Abstract
Purpose of the Review
Despite the global mortality reduction in the last two decades, diarrhea remains the second major cause of mortality in children less than 5 years of age, particularly in countries like Mozambique. This article aims to review the available data on the burden and etiology of diarrhea in Mozambique.
Recent Findings
Epidemiological studies defining the burden and etiology of diarrhea (mostly from Southern Mozambique) have demonstrated a high disease burden and an associated case fatality rate of nearly 10%. Rotavirus, Shigella spp., enterotoxigenic, and enteroaggregative Escherichia coli, Vibrio cholerae, and Cryptosporidium spp. have been reported to be associated with infantile diarrhea. Rotavirus vaccine has greatly impacted in the reduction of diarrheal hospitalization cases across the country.
Summary
Understanding the local epidemiology of diarrhea across the country is critical for defining and prioritizing other enteric vaccines or interventions that can contribute to accelerate the reduction of morbi-mortality of infantile diarrhea in Mozambique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite that diarrheal mortality has been declined over the last two and half decades (1990–2015), with tremendous reduction of nearly 40% between 2008 and 2010 [1, 2], the associated deaths remain unacceptably high (https://www.unicef.org/lac/20161111_UNICEF-one-is-too-many-report.pdf). In 2015, diarrheal disease was ranked as the second cause of childhood mortality, accounting for 8.6% of 5.9 million deaths among children under 5 years old globally [3]; and 88% of all deaths occurred in sub-Saharan Africa and South Asia [3].
Nevertheless, efforts have been made, particularly in sub-Saharan Africa to prevent childhood deaths as witnessed by decrease in the number of under five deaths from 549.092 in 2000 to 310.967 in 2013 [4]. Several factors may have played a role in the reduction of diarrheal morbidity and mortality, such as improvement of sanitation, access of clean water, increased supply of oral rehydration salts solutions (ORS), and the introduction of vaccine against rotavirus recommended by the World Health Organization in 2006 [4,5,6].
In Mozambique, estimates from verbal autopsy study showed that diarrhea is responsible for approximately 20% of hospital admissions, being the fourth cause of mortality preceded by malaria, HIV, and pneumonia respectively in a rural community of Manhiça [7]. In addition, reports have shown decline of diarrheal-related deaths from more than 13,105 annually in 2010 to almost half (7340) in 2015 among children under 5 years old affecting particularly children under 2 years of age [1, 8, 9]. One of the limitation of the aforementioned report was unable to assess the contribution of specific pathogen on diarrhea morbidity and associated mortality. In this review, we aim to compile available data on diarrhea from the last two decades in Mozambique, from various perspectives: analyses of the etiology, prevalence by provinces, and different interventions implemented in the country.
Methodology Notes
Our review summarizes the most relevant and recent literature of pediatric diarrhea in Mozambique following a search of PubMed, and review of available data from other sources such as demographic surveys (DHS), Multiple Indicator Cluster Survey (MICS) Health Information System for Monitoring and Evaluation SIS-MA and the personal perspectives of contributing experts. We searched PubMed, with the keywords “etiology of diarrhea; viral, parasitic and bacterial diarrhea in Mozambique” as our primary search term, to identify studies published between January 1997 and December 2017. We also used the combination of specific pathogens (e.g., Rotavirus, Shigella, Salmonella, Escherichia coli, etc. in Mozambique) to expand our search.
Studies Investigating Diarrheal Disease
Studies investigating etiology of diarrhea are few in Mozambique, particularly those from outside of southern Mozambique, and among them, only some have addressed a broad range of pathogens, as the majority have focused on specific pathogens. Then, this resume will contribute to fill the existing gaps on the lack of countrywide data on pediatric diarrhea and may be critical for appropriate planning of future studies. Because this is the first literature review on pediatric diarrhea, along with limited availability of data, we aimed to review and summarize the existing epidemiological and administrative data on the burden, etiology, and prevention of diarrheal disease in Mozambique during the last two decades (1997–2017).
Burden of Diarrheal Disease in Mozambique
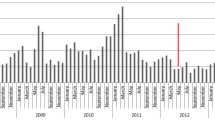
In Mozambique, administrative data on infectious disease, mainly for communicable diseases (which also include diarrheal disease) is routinely collected throughout the country based on weekly epidemiological bulletin (Boletim Epidemiológico Semanal (BES)). BES consists in recording and reporting all communicable disease seen at the health facilities, and data is transmitted from the health facility to district, provincial, and national level. So far, this is the only countrywide available data that often used to estimate the overtime trends of the specific diseases and can be used to indirectly assess the impact of interventions (e.g., rotavirus vaccine introduction). On the other hand, the national demographic health surveys aimed to estimate the main health problems including the major diseases contributing to morbi-mortality burden are relevant source of diarrheal disease data as discussed below.
Surveys Estimating the Burden of Diarrheal Disease
Between 1997 and 2011, four surveys (demographic health surveys (DHS) and Multiple Indicator Cluster Survey (MICS)) were conducted across the country [9,10,11,12] and provided a snapshot on the incidence of community-reported diarrhea, suggesting that the national prevalence of diarrhea has been declining over the time (21% in 1997, 14% in 2003, 18% in 2008, and 11% in 2011). Despite that, the survey from 1997 was conducted among children less than 3 years of age, while the others included children up to 5 years; all consistently showed high incidence of diarrhea among children aged 6 to 23 months old [9,10,11,12].
Because the hygiene and sanitation vary according to the provinces, these surveys were somehow useful to assess the local level of progress (indirectly measured as a trend of diarrhea incidence) of the implementation of the strategies to prevent diarrhea. Therefore, there was a substantial reduction (to less than 10%) on diarrhea’s prevalence for Cabo Delgado, Inhambane, Manica, and Maputo City, in contrast to Zambézia, Tete, Sofala, and Gaza that remained above 10% between 1997 and 2011 as shown in Table 1 [9,10,11,12].
This data may have important implications to define local specific interventions to reduce the burden of diarrheal disease, despite the limitation of these surveys that were unable to assess the contribution of specific pathogen on disease burden due to the lack of stool samples for microbiological investigations.
Epidemiological Studies Defining Burden and Etiology of Diarrhea
The infectious diarrhea is caused by a wide range of pathogens, such as bacteria, parasites, and viruses; however, only a small number of pathogens have been found to be associated with diarrhea [13,14,15,16]. In Mozambique, etiological data and its association with diarrhea are critical for defining and planning appropriate strategies for diarrheal prevention and/or control, and the relevant pathogens are summarized below.
Viral Etiology
Among viral pathogens, rotavirus remains the leading cause of severe diarrhea, particularly in children less than 2 years of age, globally [17]. In Mozambique, Early’s (2005) study [18] from urban area of Maputo City documented rotavirus among the leading pathogen associated with mild diarrhea in children less than 5 years accounting for 18.2% in symptomatic and 5% in asymptomatic children [18]. Similarly, the recently ended Global Enteric Multicenter Study (GEMS) case-control [19] highlighted rotavirus as the leading pathogen associated with moderate-to-severe diarrhea, particularly in Mozambican infants from rural Manhiça District with attributable fraction of 34.75% (95% CI 31.30–38.20) [20••], in contrast to early study by Mandomando [21] that was unable to detect rotavirus. Furthermore, Acácio et al. (Manuscript submitted to Vaccine) reported that the rotavirus incidence rate is even higher in infants with less severe diarrhea (24.7 cases per 100 children-years; 95% CI 915.02–34.35) compared to those with moderate to severe diarrhea (3.07 cases/100 children-years; 95% CI 2.49–3.66).
Data from additional studies (despite did that did not enroll controls) corroborated with the general finding of rotavirus being the most frequently pathogen detected accounting for 24% of hospitalized under five children with diarrhea (with 97% of the positive cases detected in children younger than 2 years of age) in the Chokwé District, Gaza Province [22•], and 42.4% (1.7-fold positivity rate higher than Chokwé) in the Maputo Province [23]. In the latter, rotavirus was found to be slightly more prevalent in urban area (44.3% in the Mavalane General Hospital) compared to 41.3% in rural area of Manhiça District, with high frequency among children aged 6–23 months [23]. Nevertheless, the single study conducted in the three regions of the country (North—Nampula Central Hospital, Nampula; Central—Beira Central Hospital, Sofala and Quelimane General Hospital, Zambezia; and South—Mavalene General Hospital and Maputo Central Hospital, Maputo) [24••] demonstrated a clear reduction of rotavirus-associated diarrhea from 40.2 and 38.3% in 2014 and 2015, respectively, to 12.2 and 13.5% in 2016 and 2017, respectively [24••], supporting the benefit effect of rotavirus vaccine adoption in September 2015.
Adenovirus 40/41 and Other Enterovirus
The available data with regard to other enterovirus are from the GEMS, where Adenovirus 40/41, Norovirus I/II, Astrovirus, and Sapovirus were detected in similar proportion between cases and controls ranging from 0 to 5% [20••]. From the aforementioned viral pathogens, only Adenovirus 40/41 was associated with diarrhea with attributable fraction of 2.73 (95% CI 2.33–3.13) among children aged 12–23 months [20••]. In addition, recently, Bero et al. [25] reported for the first time the occurrence of human enterovirus (HEV) in children with and without diarrhea in Maputo in approximately 1.5% of enrolled children [25].
Intestinal Parasites
Intestinal parasites (helminths and protozoa) are an important cause of morbidity and mortality in developing countries. Parasites are very common in the countries with deficiency in water supply, and poor hygiene and sanitation which prone their transmission through contaminated water or food [26]. Comprehensive data on the contribution of parasitic agents was assessed within the GEMS study, providing a snapshot of the relevant pathogens. Interestingly was the unexpected finding of protozoa Cryptosporidium spp. as the second leading pathogens, only after rotavirus associated with diarrhea in infants [20••]. The burden of Cryptosporidium reported in this study is a matter of concern as approximately 15.3% (95% CI 11.96–18.56) of diarrhea in this age group can be attributable to this pathogen yielding an incidence rate of 1.56 (95% CI 1.15–1.97) cases per 100 child-years-at-risk [20••], as currently, there is no effective licensed drug for cryptosporidiosis treatment.
Furthermore, the inverse association of Giardia lamblia with diarrhea suggests that Giardia may play protective role against moderate-to-severe diarrhea [14]; raising important questions on the implication for the physicians’ clinical practices on the management of patient of who Giardia is detected in stool. Therefore, the clinical significance and interpretation of the detection in another studies in the country (varying from 2.5 to 16.1%) [21, 27] may be done with caution.
The GEMS study failed to establish the association between etiological agents of amoebic dysentery (Entamoeba histolytica), as it was detected in the range of 9 to 12% [20••]. The rate of E. histolytica detection was similar between the rural community of Manhiça [20••] and urban areas (6–11%) [27, 28].
Lastly and not least, data from the National Surveillance of Acute Diarrhea in children less than 5 years of age in Mozambique (2013–2015) showed that Ascaris lumbricoides (18%) and Trichuris trichuria (12%) are among the most frequent soil transmitted helminths [28], while T. trichuria and A. lumbricoides were less common accounting with 6.5 and 2.2%, respectively, in the study by Fonseca [27].
Bacterial Diarrhea
Bacterial diarrhea pathogens, particularly diarrheagenic E. coli pathotypes, Shigella spp., Salmonella enterica, Vibrio cholerae, Aeromonas spp., and Campylobacter jejuni/coli, are among the major etiological agents of endemic diarrhea in developing countries.
E. coli are versatile pathogens as are part of animals and human flora. The pathogenic strains are common causes of bacterial infections associated with high morbidity and mortality, particularly in developing countries [29, 30]. Two major groups of pathogenic E. coli—diarrhoeagenic E. coli (DECs) and extra-intestinal pathogenic E. coli (ExPEC)—are recognized, differing in their virulence factors and associated clinical syndromes [31]. There are at least seven pathotypes of DECs (with six well recognized), enteropathogenic (EPEC), enterotoxigenic (ETEC), enterohaemorrhagic (EHEC), enteroinvasive (EIEC), and the most recently identified enteroaggregative E. coli (EAEC), diffusely adhering E. coli (DAEC) and cytolethal distending toxin (CDT)-producing E. coli [32]. Of these, EPEC, ETEC, EIEC, EHEC, and EAEC are clearly associated with different clinical types of enteritis, while the other pathotypes are candidates as potential pathogens, but their association with diarrhea has not been clearly assessed, and further studies are required to confirm their etiological role in enteric diseases [31].
The early study that investigated DECs in Mozambican children focused on mild diarrhea in Maputo City combining both molecular and cytological approaches, and showed that 59.2% (298/503) of E. coli isolated from stools had a potentially pathogenic phenotype or genotype, of which 229 (41.8%) came from symptomatic and 69 (18.1%) from asymptomatic children, p < 0.0001 [18]. Molecular analysis showed that ETEC (2.8 vs. 0.8%, p = 0.0499), EAEC (9.5 vs. 4.5%, p = 0.0067), DAEC (22.8 vs. 11.0%, p < 0.0001), and cytotoxic E. coli (4.2 vs. 1.1%, p = 0.0048) were significantly found among symptomatic than asymptomatic children. In this study [18], EIEC was uncommon (0.3%) and no EHEC strains were recovered [14], and to date, this is the only study that found the association of EAEC (4.7% among cases vs. 1.6% among controls, p = 0.0098) and DAEC (10.8% in cases and 6.3% in controls, p = 0.0195) with diarrhea [18].
In contrast to the findings from other studies [15, 18, 20••, 21], Sumbana et al. [33] found EIEC pathotype as the most frequent (21%) of the 80 E. coli isolated from children with diarrhea in Maputo City, followed by EPEC (19%), EAEC (15%), and DAEC (5%). The GEMS failed to identify the association of EAEC with moderate-to-severe diarrhea, while Shigella spp., Vibrio cholerae, and ST producing ETEC were so [14, 20••]. The differences in the role of EAEC between the two case-controls studies may be explained by the severity of diarrhea and the geographic location, as the study by Rappeli was conducted in children living in urban area with mild diarrhea, while the GEMS focused on moderate-to-severe diarrhea from rural area [18, 20••].
Although pediatric morbidity from shigellosis remains substantial, mortality has diminished, in part, due to the virtual worldwide disappearance of the highly virulent Shiga toxin-producing Shigella dysenteriae serotype 1 and because the World Health Organization guidelines recommend antibiotic treatment for clinical dysentery (diarrhea with gross blood) [34]. Data on shigellosis are very scarce in Mozambique, and a part of the early report of outbreak of dysentery that affected the country in 1993, with a total of 47,483 cases and 199 deaths, was reported, yielding an incidence rate of 292.5/100,000 and a fatality rate of 0.25% for the whole country [35]; to our knowledge, only two studies have investigated the role of shigellosis in endemic pediatric diarrhea [14, 36]. Shigellosis was found to be responsible of approximately 25% of bloody diarrhea among children aged < 5 years attending the outpatient department with minimal community incidence rate as high as 488.4/100,000 child-years-at-risk [36]. Furthermore, the role of shigellosis for pediatric diarrhea has been confirmed in the GEMS providing supporting data for the need of vaccine for prevention of this disease, where Shigella was among the top five attributable fraction of childhood diarrhea in the seven countries [14]. In addition, epidemiological data on shigellosis have provided a snapshot on serotypes circulating to guide vaccine development with broader coverage with the predominant serotypes circulating in Mozambique [34, 37] which include S. flexineri 2a (38%), S. flexineri 6 (18.9%), and S. flexineri 1b (10.8%) [34].
Salmonella enterica particularly non-typhoidal Salmonella have been for long implicated in self-limited gastroenteritis, and extra-intestinal infections including bacteremia which may occur, particularly in infants less than 3 months of age [38, 39]. However, in the last years, in sub-Saharan Africa including Mozambique, gastroenteritis associated with Salmonella are uncommon [20••, 21] and multidrug-resistant strains Salmonella ST313 have emerged as cause of invasive disease with high case fatality rate [40], including the occurrence of Salmonella Typhimurium DT104 [41]. In contrast to Salmonella gastroenteritis, the incidence rate of invasive non-typhoidal Salmonella (nearly 220 cases/100,000 child-years-at-risk) [40], particularly Salmonella Typhimurium, is similar to those reported for Streptococcus pneumoniae in Manhiça community [42]. Salmonella isolation in stool has been less than 2.5% [21], and no statistical differences were found between cases and controls in children living in rural community of Manhiça [20••].
Campylobacter jejuni/coli have been always ranked among the major diarrheal bacterial pathogens; however, in Mozambique, its prevalence ranges from 1.7 to 6% with no statistical difference between cases and control [20••, 21] when assessed by conventional microbiological techniques [43]. The lower frequency of Campylobacter spp. found in these studies is consistent with that from other African studies in which these microorganisms have been isolated in around 3 and 8% [44], and this lower frequency may be partially explained by the difficulties to culture this pathogen.
Cholera is endemic in sub-Saharan Africa and causes substantial outbreaks in many countries including Mozambique that has experienced endemic and epidemic cholera for decades. During 2000–2009, suspected cholera cases reported annually to the WHO varied from a low of 2226 during 2005 to a high of 24,375 during 2002 associated with case fatality rates ranging from 0.46 to 1.4% during 2000–2009 [45]. The national annual cholera incidence varied from 12.0–126.5 per 100,000 populations during 2000–2009, while data from national surveillance (2009–2011) showed an average of annual incidence of 55 per 100,000 population between 2009 and 2011 [45]. In this period, the provinces mostly affected were Zambezia (n = 6806), Cabo Delgado (n = 5473), Gaza (n = 128), and Inhambane (n = 37), and the national case fatality rate was 0.87% (220 deaths among the 25,431) [45].
Despite that cholera has been devastating Mozambique, particularly in Central and Northern regions, there was a decrease in the number of cases reported in the last years. Data from Africhol program (October 2011 to December 2015) aimed to enhance surveillance zones located in the provinces of Sofala (Beira), Zambézia (District Mocuba), and Cabo Delgado (Pemba City), and showed that three outbreaks during the study period occurred with the districts of Cuamba, Montepuez, and Nampula being mostly affected [46]. During the study period, a total of 1863 suspected cases (87.1% reported during the rainy season) with a case fatality ratio of 1.2% were reported, with 52.2% of the cases tested yielding a positivity rate of 23.5% for Vibrio cholerae O1 Ogawa, reinforcing the importance of continued cholera surveillance, including a strong laboratory component [46]. In addition, children less than 5 years of age were less affected (26/216, 12%), compared to other age groups with > 21% of confirmed cases [46].
Similarly, to Africhol and National Surveillance, the GEMS found that endemic V. cholerae Ogawa O1 is an important pathogen for childhood diarrhea with attributable fraction of 8.3 (95% CI 2.8–13.9) among children aged 24–59 months admitted at the hospital with moderate-to-severe diarrhea [14].
Even though that the number of cholera outbreaks has been diminishing over the years, new outbreak was reported in Nampula with 12 confirmed cases [47]. Another outbreak was reported between August of 2017 and February of 2018 with 1.799 reported cases and 1 death in northern of Mozambique (Nampula and Cabo Delgado) [48]. These outbreaks of cholera show the need to intensify actions of hygiene, sanitation, and health education and determining associated factors of the outbreaks in each of the provinces. In order to reduce case fatalities related to cholera, the government introduced cholera vaccine in Nampula in 2016 as priority considering the background of the province, and more than 425.486 doses of vaccine were sent to Nampula to implement the campaign [49].
The Role of Molecular Techniques in Disease Burden Estimation
The determination of the microbiologic etiology of enteric infection remains an important challenge, in part due to limitations of conventional approaches, including culture, microscopy, and antigen-based detection. Therefore, molecular diagnostics, especially PCR-based tests, are rapidly changing research and practice in infectious diseases and with high sensitive, may result in the detection of low levels of enteropathogens which could contribute to define the true disease burden and pathogen specific. Indeed, the reanalysis of the GEMS study [14] using a quantitative PCR [50••] showed that overall, pathogen-attributable diarrheal burden was higher as 89.3% (95% CI 83.2–96.0) at the population level, compared with 51.5% (48.0–55.0) in the original GEMS analysis. The incidence for most pathogens was greater with qPCR than with the original methods, particularly for adenovirus 40/41 (around five times), Shigella spp. or enteroinvasive E. coli (EIEC) and Campylobactor jejuni/coli (around two times), and ST producing ETEC (around 1.5 times). The six most attributable pathogens became, in descending order, Shigella spp., rotavirus, adenovirus 40/41, ST-ETEC, Cryptosporidium spp., and Campylobacter spp. [50••]. Reanalysis of the GEMS data from Mozambique showed that pathogens like with attributable fraction (AF) of 11.2 (95% CI 3.0–20.0) and Adenovirus 40/41 (AF = 13.3, 95% CI 11.3–24.1) in infants; typical enteropathogenic E. coli (AF = 3.4, 95% CI 1.5–10.5), Adenovirus 40/41 (FA = 11.3, 95% CI 4.8–23.4), and Norovirus GII (AF = 3.8, 95% CI 1.7–9.2) in children 12–23 months; and Aeromonas (AF = 5.6; 95% CI 1.1–12.5) in older children were among the pathogens that significantly increased the detection rate and contribution in moderate-to-severe diarrhea by qPCR [50••]. These results highlight the importance of the qPCR on diarrheal disease burden assessment and also that this technique can be adopted in the research institution in Africa as platform for investigation etiology of diarrhea in these settings (often with a lack of well-trained staff challenging the accurate diagnosis). Despite that TaqMan Array Card is an expensive technology, it may be cost-effective taking into account the cost of individual pathogen detection cost associated with unaffordable prices of molecular biology reagents (three to four times higher than Europe or USA) applied by local vendors, in addition to the limited number of qualified technicians.
Antimicrobial Resistance Among Bacterial Pathogens Implicated on Diarrhea
The management of diarrhea disease is based on reposition of fluid, and antibiotics are recommended for specific cases to shorten the period of bacterial excretion and transmission such as shigellosis or cholera. However, the prevalence of antimicrobial resistance is a growing concern. For example, among Salmonella isolates, multidrug resistance (resistance to ampicillin, chloramphenicol, and trimethoprim-sulfamethoxazole) has become common in Mozambique [41, 51,53,53]. Similarly, growing concern on antimicrobial resistance is also observed among Shigella isolates where resistance rates ranged from 50.7% (34/67) for ampicillin to 92.5% (62/67) for trimethoprim/sulfametoxazole, with multidrug resistance being present in 55.2% (37/67) of the isolates and associated case fatality rate of 8.1% (3/37) [37]. On the other hand, Vibrio cholerae strains have been susceptible to the recommended antibiotics (e.g., tetracycline) [54]; however, in the last years, there was a continuous growing of antimicrobial resistance from 25% in 2012 to 100% in 2015 of tested strains to tetracycline [55]. This resistance are alarming as the drug of choice (doxycycline) was also found not efficacious in 100% of tested strains in 2015 [55], limiting therapeutic options in the countries with limited access of second-line treatment as Mozambique. In addition, the presence of resistance markers associated to cholera resistance including genetic diversity of strains [56,58,59,59] strongly reinforces the need to strengthen the laboratory capacities for prompt diagnostic confirmatory of cholera across country to support continuous surveillance of antimicrobial resistance and emergence of new strains. Lastly, not least, the widespread emergence of extended spectrum of Bata-lactamases (ESBL) among E. coli strains including diarrheagenic ones has been pressing substantially among sub-Saharan Africa including Mozambique where highly resistant E. coli causing urinary tract infection were reported in 89.7% (26/29) in Beira [60]. Indeed, ESBL producing E. coli were found in 11% (17/151) of E. coli isolates causing bacteremia and UTI in the Manhiça community with CTX-M-15 being the most frequently detected ESBL, accounting for a 75% of the total isolates characterized associated with the presence of two plasmid [Guiral et al. in press Infect Drug Resist].
Collectively, available data on antimicrobial resistance in Mozambique highlight the critical challenges for management of patients presenting with severe diarrhea which requires appropriate supportive care, and correct antimicrobial therapy when recommended to prevent poor outcome as reported elsewhere [37]. This suggests the urgent need to understand the local factors that govern the antimicrobial resistance increase as well as the need of new and effective antimicrobial agents.
Diarrhea, HIV, and Malnutrition
Mozambique is one of the African countries with high prevalence of malnutrition in children. It is estimated that approximately 40% of the children in the country suffer from one type of malnutrition [9]. On the other hand, in 2015, the national prevalence of HIV was 13.2% [61] and in 2014, the number of children (0–14) years old living with HIV was estimated in 183.631 [62].
Malnutrition and HIV are two very important factors of diarrhea diseases both reported in some studies conducted in children from Mozambique. Nhampossa et al. [63] conducted a 10-year analysis of hospital admission of children in the area of Manhiça, reporting that 47% of the 274.813 children attended were admitted with some degree of malnutrition (of which 6% was severe malnutrition). Acute diarrhea was one of the risk factors for mortality in children with severe malnutrition [63].
On the other hand, co-infection HIV and diarrhea is common in high HIV prevalence settings, with reports showing a frequency of 17.7% of HIV infection and 43.7% of under nutrition among children with acute diarrhea [23]. In addition, a high proportion of children malnourished infected with rotavirus was observed by de Deus and co-authors in Maputo and Manhiça [23]. Furthermore, in GEMS study, a sub-study addressing the role of HIV infection on the etiology and severity of diarrhea showed that approximately 23% of children attending the health facilities with moderate to severe diarrhea were co-infected with HIV compared to 6% for the matched controls, and HIV was found as contributor of excess mortality and shaped the etiology of diarrhea [Acacio manuscript submitted to Internat. J Infect Dis]. These data show the importance of understanding the relation or the influence of HIV infection and malnutrition in children with diarrhea. This is particularly important to understand the low efficacy of rotavirus vaccine in African countries, where malnutrition has been shown to be associated with this low effectiveness in this region [64].
Interventions That May Have Contributed to Prevent/Control Diarrhea Disease in the Country
Interestingly, the trend of diarrhea hospitalization has been declined over the years even prior to rotavirus vaccine introduction, which clearly accelerated this trend countrywide. The national reduction of diarrhea in the country can be explained by different policies implemented in the country such as the increase access of safe water, and improvement of sanitation and hygiene (WASH). According to National Directorate of Water and Minister of Public Work, between 1990 and 2008, the number of people with supply of clean water in rural areas increased from 30 to 52 and 35 to 50% in urban areas [65]. The number of people with good sanitary condition increased from 16 to 40% in rural areas and 15 to 55% in urban areas from 1990 to 2008 [65]. In spite of the increase in sanitation, two out of five people living in rural areas are still practicing open defecation [65].
The DHS surveys also collect data on the health seek behavior from the mothers and caretaker of the children. With regard to the mothers’ knowledge about ORS use in children with diarrhea, there was substantial increase of the knowledge among the respondents, from 87.0% in 2003 to 91% in 2011 [9, 11]. Fifty-six percent of the children with diarrhea were taken to the hospital and received SRO and zinc oxide [61].
The frequency of children with diarrhea, who received hydration therapy, increased from 49% in 2003 to 62% in 2011, showing the effectiveness of the campaigns and sensitization of the population in the care they should have about diarrhea [9, 11].
Other important intervention which may have contributed for this reduction was the implementation of the campaign called the “national health week” which is held twice a year since 2008, where children are vaccinated, dewormed, and supplemented with vitamins A and iodine [62]. The lack of surveys between 2012 and 2018 does not allow to evaluate the time trend of this actions from the last 6 years.
Annual statistics data of hospitalization due to diarrhea in Mozambique showed also a reduction of cases of diarrhea in the last 6 years. These data showed that 447.215 children under 4 years of age in 2012 were admitted with diarrhea that dropped to 333,932 admissions in 2017 [66].
Mozambican government implemented other important interventions to reduce the burden of diarrhea in the country. In September 2015, Rotavirus monovalent vaccine (Rotarix; GlaxoSmithKline Biologicals) was introduced in the National Immunization Program. de Deus et al. [24••] observed a reduction of rotavirus infection from 40 to 12%, after vaccine introduction in the country. Despite this reduction, there is a need to study the 12% of children positive to rotavirus. Additional studies will be necessary to investigate the effectiveness of rotavirus vaccine in the country and factors contributing to the occurrence of rotavirus infection in vaccinated children. Finally, it is important to understand the role of malnutrition and HIV on vaccine effectiveness in the country.
Conclusions
Despite that epidemiological data remain scarce in Mozambique, several actions were implemented in the country (including the vaccination against rotavirus as the leading attributable pathogens of severe diarrhea in children younger than 2 years) and contributed in the reduction of diarrheal burden in Mozambique in the last two decades. However, there are still gaps in assessing the contribution of specific pathogen on diarrhea burden and associated risk factors, particularly outside of Maputo Province, supporting the need of continuous diarrheal surveillance countrywide to inform decision making for appropriate interventions targeting pathogen specific and understand the co-morbidity factors (e.g., malnutrition, HIV) of diarrhea, including strategies to contain antimicrobial resistance trends among bacterial pathogens.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375:1969–87.
Liu L, Oza S, Hogan D, Perin J, Rudan I, Lawn JE, et al. Global, regional, and national causes of child mortality in 2000-13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet. 2015;385:430–40.
Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, et al. Global, regional, and national causes of under-5 mortality in 2000-15: an updated systematic analysis with implications for the sustainable development goals. Lancet. 2016;388:3027–35.
Tate JE, Burton AH, Boschi-Pinto C, Parashar UD. World Health Organization–Coordinated Global Rotavirus Surveillance Network. Global, regional, and national estimates of rotavirus mortality in children <5 years of age, 2000-2013. Clin Infect Dis. 2016;62(Suppl 2):S96–105.
https://www.unicef.org/supply/files/ORS_and_Zinc_Supply_Update.pdf. UNICEF. Oral rehydrations salts and zinc suppliers and product range UNICEF Supply Division 2014. 2014.
Rotavirus vaccines WHO position paper: January 2013 - Recommendations. Vaccine. 2013;31:6170–1.
Inquéritos — Instituto Nacional de Estatistica [Internet]. [cited 2018 Mar 13]. Available from: http://www.ine.gov.mz/operacoes-estatisticas/inqueritos/inquerito-sobre-causa-de-mortalidade/inquerito-nacional-sobre-causa-de-mortalidade-2007-8-pdf/view.
Inquérito sobre Causas de Mortalidade (INCAM) — Instituto Nacional de Estatistica [Internet]. [cited 2018 Apr 9]. Available from: http://www.ine.gov.mz/operacoes-estatisticas/inqueritos/inquerito-sobre-causas-de-mortalidade.
IDS. Moçambique Inquérito Demográfico e de Saúde 2011. Calverton, Maryland, USA: MISAU, INE e ICFI. 2011;412.
IDS 1997.pdf — Instituto Nacional de Estatistica [Internet]. [cited 2018 Mar 13]. Available from: http://www.ine.gov.mz/operacoes-estatisticas/inqueritos/inquerito-demografico-e-de-saude/ids-1997.pdf/view.
IDS 2003.pdf — Instituto Nacional de Estatistica [Internet]. [cited 2018 Mar 13]. Available from: http://www.ine.gov.mz/operacoes-estatisticas/inqueritos/inquerito-demografico-e-de-saude/ids-2003.pdf/view.
https://mics-surveys-prod.s3.amazonaws.com/MICS3/.../2008/.../Mozambique%202008... MICS. Inquérito de Indicadores Múltiplos. 2008.
Breurec S, Vanel N, Bata P, Chartier L, Farra A, Favennec L, et al. Etiology and epidemiology of diarrhea in hospitalized children from low income country: a matched case-control study in Central African Republic. PLoS Negl Trop Dis. 2016;10:e0004283.
Kotloff KL, Nataro JP, Blackwelder WC, Nasrin D, Farag TH, Panchalingam S, et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the global enteric multicenter study, GEMS): a prospective, case-control study. Lancet. 2013;382:209–22.
Nataro JP, Mai V, Johnson J, Blackwelder WC, Heimer R, Tirrell S, et al. Diarrheagenic Escherichia coli infection in Baltimore, Maryland, and New Haven, Connecticut. Clin Infect Dis. 2006;43:402–7.
Meng CY, Smith BL, Bodhidatta L, Richard SA, Vansith K, Thy B, et al. Etiology of diarrhea in young children and patterns of antibiotic resistance in Cambodia. Pediatr Infect Dis J. 2011;30:331–5.
Agócs MM, Serhan F, Yen C, Mwenda JM, de Oliveira LH, Teleb N, et al. WHO global rotavirus surveillance network: a strategic review of the first 5 years, 2008-2012. MMWR Morb Mortal Wkly Rep. 2014;63:634–7.
Rappelli P, Folgosa E, Solinas ML, Dacosta JL, Pisanu C, Sidat M, et al. Pathogenic enteric Escherichia coli in children with and without diarrhea in Maputo, Mozambique. FEMS Immunol Med Microbiol. 2005;43:67–72.
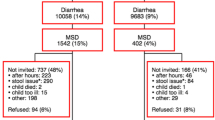
Kotloff KL, Blackwelder WC, Nasrin D, Nataro JP, Farag TH, van Eijk A, et al. The global enteric multicenter study (GEMS) of diarrheal disease in infants and young children in developing countries: epidemiologic and clinical methods of the case/control study. Clin Infect Dis. 2012;55(Suppl 4):S232–45.
•• Nhampossa T, Mandomando I, Acacio S, Quintó L, Vubil D, Ruiz J, et al. Diarrheal disease in rural Mozambique: burden, risk factors and etiology of diarrheal disease among children aged 0-59 months seeking care at health facilities. PLoS One. 2015;10:e0119824. Nhampossa et al, highlighted the contribution of pathogen specific on diarrheal burden and associated mortality showing that interventions targeting 4 pathogens could prevent more than 60% of moderate-to-severe diarrhea in infants. Data that was critical to justify the introduction of rotavirus vaccine.
Mandomando IM, Macete EV, Ruiz J, Sanz S, Abacassamo F, Vallès X, et al. Etiology of diarrhea in children younger than 5 years of age admitted in a rural hospital of southern Mozambique. Am J Trop Med Hyg. 2007;76:522–7.
• Langa JS, Thompson R, Arnaldo P, Resque HR, Rose T, Enosse SM, et al. Epidemiology of rotavirus A diarrhea in Chókwè, southern Mozambique, from February to September, 2011. J Med Virol. 2016;88:1751–8. Langa et al, in Chokwé a province of Gaza southern of Mozambique, reported the prevalence of rotavirus infection in hospitalized and non-hospitalized children with diarrhea, showing for the first time the importance of rotavirus in rural area outside of Maputo Province.
de Deus N, João E, Cuamba A, Cassocera M, Luís L, Acácio S, et al. Epidemiology of rotavirus infection in children from a rural and urban area, in Maputo, Southern Mozambique, before vaccine introduction. J Trop Pediatr. 2018;64(2):141–5.
•• de Deus N, Chilaúle JJ, Cassocera M, Bambo M, Langa JS, Sitoe E, et al. Early impact of rotavirus vaccination in children less than five years of age in Mozambique. Vaccine [Internet]. 2017; Available from: Vaccine. 2017. https://doi.org/10.1016/j.vaccine.2017.10.060. de Deus et al. reported for the first time the early impact of rotavirus vaccine in Mozambique, supporting how rotavirus vaccine could play a role on under 5 mortality reduction as part of sustainable development goals.
Bero DM, Deus ND, Costa EV, Burlandy FM, Jani IV, Silva EE. Natural circulation of human enterovirus in Maputo City. Mozambique. 2015;9:1419–23.
Daryani A, Sharif M, Nasrolahei M, Khalilian A, Mohammadi A, Barzegar G. Epidemiological survey of the prevalence of intestinal parasites among schoolchildren in Sari, northern Iran. Trans R Soc Trop Med Hyg. 2012;106:455–9.
Fonseca AM, Fernandes N, Ferreira FS, Gomes J, Centeno-Lima S. Intestinal parasites in children hospitalized at the Central Hospital in Maputo, Mozambique. J Infect Dev Ctries. 2014;8:786–9.
Cossa-Moiane ILC, Chilaule JJ, Cossa H, Cassocera M, Guimarrães E, Deus ND. Parasitic infections in children presenting with acute diarrhea in Mozambique: national surveillance data (2013 – 2015). Int J Infect Dis. 2016;45:356.
Okeke IN. Diarrheagenic Escherichia coli in sub-Saharan Africa: status, uncertainties and necessities. J Infect Dev Ctries. 2009;3:817–42.
Deen J, von Seidlein L, Andersen F, Elle N, White NJ, Lubell Y. Community-acquired bacterial bloodstream infections in developing countries in south and Southeast Asia: a systematic review. Lancet Infect Dis. 2012;12:480–7.
Kaper JB, Nataro JP, Mobley HL. Pathogenic Escherichia coli. Nat Rev Microbiol. 2004;2:123–40.
Nataro JP, Kaper JB. Diarrheagenic Escherichia coli. Clin Microbiol Rev. 1998;11:142–201.
Sumbana J, Taviani E, Manjate A, Paglietti B, Santona A, Colombo MM. Genetic determinants of pathogenicity of Escherichia coli isolated from children with acute diarrhea in Maputo, Mozambique. J Infect Dev Ctries. 2015;9:661–4.
Livio S, Strockbine NA, Panchalingam S, Tennant SM, Barry EM, Marohn ME, et al. Shigella isolates from the global enteric multicenter study inform vaccine development. Clin Infect Dis. 2014;59:933–41.
Aragón M, Barreto A, Chambule J, Noya A, Tallarico M. Shigellosis in Mozambique: the 1993 outbreak rehabilitation—a follow-up study. Trop Dr. 1995;25:159–62.
Mandomando I, Sigaúque B, Vallès X, Espasa M, Sanz S, Sacarlal J, et al. Epidemiology and clinical presentation of shigellosis in children less than five years of age in rural Mozambique. Pediatr Infect Dis J. 2007;26:1059–61.
Vubil D, Balleste-Delpierre C, Mabunda R, Acácio S, Garrine M, Nhampossa T, et al. Antibiotic resistance and molecular characterization of Shigella isolates recovered from children less than 5 years in Manhiça, Southern Mozambique. Int J Antimicrob Agents. 2018. https://doi.org/10.1016/j.ijantimicag.2018.02.005.
Davis RC. Salmonella sepsis in infancy. Am J Dis Child. 1981;135:1096–9.
Nelson SJ, Granoff D. Salmonella gastroenteritis in the first three months of life. A review of management and complications. Clin Pediatr (Phila). 1982;21:709–12.
Mandomando I, Bassat Q, Sigaúque B, Massora S, Quintó L, Ácacio S, et al. Invasive Salmonella infections among children from rural Mozambique, 2001-2014. Clin Infect Dis. 2015;61(Suppl 4):S339–45.
Ruiz J, Herrera-Leon S, Mandomando I, Macete E, Puyol L, Echeita A, et al. Detection of Salmonella enterica serotype typhimurium DT104 in Mozambique. Am J Trop Med Hyg. 2008;79:918–20.
Sigaúque B, Roca A, Mandomando I, Morais L, Quintó L, Sacarlal J, et al. Community-acquired bacteremia among children admitted to a rural hospital in Mozambique. Pediatr Infect Dis J. 2009;28:108–13.
Panchalingam S, Antonio M, Hossain A, Mandomando I, Ochieng B, Oundo J, et al. Diagnostic microbiologic methods in the GEMS-1 case/control study. Clin Infect Dis. 2012;55(Suppl 4):S294–302.
Fletcher SM, Stark D, Ellis J. Prevalence of gastrointestinal pathogens in sub-Saharan Africa: systematic review and meta-analysis. J Public Health Afr. 2011;2:e30.
Gujral L, Sema C, Rebaudet S, Taibo CLA, Manjate AA, Piarroux R, et al. Cholera epidemiology in Mozambique using national surveillance data. J Infect Dis. 2013;208(Suppl 1):S107–14.
Semá Baltazar C, Langa JP, Dengo Baloi L, Wood R, Ouedraogo I, Njanpop-Lafourcade B-M, et al. Multi-site cholera surveillance within the African Cholera Surveillance Network shows endemicity in Mozambique, 2011-2015. PLoS Negl Trop Dis. 2017;11:e0005941.
PROMED. Cólera - Moçambique (Nampula), Surto. Maputo. 806 2016. Available from: http://noticias.tvm.co.mz/index.php/saude/item/7718-c%C3%B3lera-em-nampula-autoridades-confirmam-surto-da-doen%C3%A7a-em-nampula.hhh.
WHO | Cholera – Mozambique [Internet]. [cited 2018 Mar 9]. Available from: http://www.who.int/csr/don/19-february-2018-cholera-mozambique/en/.
Démolis R, Botão C, Heyerdahl LW, Gessner BD, Cavailler P, Sinai C, et al. A rapid qualitative assessment of oral cholera vaccine anticipated acceptability in a context of resistance towards cholera intervention in Nampula, Mozambique. Vaccine. 2017. https://doi.org/10.1016/j.vaccine.2017.10.087.
•• Liu J, Platts-Mills JA, Juma J, Kabir F, Nkeze J, Okoi C, et al. Use of quantitative molecular diagnostic methods to identify causes of diarrhoea in children: a reanalysis of the GEMS case-control study. Lancet. 2016;388:1291–301. Liu et al. provided important snapshot on the future and best approach to quantify the true burden of disease - qPCR (TaqMan Array Cards - TAC) particularly for the sensitive organisms that are often underestimated by conventional microbiology techniques. This data suggest that TAC could be cost-effective platform to quantify the burden of disease in the place with limited qualified staff.
Mandomando I, Jaintilal D, Pons MJ, Vallès X, Espasa M, Mensa L, et al. Antimicrobial susceptibility and mechanisms of resistance in Shigella and Salmonella isolates from children under five years of age with diarrhea in rural Mozambique. Antimicrob Agents Chemother. 2009;53:2450–4.
Mandomando I, Sigaúque B, Morais L, Espasa M, Vallès X, Sacarlal J, et al. Antimicrobial drug resistance trends of bacteremia isolates in a rural hospital in southern Mozambique. Am J Trop Med Hyg. 2010;83:152–7.
Preziosi M, Zimba TF, Lee K, Tomas M, Kinlin S, Nhatave-Paiva C, et al. A prospective observational study of bacteraemia in adults admitted to an urban Mozambican hospital. S Afr Med J. 2015;105:370–4.
Mandomando I, Espasa M, Vallès X, Sacarlal J, Sigaúque B, Ruiz J, et al. Antimicrobial resistance of Vibrio cholerae O1 serotype Ogawa isolated in Manhiça District Hospital, southern Mozambique. J Antimicrob Chemother. 2007;60:662–4.
Dengo-Baloi LC, Semá-Baltazar CA, Manhique LV, Chitio JE, Inguane DL, Langa JP. Antibiotics resistance in El Tor Vibrio cholerae 01 isolated during cholera outbreaks in Mozambique from 2012 to 2015. PLoS One. 2017;12:e0181496.
Garrine M, Mandomando I, Vubil D, Nhampossa T, Acacio S, Li S, et al. Minimal genetic change in Vibrio cholerae in Mozambique over time: multilocus variable number tandem repeat analysis and whole genome sequencing. PLoS Negl Trop Dis. 2017;11:e0005671.
Langa JP, Sema C, De Deus N, Colombo MM, Taviani E. Epidemic waves of cholera in the last two decades in Mozambique. J Infect Dev Ctries. 2015;9:635–41.
Ansaruzzaman M, Chowdhury A, Bhuiyan NA, Sultana M, Safa A, Lucas M, et al. Characteristics of a pandemic clone of O3 : K6 and O4 : K68 Vibrio parahaemolyticus isolated in Beira, Mozambique. J Med Microbiol. 2008;57:1502–7.
Safa A, Bhuyian NA, Nusrin S, Ansaruzzaman M, Alam M, Hamabata T, et al. Genetic characteristics of Matlab variants of Vibrio cholerae O1 that are hybrids between classical and El Tor biotypes. J Med Microbiol. 2006;55:1563–9.
van der Meeren BT, Chhaganlal KD, Pfeiffer A, Gomez E, Ferro JJ, Hilbink M, et al. Extremely high prevalence of multi-resistance among uropathogens from hospitalised children in Beira, Mozambique. S Afr Med J. 2013;103:382–6.
https://mz.usembassy.gov/wp-content/uploads/sites/182/2017/06/IMASIDA-2016_Relatorio-de-Indicadores-Basicos-for-Web.pdf. IMASIDA. Inquerito de Indicadores de Imunização, Malária e HIV/SIDA em Moçambique. 2016.
sitan.unicef.org.mz/files/UNICEF-SITAN-PT_WEB.pd - Pesquisa Google [Internet]. [cited 2018 Mar 13]. Available from: https://www.google.co.mz/search?dcr=0&source=hp&ei=HEanWvT2BMe9UbSNo1g&q=sitan.unicef.org.mz%2Ffiles%2FUNICEF-SITAN-PT_WEB.pd&oq=sitan.unicef.org.mz%2Ffiles%2FUNICEF-SITAN-PT_WEB.pd&gs_l=psy-ab.3...1689.1689.0.2783.2.1.0.0.0.0.414.414.4–1.1.0....0...1c..64.psy-ab..1.0.0.0...0.YI7UahijLBY.
Nhampossa T, Sigaúque B, Machevo S, Macete E, Alonso P, Bassat Q, et al. Severe malnutrition among children under the age of 5 years admitted to a rural district hospital in southern Mozambique. Public Health Nutr. 2013;16:1565–74.
Gastañaduy PA, Steenhoff AP, Mokomane M, Esona MD, Bowen MD, Jibril H, et al. Effectiveness of monovalent rotavirus vaccine after programmatic implementation in Botswana: a multisite prospective case-control study. Clin Infect Dis. 2016;62(Suppl 2):S161–7.
https://www.mef.gov.mz/index.php/documents/80-balamco-do-pes-2009/file?force_download=1. Direccao Nacional de Obras Publicas e Habitação / Direcção Nacional das Águas MOP/DNA. Balanço do Plano Económico e Social 2008. 2009.
MISAU - Boletins Epidemiológicos [Internet]. [cited 2018 Mar 13]. Available from: http://www.misau.gov.mz/index.php/boletins-epidemiologicos.
Acknowledgements
CISM receives the core funding from Spanish Agency for International Cooperation and Development (AECID). Nilsa de Deus is a fellow from European Foundation Initiative into African Research in Neglected Tropical Diseases (EFINTD).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Assucênio Chissaque, Nilsa de Deus, Delfino Vubil, and Inácio Mandomando declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human subjects performed by any of the authors. The epidemiological studies summarized in this article were conducted under ICH guidelines.
Additional information
This article is part of the Topical Collection on Tropical Diseases of Mozambique
Rights and permissions
About this article
Cite this article
Chissaque, A., de Deus, N., Vubil, D. et al. The Epidemiology of Diarrhea in Children Under 5 Years of Age in Mozambique. Curr Trop Med Rep 5, 115–124 (2018). https://doi.org/10.1007/s40475-018-0146-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40475-018-0146-6