Abstract
Purpose
To test the feasibility of US/CT fusion imaging to guide lumbar intradiscal O2/O3 therapy to treat discogenic degenerative low back pain due to lumbar disc herniation (LDH).
Methods
We retrospectively included consecutive patients affected by low back pain and/or sciatica due to LDH resistant to conservative therapies, who underwent to lumbar intradiscal O2/O3 injection under CT/US fusion imaging guidance (Fusion Group) and standard CT guidance (Control Group). For each procedure, we collected procedure operative time, room utilization time, number of CT passes, complications, and O2/O3 intradiscal diffusion adequacy. Technical success was defined as the ability to complete the procedure as initially planned to reach the disc. Technical efficacy was based on O2/O3 intradiscal diffusion adequacy, as demonstrated by the last CT scan.
Results
Six patients (4 males; mean age: 68 ± 15 years) were included in the Fusion group, six (4 males; mean age: 66 ± 12 years) in Control group. No complications were observed in both groups. In Fusion group we found significantly lower room utilization time (30 ± 6 min vs. 46 ± 10 min, p = 0.008), procedure operative time (14 ± 3 min vs. 24 ± 6 min, p = 0.008), and number of CT passes (2 [2,2] vs. 3 [3,3], p = 0.006) than in Control Group, respectively. Technical success and efficacy were 100% in both Groups.
Conclusion
CT/US fusion imaging seems to be a feasible and safe guidance for intradiscal O2/O3 injections, allowing decrease of procedure time and number of CT passes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Low back pain (LBP) is a quite common condition, particularly in elderly, affecting about 80% of people during their lives [1]. Hence, this condition has a non-negligible social and economic relevance. It is generally related to degenerative changes of the lumbar spine, and it has been associated to lumbar disc herniation (LDH) in 9% of patients [2]. As a matter of say, surgery is considered as the last and less desirable option, although it may become necessary if neurological symptoms occur. LBP is generally first approached with conservative treatments such as anti-inflammatory drugs, physical therapy, life modifications, specific exercises, and weight loss. As a second step, minimally invasive therapies can be provided, mostly including injections around the spine. Among them, an increasing interest and use have been observed over the last years regarding percutaneous injection of oxygen-ozone (O2/O3) mixtures. These injections may have different targets, including the epidural space, foramina, facets, and intervertebral discs.
The impact of ozone in LDH is thought to be related to its anti-oxidant and anti-inflammatory properties, which can contrast the inflammatory response triggered by LDH as an attempt to decrease the size of the hernia itself. Although controversial results have been reported, recent data support the use of O2/O3injections for treating LDH, with substantial and significant clinical improvement after treatment, as reported by a recent meta-analysis [3]. Injections can be performed under imaging guidance (CT, fluoroscopy or, less frequently, ultrasound), which ensures needle tip positioning exactly at the specific target [4,5,6,7,8]. Alternatively, injections may be performed without imaging guidance in the muscular paravertebral tissues at the level of pathologic disc. Notably, imaging guidance is essential for an accurate periradicular, intraforaminal, or intradiscal injection. In this setting, a recent meta-analysis has shown that image-guided O2/O3 mixture injection had better performance for LBP when compared to non-image-guided procedures, with better effectiveness and lower age-related variability in outcomes [4]. Ultrasound (US) guidance has been rarely used for O2/O3 injections in the spine, for procedures involving foraminal [5] and paravertebral muscles [8] injections. No previous studies focused on the application of US to guide O2/O3 injections in the lumbar discs, due to deep location of the disc that can be hardly recognized on US.
Over the last years, more and more applications have been introduced for fusion imaging to match real-time US with other more panoramic cross-sectional modalities, such as computed tomography (CT) and magnetic resonance imaging (MRI) [9]. This technology has been improved to integrate US with pre-intervention CT or MRI, making “visible” a target that cannot be visualized on US. Further, needle tracking software may enable following the needle path even when the tip is not directly seen [9]. This technology is routinely used for several procedures involving prostate, liver, and brain [10,11,12], while in the spine its use has not been extensively reported, with limited studies having proven its feasibility and efficacy for facet and sacroiliac joints injections, and bone biopsies [9, 13, 14]. Fusion imaging guidance has the potential of reducing the number of CT scans that should be acquired to track the needle, and in turn radiation exposure and procedure duration, improving safety and effectiveness of the intervention. Therefore, we carried on a pilot study to test the feasibility of US/CT fusion imaging and virtual navigation in the guidance of lumbar intradiscal O2/O3 therapy for treating LDH.
Materials and methods
Study design
This is a single-center retrospective observational study. Institutional Review Board approval was obtained and informed consent was waived. After matching imaging and clinical data, our database was anonymized to remove any connections between data and patients’ identity according to the General Data Protection Regulation.
We retrospectively included consecutive patients admitted to the Radiology Department of IRCCS Ospedale Galeazzi-Sant'Ambrogio to be subjected to lumbar intradiscal O2/O3therapy in May 2023. Included patients were affected by LBP and/or sciatica due to LDH resistant to conservative therapies (anti-inflammatory medications, physical therapy, and life changes) and were sent by a referral orthopaedist for lumbar injections. Exclusion criteria were: (i) pregnancy; (ii) coagulation impairment; (iii) motor deficits; (iv) spine infections; (v) neoplastic vertebral lesions; and (vi) calcified disc herniations [15]. Our institutional database was searched for standard CT-guided procedures like those subjected to injections under fusion imaging in terms of age, gender, and disc level. Data from these patients were used as controls. Therefore, patients included in this study were divided in those subjected to standard percutaneous CT-guided lumbar intradiscal O2/O3 therapy (Control Group) and those treated using US/CT fusion imaging and virtual navigation as guidance for injections (Fusion Group).
Standard and CT + US fusion-guided injection
Interventions were performed in the CT suite by one musculoskeletal radiologist with 30 years of experience in intradiscal injections and by one musculoskeletal radiologist with 7 years of experience in interventional procedures but without experience in intradiscal injections, although under the supervision of the experienced operator. The coagulation profile was evaluated within 48 h of the procedure and anticoagulants/antiplatelet agents were discontinued, according to the guidelines by the Cardiovascular and Interventional Radiological Society of Europe [16]. Intradiscal O2/O3 injections were performed with patients under conscious sedation with sterile technique. Patients were placed prone on the CT table (Canon Aquilion, Canon Medical Systems, USA) with a pillow under the belly to increase the lumbosacral angle. An external fiducial marker was positioned in the relevant area and a CT scan of the area of interest was obtained and used as a reference image for planning the needle path and to be matched with US for fusion imaging. DICOM dataset was then loaded onto an US machine equipped with a Global Positioning System (GPS)-based electromagnetic navigation unit, a sensor on the US transducer, and a needle-tracking system (MyLab X90, Esaote, Genova, Italy). The system provides an automatic match of CT images with US transducer and patient positioning with respect to the GPS sensor. Then, skin disinfection and sterile draping were done. Needle tracking was obtained with a single sensor (V-TRAX, Civco Medical Solutions, Coralville, USA), which was directly connected to the needle (15 cm length spinal needle, 22 G). The navigation system enables to monitor real-time the procedure by following a virtual needle that is displayed on either CT and US images. The needle was introduced through a paravertebral oblique postero-lateral in-plane approach to reach the center of the herniated disc (Fig. 1). Then, 20 mL O2/O3 was injected into the disc. The procedure was completed with periarticular injection of a mixture of local anesthetic (0.5 ml of mepivacaine 1%), steroid (0.3 ml of triamcinolone acetonide), and 10 ml of O2/O3 into each facet joint at L3-L4, L4-L5, and L5-S1 levels. Last, a CT scan was performed to evaluate the adequate O2/O3 intradiscal and paravertebral diffusion. All procedures were performed as outpatient, and all patients were advised to return to normal activities after 5 − 7 days, with specific instruction for avoiding bending, and weightlifting for 2 weeks. Pain medications and antibiotic therapy were not prescribed on discharge. Conventional percutaneous CT-guided injections were performed in the same way, but using CT as a guidance only (Fig. 2).
US/CT fusion imaging guided lumbar intradiscal O2-O3 injection. An external fiducial marker was positioned close to the relevant area (arrow, A). After disinfection, US probe was placed on the skin to merge images with CT scan (B, C) that has been already loaded onto the US machine equipped with a GPS-sensor (void arrows, B). Six needles were introduced into each facet joint at L3-L4, L4-L5, and L5-S1 levels, and one needle was introduced through a paravertebral oblique postero-lateral in-plane approach to reach the center of the herniated disc (D). The navigation system allowed real-time fusion of CT and US image with perfect superimposition of the posterior vertebral arch (E)
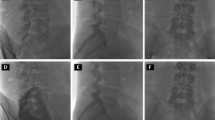
Conventional percutaneous CT-guided injection. The same procedure was done under CT guidance with the needles inserted into the facet joints and into the herniated disc (A–C). At the end of the procedure, a CT scan was performed to confirm the adequate O2/O3 intradiscal and paravertebral diffusion (D)
Data collection, sample size calculation, and statistical analysis
For each procedure, we collected the following data: (i) elapsed time from first CT scan and last injection (procedure operative time); (ii) room utilization time; (iii) number of CT passes; (iv) complications; (v) O2/O3 intradiscal diffusion adequacy. For what concerns the assessment of intervention duration, we could evaluate the elapsed time from first CT scan to last injection just looking at the time of acquisition of the first and last CT images. Regarding room utilization time, we routinely collect admission and discharge time of our patients from the interventional and CT units in our internal report.
Technical success was defined as the ability to complete the procedure as initially planned [17, 18] to reach the disc. Technical efficacy was based O2/O3 intradiscal diffusion adequacy, as demonstrated by the last CT scan. Differences in terms of demographics, disc levels, and procedure details were investigated between Fusion Group and Control Group.
Anonymous data were analyzed using MATLAB 2016b (The MathWorks, Natick, 2016). Differences among variables were evaluated by Fisher’s exact test for categorical variables, and by non-parametric Mann–Whitney U-test for continuous variables. A p value < 0.05 was considered to indicate statistical significance. Categorical variables were reported as absolute value and percentage; continuous variables were reported as either mean ± standard deviation or median and interquartile [25th–75th] range.
Results
Six patients (4 males, 2 females; mean age: 68 ± 15 years) were included in the Fusion Group and six patients (4 males, 2 females; mean age: 66 ± 12 years) were included in the Control Group. LDH involved the L3-L4 level (n = 1), L4-L5 level (n = 3), and L5-S1 level (n = 2) in the Fusion Group, the L3-L4 level (n = 1), L4-L5 level (n = 2), and L5-S1 level (n = 3) in Control Group. No significant differences in age (p = 0.749) and gender (p > 0.999) were found between the two groups. No complications were observed in both Groups. Room utilization time, procedure operative time, and number of CT passes were 30 ± 6 min, 14 ± 3 min, and 2 [2, 2] in the Fusion group, and 46 ± 10 min, 24 ± 6 min, and 3 [3, 3] in the Control group, respectively. Comparing the two groups, we observed significantly lower room utilization time (p = 0.008), procedure operative time (p = 0.008), and number of CT passes (p = 0.006) in the Fusion group. Patient characteristics and procedure details are resumed in Table 1. Technical success was 100% in both Groups, as the center of the herniated disc was reached with the tip of the needle in all patients. Technical efficacy was 100% in both Groups, as O2/O3 intradiscal diffusion was adequate in all cases as demonstrated by the last CT scan.
Discussion
Our main finding is that CT/US fusion imaging and virtual navigation system seems to be feasible and safe to guide lumbar intradiscal O2/O3 therapy, with 100% technical success and efficacy. CT/US fusion-imaging guidance ensured a decrease in procedure time and number of CT passes when compared to standard CT-guided interventions.
As abovementioned, the results of recent studies support the use of O2/O3 therapy for treating LBP and sciatica related to LDH [3]. When intradiscal is injected, imaging guidance must be used to reach the center of the herniated disc and to obtain better clinical improvements [4]. CT and fluoroscopy have been used for guiding this kind of intervention, but a non-negligible amount of ionizing radiations is administered to patients, which is particularly relevant when dealing with young adults. Unfortunately, the target of intradiscal injection cannot be seen directly through US. For this reason, CT/US fusion imaging could be helpful to overcome the limitations of the single imaging modalities used as guidance for interventions. As a matter of fact, CT images must be acquired repeatedly during a CT-guided intervention, with a subsequent increase of radiation exposure [19]. CT/US fusion imaging systems, match preoperative CT images with real-time US images, so that any structure detected on US can be immediately recognized on the corresponding structure on CT image without acquiring additional CT images. Hence, there is no need to stop the intervention to acquire CT images to monitor step-by-step the advancement of the needle that can be followed through fusion imaging guidance, thereby decreasing procedure time and making the intervention well-tolerated by the patient [20]. Last, this virtual navigation system makes spine interventional procedures safe [9]. These important points are all supported by our results. Indeed, we have reported a significant reduction of room utilization time and procedure operative time, that means an improvement of cost-effectiveness of these injections. In addition, the decrease of number of CT passes may help reducing radiation exposure of patients subjected to spine injections. In fact, during procedures guided by CT/US fusion imaging, we needed just pre-operative CT scan and post-operative CT images to confirm the correct placement of the needle, with a total of 2 CT passes for each procedure.
Similar results have been reported by a recent study that compared procedure duration time and clinical outcome of fluoroscopy guided vs CT guided intradiscal O2/O3 injections. Authors found decreased room utilization time and procedure operative time using fluoroscopy, with similar clinical success at 1-month, highlighting the importance of reducing time consumption [6]. No other studies have investigated the potential application of CT/US fusion imaging for guiding intradiscal injections. Nevertheless, in a similar setting, CT/US fusion has been shown to be helpful in decreasing radiation exposure and making shorter procedure duration time of spine bone biopsies [9]. Notably, during a bone biopsy, the needle must be placed exactly within the target lesion, paying attention particularly when dealing with small lesions. Hence, standalone fusion imaging cannot yet be employed without verifying needle position by CT before biopsy is performed. Conversely, during intradiscal O2/O3 injection, the operator clearly feels an increase of tissue resistance due to the needle transition when the needle penetrates the disc, with a completely different resistance compared to bon margins of vertebral bodies. Therefore, the correct placement of the needle can be easily perceived by the operator. Of note, in our study, three CT/US fusion imaging guided procedures were performed by a radiologist with 30 years of experience in intradiscal injections and three procedures were done by a radiologist without experience in intradiscal injections, but in all cases 100% technical success and efficacy were reached with two CT passes.
Some limitations of this study must be pointed out. First, the small sample size of our cohort that makes this series just a pilot study to understand the safety and feasibility of CT/US fusion imaging for guiding intradiscal injections. However, statistical significance was obtained for the two most important outcomes. Indeed, we think this is just a starting point for future studies aimed at confirming our results and investigating clinical impact and actual cost-effectiveness of this procedure. In this regard, it should be underlined that recommendations and guidelines have been published about image-guided musculoskeletal interventional procedures performed in the upper [21,22,23] and lower limb [24,25,26,27], but there is still a lack of standardization for what concerns the application of imaging as a guidance in the spine, despite several studies have been published on this topic [28, 29]. Last, we did not directly measure the reduction of radiation dose administered to the patients, but this is witnessed by the reduced number of CT passes that were done to complete fusion imaging guided injections. However, a reduction of the number of CT passes directly implies a reduction of radiation dose usage.
In conclusion, CT/US fusion imaging seems to be a feasible and safe guidance for intradiscal O2/O3 injections. US fusion with previously acquired CT images ensures real-time needle monitoring and correct needle placement into the herniated disc, allowing decrease of procedure time and number of CT passes needed to perform the injections, regardless operator’s experience. It may improve cost-effectiveness of intradiscal injections, which deserves further investigation by larger prospective studies.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Patrick N, Emanski E, Knaub MA (2014) Acute and chronic low back pain. Med Clin N Am 98(777–789):xii
Hoy D, March L, Brooks P et al (2014) The global burden of low back pain: estimates from the global burden of disease 2010 study. Ann Rheum Dis 73:968–974
Migliorini F, Maffulli N, Eschweiler J, Bestch M, Tingart M, Baroncini A (2020) Ozone injection therapy for intervertebral disc herniation. Br Med Bull 136:88–106. https://doi.org/10.1093/bmb/ldaa032
Rimeika G, Saba L, Arthimulam G et al (2021) Metanalysis on the effectiveness of low back pain treatment with oxygen-ozone mixture: Comparison between image-guided and non-image-guided injection techniques. Eur J Radiol Open 8:100389. https://doi.org/10.1016/j.ejro.2021.100389
Sconza C, Braghetto G, Respizzi S, Morenghi E, Kon E, Di Matteo B (2021) Ultrasound-guided periradicular oxygen-ozone injections as a treatment option for low back pain associated with sciatica. Int Orthop 45:1239–1246. https://doi.org/10.1007/s00264-021-04975-w
Somma F, Gatta G, Negro A et al (2022) Intradiscal ozone therapy: fluoroscopic guidance reduces operative time in comparison with CT guidance in patients with lumbar disc herniation. Radiol Med 127:526–533. https://doi.org/10.1007/s11547-022-01469-6
Simon C, Le Corroller T, Pauly V, Creze M, Champsaur P, Guenoun D (2022) Intradiscal oxygen-ozone therapy for the treatment of symptomatic lumbar disc herniation: a preliminary study. J Neuroradiol 49:180–186. https://doi.org/10.1016/j.neurad.2021.09.004
Morselli A, Zuccarini F, Scarpa I et al (2015) Ultrasound guidance in paravertebral injections of oxygen-ozone: treatment of low back pain. J Pain Relief 4:220
Mauri G, Gitto S, Pescatori LC, Albano D, Messina C, Sconfienza LM (2022) Technical feasibility of electromagnetic US/CT fusion imaging and virtual navigation in the guidance of spine biopsies. Ultraschall Med 43:387–392. https://doi.org/10.1055/a-1194-4225
Brock M, Roghmann F, Sonntag C et al (2014) Fusion of magnetic resonance imaging and real-time elastography to visualize prostate cancer: a prospective analysis using whole mount sections after radical prostatectomy. Ultraschall in Med 36:355–361
Prada F, Vitale V, Del Bene M et al (2017) Contrast-enhanced MR imaging versus contrast-enhanced US: a comparison in glioblastoma surgery by using intraoperative fusion imaging. Radiology 285:242–249
Calandri M, Ruggeri V, Carucci P (2019) Thermal ablation with fusion imaging guidance of hepatocellular carcinoma without conspicuity on conventional or contrast-enhanced US: surrounding anatomical landmarks matter. Radiol Med 124:1043–1048. https://doi.org/10.1007/s11547-019-01057-1
Klauser AS, De Zordo T, Feuchtner GM et al (2010) Fusion of real-time US with CT images to guide sacroiliac joint injection in vitro and in vivo. Radiology 256:547–553
Sartoris R, Orlandi D, Corazza A et al (2017) In vivo feasibility of real-time MR–US fusion imaging lumbar facet joint injections. J Ultrasound 20:23–31
Giurazza F, Guarnieri G, Murphy KJ, Muto M (2017) Intradiscal O2O3: rationale, injection technique, short- and long-term outcomes for the treatment of low back pain due to disc herniation. Can Assoc Radiol J 68:171–177. https://doi.org/10.1016/j.carj.2016.12.007
PatelI J, Davidson JC, Nikolic B et al (2012) Consensus guidelines for periprocedural management of coagulation status and hemostasis risk in percutaneous image-guided interventions. J Vasc Interv Radiol 23:727–736
Sconfienza LM, Albano D, Messina C et al (2020) Ultrasound-guided percutaneous tenotomy of the long head of biceps tendon in patients with symptomatic complete rotator cuff tear: in vivo non-controlled prospective study. J Clin Med 9:2114. https://doi.org/10.3390/jcm9072114
Albano D, Messina C, Gitto S, Chianca V, Sconfienza LM (2023) Bone biopsies guided by augmented reality: a pilot study. Eur Radiol Exp 7:40. https://doi.org/10.1186/s41747-023-00353-w
Hoang JK, Yoshizumi TT, Toncheva G et al (2011) Radiation dose exposure for lumbar spine epidural steroid injections: a comparison of conventional fluoroscopy data and CT fluoroscopy techniques. Am J Roentgenol 197:778–782
Martins PH, Costa FM, Lopes FPPL et al (2018) Advanced MR imaging and ultrasound fusion in musculoskeletal procedures. Magn Reson Imaging Clin N Am 26:571–579
Sconfienza LM, Adriaensen M, Albano D et al (2020) Clinical indications for image guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)—part III, nerves of the upper limb. Eur Radiol 30:1498–1506. https://doi.org/10.1007/s00330-019-06479-z
Sconfienza LM, Adriaensen M, Albano D et al (2020) Clinical indications for image-guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)—part II, elbow and wrist. Eur Radiol 30:2220–2230. https://doi.org/10.1007/s00330-019-06545-6
Sconfienza LM, Adriaensen M, Albano D et al (2020) Clinical indications for image-guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)-part I, shoulder. Eur Radiol 30:903–913. https://doi.org/10.1007/s00330-019-06419-x
Sconfienza LM, Adriaensen M, Albano D et al (2022) Clinical indications for image-guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)-part VI, foot and ankle. Eur Radiol 32:1384–1394. https://doi.org/10.1007/S00330-021-08125-Z
Sconfienza LM, Adriaensen M, Alcala-Galiano A et al (2022) Clinical indications for image-guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)-part IV, hip. Eur Radiol 32:551–560. https://doi.org/10.1007/S00330-021-07997-5
Sconfienza LM, Adriaensen M, Albano D et al (2022) Clinical indications for image-guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)-part VII, nerves of the lower limb. Eur Radiol 32:1456–1464. https://doi.org/10.1007/S00330-021-08283-0
Sconfienza LM, Adriaensen M, Albano D et al (2022) Clinical indications for image-guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)—part V, knee. Eur Radiol 32:1438–1447. https://doi.org/10.1007/s00330-021-08258-1
Wu TJ, Hung CY, Lee CW, Lam S, Clark TB, Chang KV (2020) Ultrasound-guided lumbar intradiscal injection for discogenic pain: technical innovation and presentation of two cases. J Pain Res 13:1103–1107. https://doi.org/10.2147/JPR.S253047
Chang KV, Kara M, Su DC et al (2019) Sonoanatomy of the spine: a comprehensive scanning protocol from cervical to sacral region. Med Ultrason 21:474–482. https://doi.org/10.11152/mu-2034
Funding
Open access funding provided by Università degli Studi di Milano within the CRUI-CARE Agreement. The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Interventional procedures were performed by DA and AB. Material preparation, data collection and analysis were performed by CM, SG and SF. The first draft of the manuscript was written by DA and CM. The draft was reviewed by LMS and AB. All authors commented on previous versions of the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
Institutional Review Board approval was obtained for this retrospective study.
Consent to participate
Written informed consent was waived by our Ethical Committee.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of the images.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Albano, D., Messina, C., Gitto, S. et al. US/CT fusion imaging and virtual navigation to guide lumbar intradiscal oxygen-ozone therapy: a pilot study. J Ultrasound (2023). https://doi.org/10.1007/s40477-023-00835-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40477-023-00835-y