJ, Mastrandrea MD, Bilir TE, et al., editors. Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. New York, NY, USA: Cambridge University Press; 2017. p. 709–54.
Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Belesova K, Boykoff M, et al. The 2019 report of The Lancet Countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet. 2019;394(10211):1836–78. https://doi.org/10.1016/S0140-6736(19)32596-6.
Ye X, Wolff R, Yu W, Vaneckova P, Pan X, Tong S. Ambient temperature and morbidity: a review of epidemiological evidence. Environ Health Perspect. 2012;120(1):19–28. https://doi.org/10.1289/ehp.1003198.
Anderson BG, Bell ML. Weather-related mortality: how heat, cold, and heat waves affect mortality in the United States. Epidemiology. 2009;20(2):205–13. https://doi.org/10.1097/EDE.0b013e318190ee08.
Schneider A, Rückerl R, Breitner S, Wolf K, Peters A. Thermal control, weather, and aging. Curr Environ Health Rep. 2017;4:21–9. https://doi.org/10.1007/s40572-017-0129-0.
Fiore AM, Naik V, Leibensperger EM. Air quality and climate connections. J Air Waste Manage Assoc. 2015;65(6):645–85. https://doi.org/10.1080/10962247.2015.1040526.
Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 2017;389(10082):1907–18. https://doi.org/10.1016/S0140-6736(17)30505-6.
Gasparrini A, Guo YM, Hashizume M, Lavigne E, Zanobetti A, Schwartz J, et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet. 2015;386(9991):369–75. https://doi.org/10.1016/s0140-6736(14)62114-0.
United Nations Department of Economic Social Affairs Population Division. World Population Prospects 2019. New York: United Nations.
Shumake KL, Sacks JD, Lee JS, Johns DO. Susceptibility of older adults to health effects induced by ambient air pollutants regulated by the European Union and the United States. Aging Clin Exp Res. 2013;25(1):3–8. https://doi.org/10.1007/s40520-013-0001-5.
Son J, Liu JC, Bell ML. Temperature-related mortality: a systematic review and investigation of effect modifiers. Environ Res Lett. 2019;14(7):073004. https://doi.org/10.1088/1748-9326/ab1cdb.
Di Q, Dai L, Wang Y, Zanobetti A, Choirat C, Schwartz JD, et al. Association of short-term exposure to air pollution with mortality in older adults. JAMA. 2017;318(24):2446–56. https://doi.org/10.1001/jama.2017.17923.
Kinney PL. Interactions of climate change, air pollution, and human health. Curr Environ Health Rep. 2018;5(1):179–86. https://doi.org/10.1007/s40572-018-0188-x.
Orru H, Ebi KL, Forsberg B. The interplay of climate change and air pollution on health. Curr Environ Health Rep. 2017;4(4):504–13. https://doi.org/10.1007/s40572-017-0168-6.
Huang C, Barnett AG, Wang X, Vaneckova P, FitzGerald G, Tong S. Projecting future heat-related mortality under climate change scenarios: a systematic review. Environ Health Perspect. 2011;119(12):1681–90. https://doi.org/10.1289/ehp.1103456.
Sujaritpong S, Dear K, Cope M, Walsh S, Kjellstrom T. Quantifying the health impacts of air pollution under a changing climate-a review of approaches and methodology. Int J Biometeorol. 2014;58(2):149–60. https://doi.org/10.1007/s00484-012-0625-8.
Madaniyazi L, Guo Y, Yu W, Tong S. Projecting future air pollution-related mortality under a changing climate: progress, uncertainties and research needs. Environ Int. 2015;75:21–32. https://doi.org/10.1016/j.envint.2014.10.018.
Sanderson M, Arbuthnott K, Kovats S, Hajat S, Falloon P. The use of climate information to estimate future mortality from high ambient temperature: a systematic literature review. PLoS One. 2017;12(7):e0180369. https://doi.org/10.1371/journal.pone.0180369.
Chen R, Yin P, Wang L, Liu C, Niu Y, Wang W, et al. Association between ambient temperature and mortality risk and burden: time series study in 272 main Chinese cities. BMJ. 2018;363:k4306. https://doi.org/10.1136/bmj.k4306.
Fu SH, Gasparrini A, Rodriguez PS, Jha P. Mortality attributable to hot and cold ambient temperatures in India: a nationally representative case-crossover study. PLoS Med. 2018;15(7):e1002619. https://doi.org/10.1371/journal.pmed.1002619.
Pascal M, Wagner V, Corso M, Laaidi K, Ung A, Beaudeau P. Heat and cold related-mortality in 18 French cities. Environ Int. 2018;121:189–98. https://doi.org/10.1016/j.envint.2018.08.049.
Limaye VS, Vargo J, Harkey M, Holloway T, Patz JA. Climate change and heat-related excess mortality in the Eastern USA. Ecohealth. 2018;15(3):485–96. https://doi.org/10.1007/s10393-018-1363-0.
Kim DW, Deo RC, Chung JH, Lee JS. Projection of heat wave mortality related to climate change in Korea. Nat Hazards. 2016;80(1):623–37. https://doi.org/10.1007/s11069-015-1987-0.
•• Hajat S, Vardoulakis S, Heaviside C, Eggen B. Climate change effects on human health: projections of temperature-related mortality for the UK during the 2020s, 2050s and 2080s. J Epidemiol Community Health. 2014;68(7):641–8. https://doi.org/10.1136/jech-2013-202449This study, one of the first to take into account both age-specific changes in population size and age-specific ERFs in assessing cold-related mortality under climate change, suggests that the reduction in cold-related mortality in the UK between the 2000s and the 2050s would be substantially smaller (2%) than under an assumption of constant population (26%).
• Vardoulakis S, Dear K, Hajat S, Heaviside C, Eggen B, AJ MM. Comparative assessment of the effects of climate change on heat- and cold-related mortality in the United Kingdom and Australia. Environ Health Perspect. 2014;122(12):1285–92. https://doi.org/10.1289/ehp.1307524This study illustrates that under a constant population assumption, a large reduction in cold-related mortality would result in a net decrease in the temperature-related mortality burden in the United Kingdom and Australia between the 2020s and 2050s, whereas taking into account age-specific changes in population size and age-specific ERFs largely offsets the decrease in cold-related mortality, leading to a substantial net increase in overall temperature-related mortality from cold and heat combined.
•• Lee JY, Kim H. Projection of future temperature-related mortality due to climate and demographic changes. Environ Int. 2016;94:489–94. https://doi.org/10.1016/j.envint.2016.06.007This study shows the dominant influence of population aging compared with changes in the total population size (not taking changes in the age structure into account) in projecting future temperature-related mortality under a full range of plausible combinations of climate (four RCPs) and population scenarios (three UN WPP scenarios).
Lee JY, Kim E, Lee WS, Chae Y, Kim H. Projection of future mortality due to temperature and population changes under Representative Concentration Pathways and Shared Socioeconomic Pathways. Int J Environ Res Public Health. 2018;15(4). https://doi.org/10.3390/ijerph15040822.
Gronlund CJ, Cameron L, Shea C, O'Neill MS. Assessing the magnitude and uncertainties of the burden of selected diseases attributable to extreme heat and extreme precipitation under a climate change scenario in Michigan for the period 2041-2070. Environ Health. 2019;18(1):40. https://doi.org/10.1186/s12940-019-0483-5.
Lee JY, Lee WS, Ebi KL, Kim H. Temperature-related summer mortality under multiple climate, population, and adaptation scenarios. Int J Environ Res Public Health. 2019;16(6). https://doi.org/10.3390/ijerph16061026.
Liu T, Ren Z, Zhang Y, Feng B, Lin H, Xiao J, et al. Modification effects of population expansion, ageing, and adaptation on heat-related mortality risks under different climate change scenarios in Guangzhou, China. Int J Environ Res Public Health. 2019;16(3). https://doi.org/10.3390/ijerph16030376.
Wang YJ, Wang AQ, Zhai JQ, Tao H, Jiang T, Su BD et al. Tens of thousands additional deaths annually in cities of China between 1.5 degrees C and 2.0 degrees C warming. Nat Commun. 2019;10:7. Doi:https://doi.org/10.1038/s41467-019-11283-w.
Marsha A, Sain SR, Heaton MJ, Monaghan AJ, Wilhelmi OV. Influences of climatic and population changes on heat-related mortality in Houston, Texas, USA. Clim Change. 2018;146(3–4):471–85. https://doi.org/10.1007/s10584-016-1775-1.
Markandya A, Sampedro J, Smith SJ, Van Dingenen R, Pizarro-Irizar C, Arto I, et al. Health co-benefits from air pollution and mitigation costs of the Paris Agreement: a modelling study. Lancet Planet Health. 2018;2(3):e126–e33. https://doi.org/10.1016/s2542-5196(18)30029-9.
Shindell D, Faluvegi G, Seltzer K, Shindell C. Quantified, localized health benefits of accelerated carbon dioxide emissions reductions. Nat Clim Chang. 2018;8(4):291–5. https://doi.org/10.1038/s41558-018-0108-y.
Saari RK, Mei Y, Monier E, Garcia-Menendez F. Effect of health-related uncertainty and natural variability on health impacts and cobenefits of climate policy. Environ Sci Technol. 2019;53(3):1098–108. https://doi.org/10.1021/acs.est.8b05094.
Zapata CB, Yang C, Yeh S, Ogden J, Kleeman MJ. Low-carbon energy generates public health savings in California. Atmos Chem Phys. 2018;18(7):4817–30. https://doi.org/10.5194/acp-18-4817-2018.
Burnett RT, Pope CA, Ezzati M, Olives C, Lim SS, Mehta S, et al. An integrated risk function for estimating the global burden of disease attributable to ambient fine particulate matter exposure. Environ Health Perspect. 2014;122(4):397–403. https://doi.org/10.1289/ehp.1307049.
•• Silva RA, West JJ, Lamarque JF, Shindell DT, Collins WJ, Dalsoren S, et al. The effect of future ambient air pollution on human premature mortality to 2100 using output from the ACCMIP model ensemble. Atmos Chem Phys. 2016;16(15):9847–62. https://doi.org/10.5194/acp-16-9847-2016This was one of the first global studies to apply age-specific population size projections and age-specific ERFs in projecting future mortality burden attributable to long-term PM2.5 exposure.
Silva RA, West JJ, Lamarque JF, Shindell DT, Collins WJ, Faluvegi G, et al. Future global mortality from changes in air pollution attributable to climate change. Nat Clim Chang. 2017;7(11):845. https://doi.org/10.1038/nclimate3427.
Chowdhury S, Dey S, Smith KR. Ambient PM2.5 exposure and expected premature mortality to 2100 in India under climate change scenarios. Nat Commun. 2018;9(1):318. https://doi.org/10.1038/s41467-017-02755-y.
•• Chen K, Fiore AM, Chen R, Jiang L, Jones B, Schneider A, et al. Future ozone-related acute excess mortality under climate and population change scenarios in China: a modeling study. PLoS Med. 2018;15(7):e1002598. https://doi.org/10.1371/journal.pmed.1002598This was the first study to quantify the amplifying effect of population aging on short-term ozone-related mortality while simultaneously accounting for age-specific changes in population size, age-specific ERFs, and age-specific BMRs.
Yin P, Chen R, Wang L, Meng X, Liu C, Niu Y, et al. Ambient ozone pollution and daily mortality: a nationwide study in 272 Chinese cities. Environ Health Perspect. 2017;125(11):117006. https://doi.org/10.1289/EHP1849.
Carter TR, Fronzek S, Inkinen A, Lahtinen I, Lahtinen M, Mela H, et al. Characterising vulnerability of the elderly to climate change in the Nordic region. Reg Environ Chang. 2016;16(1):43–58. https://doi.org/10.1007/s10113-014-0688-7.
Li T, Horton RM, Bader DA, Zhou M, Liang X, Ban J, et al. Aging will amplify the heat-related mortality risk under a changing climate: projection for the elderly in Beijing, China. Sci Rep. 2016;6:28161. https://doi.org/10.1038/srep28161.
Sun J, Fu JS, Huang K, Gao Y. Estimation of future PM2.5- and ozone-related mortality over the continental United States in a changing climate: an application of high-resolution dynamical downscaling technique. J Air Waste Manage Assoc. 2015;65(5):611–23. https://doi.org/10.1080/10962247.2015.1033068.
Achakulwisut P, Mickley LJ, Anenberg SC. Drought-sensitivity of fine dust in the US Southwest: implications for air quality and public health under future climate change. Environ Res Lett. 2018;13(5):11. https://doi.org/10.1088/1748-9326/aabf20.
Achakulwisut P, Anenberg SC, Neumann JE, Penn SL, Weiss N, Crimmins A, et al. Effects of increasing aridity on ambient dust and public health in the U.S. Southwest under climate change. Geohealth. 2019;3(5):127–44. https://doi.org/10.1029/2019gh000187.
Hong C, Zhang Q, Zhang Y, Davis SJ, Tong D, Zheng Y, et al. Impacts of climate change on future air quality and human health in China. Proc Natl Acad Sci U S A. 2019;116(35):17193–200. https://doi.org/10.1073/pnas.1812881116.
Yang PL, Zhang Y, Wang K, Doraiswamy P, Cho SH. Health impacts and cost-benefit analyses of surface O3 and PM2.5 over the US under future climate and emission scenarios. Environ Res. 2019;178:15. https://doi.org/10.1016/j.envres.2019.108687.
Orru H, Astrom C, Andersson C, Tamm T, Ebi KL, Forsberg B. Ozone and heat-related mortality in Europe in 2050 significantly affected by changes in climate, population and greenhouse gas emission. Environ Res Lett. 2019;14(7):8. https://doi.org/10.1088/1748-9326/ab1cd9.
Geels C, Andersson C, Hanninen O, Lanso AS, Schwarze PE, Skjoth CA, et al. Future premature mortality due to O3, secondary inorganic aerosols and primary PM in Europe--sensitivity to changes in climate, anthropogenic emissions, population and building stock. Int J Environ Res Public Health. 2015;12(3):2837–69. https://doi.org/10.3390/ijerph120302837.
Gasparrini A, Guo Y, Sera F, Vicedo-Cabrera AM, Huber V, Tong S, et al. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet Health. 2017;1(9):e360–e7. https://doi.org/10.1016/S2542-5196(17)30156-0.
Vicedo-Cabrera AM, Guo Y, Sera F, Huber V, Schleussner C-F, Mitchell D, et al. Temperature-related mortality impacts under and beyond Paris Agreement climate change scenarios. Clim Chang. 2018;150(3):391–402. https://doi.org/10.1007/s10584-018-2274-3.
Brook RD, Rajagopalan S, Pope CA, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease. Circulation. 2010;121(21):2331–78. https://doi.org/10.1161/CIR.0b013e3181dbece1.
Bell ML, Zanobetti A, Dominici F. Who is more affected by ozone pollution? A systematic review and meta-analysis. Am J Epidemiol. 2014;180(1):15–28. https://doi.org/10.1093/aje/kwu115.
Jerrett M, Burnett RT, Pope CA III, Ito K, Thurston G, Krewski D, et al. Long-term ozone exposure and mortality. N Engl J Med. 2009;360(11):1085–95. https://doi.org/10.1056/NEJMoa0803894.
Turner MC, Jerrett M, Pope CA III, Krewski D, Gapstur SM, Diver WR, et al. Long-term ozone exposure and mortality in a large prospective study. Am J Respir Crit Care Med. 2016;193(10):1134–42. https://doi.org/10.1164/rccm.201508-1633OC.
Lim CC, Hayes RB, Ahn J, Shao Y, Silverman DT, Jones RR, et al. Long-term exposure to ozone and cause-specific mortality risk in the U.S. Am J Respir Crit Care Med. 2019;200(8):1022–31. https://doi.org/10.1164/rccm.201806-1161OC.
O'Neill BC, Tebaldi C, van Vuuren DP, Eyring V, Friedlingstein P, Hurtt G, et al. The Scenario Model Intercomparison Project (ScenarioMIP) for CMIP6. Geosci Model Dev. 2016;9(9):3461–82. https://doi.org/10.5194/gmd-9-3461-2016.
Morefield PE, Fann N, Grambsch A, Raich W, Weaver CP. Heat-related health impacts under scenarios of climate and population change. Int J Environ Res Public Health. 2018;15(11). https://doi.org/10.3390/ijerph15112438.
Striessnig E, Gao J, O’Neill BC, Jiang L. Empirically based spatial projections of US population age structure consistent with the shared socioeconomic pathways. Environ Res Lett. 2019;14(11):114038. https://doi.org/10.1088/1748-9326/ab4a3a.
Foreman KJ, Marquez N, Dolgert A, Fukutaki K, Fullman N, McGaughey M, et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016–40 for 195 countries and territories. Lancet. 2018;392(10159):2052–90. https://doi.org/10.1016/S0140-6736(18)31694-5.
Astrom C, Astrom DO, Andersson C, Ebi KL, Forsberg B. Vulnerability reduction needed to maintain current burdens of heat-related mortality in a changing climate-magnitude and determinants. Int J Environ Health Res. 2017;14(7):10. https://doi.org/10.3390/ijerph14070741.
Huang J, Li GX, Liu Y, Huang J, Xu GZ, Qian XJ, et al. Projections for temperature-related years of life lost from cardiovascular diseases in the elderly in a Chinese city with typical subtropical climate. Environ Res. 2018;167:614–21. https://doi.org/10.1016/j.envres.2018.08.024.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Dubrow reports a grant from the High Tide Foundation during the conduct of the study. The other authors declare they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Susceptibility Factors in Environmental Health
Rights and permissions
About this article
Cite this article
Chen, K., Vicedo-Cabrera, A.M. & Dubrow, R. Projections of Ambient Temperature- and Air Pollution-Related Mortality Burden Under Combined Climate Change and Population Aging Scenarios: a Review. Curr Envir Health Rpt 7, 243–255 (2020). https://doi.org/10.1007/s40572-020-00281-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40572-020-00281-6