Abstract
Purpose of Review
While a great deal of literature has been published in recent years on infections in kidney transplant (KT) recipients, there is a relative paucity of literature on infections and their impact on the graft and overall health of older KT recipients. We reviewed the most recent literature and guidelines in the field of kidney transplantation and summarized the current recommendations for physicians caring for older KT recipients at risk for infections.
Recent Findings
Older KT recipients are at an increased risk of infections during the first year post-KT resulting in readmission or other poor outcomes, compared to younger KT recipients. Immune senescence and frailty likely increase the risk for infections in older KT recipients during the first year post-KT when KT recipients are receiving a higher degree of immune suppressive therapy. Most common infections include urinary tract infections, bloodstream infections, cytomegalovirus reactivation or primary infection, and BK virus. A majority of older KT recipients survive and have a functioning graft at 1 year.
Summary
KT can be a successful treatment for older adults on dialysis if post-transplant complications, including rejection and infection, can be appropriately managed. Despite this increased risk for infections, older KT recipients have a lower risk for all-cause mortality and death secondary to infections compared with patients on dialysis. Further studies on modification of immune suppression and prophylactic strategies are much needed in this high-risk KT population.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
• United States Renal Data System, 2019 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda: National Institute of Diabetes and Digestive and Kidney Diseases; 2019. This reference provides current statistics for older adults with end-stage renal disease on hemodialysis and older adults undergoing kidney transplantation.
Hebert SA, Ibrahim HN. Kidney transplantation in septuagenarians: 70 Is the New 60! Kidney Int Rep. 2019;4(5):640–2. https://doi.org/10.1016/j.ekir.2019.03.015.
Hart A, Smith JM, Skeans MA, Gustafson SK, Wilk AR, Castro S, et al. OPTN/SRTR 2018 Annual Data Report: Kidney. Am J Transplant. 2020;20(Suppl s1):20–130. https://doi.org/10.1111/ajt.15672.
Huang E, Segev DL, Rabb H. Kidney transplantation in the elderly. Semin Nephrol. 2009;29(6):621–35. https://doi.org/10.1016/j.semnephrol.2009.07.011.
McAdams-DeMarco MA, James N, Salter ML, Walston J, Segev DL. Trends in kidney transplant outcomes in older adults. J Am Geriatr Soc. 2014;62(12):2235–42. https://doi.org/10.1111/jgs.13130.
Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LY, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341(23):1725–30. https://doi.org/10.1056/NEJM199912023412303.
Lemoine M, Titeca Beauport D, Lobbedez T, Choukroun G, Hurault de Ligny B, Hazzan M, et al. Kidney Int Rep. 2019;4(5):656–66. https://doi.org/10.1016/j.ekir.2019.01.014.
Rao PS, Merion RM, Ashby VB, Port FK, Wolfe RA, Kayler LK. Renal transplantation in elderly patients older than 70 years of age: results from the Scientific Registry of Transplant Recipients. Transplantation. 2007;83(8):1069–74. https://doi.org/10.1097/01.tp.0000259621.56861.31.
US Renal Data System. USRDS 2008 annual data report: atlas of end-stage renal disease in the United States. Bethesda: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2008.
Tiago Silva J, Lopez-Medrano F, Aguado JM. Highlights in solid transplant infectious diseases 2015-2017. Rev Esp Quimioter. 2018;31(Suppl 1):52–5.
Meier-Kriesche HU, Ojo A, Hanson J, Cibrik D, Lake K, Agodoa LY, et al. Increased immunosuppressive vulnerability in elderly renal transplant recipients. Transplantation. 2000;69(5):885–9. https://doi.org/10.1097/00007890-200003150-00037.
Kauffman HM, McBride MA, Cors CS, Roza AM, Wynn JJ. Early mortality rates in older kidney recipients with comorbid risk factors. Transplantation. 2007;83(4):404–10. https://doi.org/10.1097/01.tp.0000251780.01031.81.
Karim A, Farrugia D, Cheshire J, Mahboob S, Begaj I, Ray D, et al. Recipient age and risk for mortality after kidney transplantation in England. Transplantation. 2014;97(8):832–8. https://doi.org/10.1097/01.TP.0000438026.03958.7b.
Meier-Kriesche HU, Ojo AO, Hanson JA, Kaplan B. Exponentially increased risk of infectious death in older renal transplant recipients. Kidney Int. 2001;59(4):1539–43. https://doi.org/10.1046/j.1523-1755.2001.0590041539.x.
Trouillhet I, Benito N, Cervera C, Rivas P, Cofan F, Almela M, et al. Influence of age in renal transplant infections: cases and controls study. Transplantation. 2005;80(7):989–92. https://doi.org/10.1097/01.tp.0000173822.05877.d7.
Kang SS, Park WY, Jin K, Park SB, Han S. Kidney transplantation in Korean patients with end-stage renal disease aged 65 and older: a single-center experience. Transplant Proc. 2017;49(5):987–91. https://doi.org/10.1016/j.transproceed.2017.03.060.
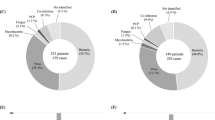
• Hemmersbach-Miller M, Alexander BD, Sudan DL, Pieper C, Schmader KE. Single-center analysis of infectious complications in older adults during the first year after kidney transplantation. Eur J Clin Microbiol Infect Dis. 2019;38(1):141–8. https://doi.org/10.1007/s10096-018-3405-5This study describes a single-center analysis on the risk of infections in older adults in the first year post-kidney transplant.
• Hemmersbach-Miller M, Alexander BD, Sudan DL, Pieper C, Schmader KE. Infections after kidney transplantation. Does age matter? Clin Transpl. 2019;33(4):e13516. https://doi.org/10.1111/ctr.13516This reference highlights increased frequency of infections in older kidney transplant recipients.
Martins PN, Pratschke J, Pascher A, Fritsche L, Frei U, Neuhaus P, et al. Age and immune response in organ transplantation. Transplantation. 2005;79(2):127–32. https://doi.org/10.1097/01.tp.0000146258.79425.04.
McKay D, Jameson J. Kidney transplantation and the ageing immune system. Nat Rev Nephrol. 2012;8(12):700–8. https://doi.org/10.1038/nrneph.2012.242.
• Schaenman JM, Rossetti M, Sidwell T, Groysberg V, Sunga G, Korin Y, et al. Increased T cell immunosenescence and accelerated maturation phenotypes in older kidney transplant recipients. Hum Immunol. 2018;79(9):659–67. https://doi.org/10.1016/j.humimm.2018.06.006This reference highlights the frequency of immunosenescence T cells in older kidney transplant recipients, increasing the risk for infections.
Dempster NJ, Ceresa CD, Aitken E, Kingsmore D. Outcomes following renal transplantation in older people: a retrospective cohort study. BMC Geriatr. 2013;13:79. https://doi.org/10.1186/1471-2318-13-79.
Bia M, Adey DB, Bloom RD, Chan L, Kulkarni S, Tomlanovich S. KDOQI US commentary on the 2009 KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Kidney Dis. 2010;56(2):189–218. https://doi.org/10.1053/j.ajkd.2010.04.010.
Pham C, Kuten SA, Knight RJ, Nguyen DT, Graviss EA, Gaber AO. Assessment of infectious complications in elderly kidney transplant recipients receiving induction with anti-thymocyte globulin vs basiliximab. Transpl Infect Dis. 2020;22(3):e13257. https://doi.org/10.1111/tid.13257.
Meier-Kriesche HU, Friedman G, Jacobs M, Mulgaonkar S, Vaghela M, Kaplan B. Infectious complications in geriatric renal transplant patients: comparison of two immunosuppressive protocols. Transplantation. 1999;68(10):1496–502. https://doi.org/10.1097/00007890-199911270-00012.
Johnson DW, Nicol DL, Purdie DM, Preston JM, Brown AM, Hawley CM, et al. Is mycophenolate mofetil less safe than azathioprine in elderly renal transplant recipients? Transplantation. 2002;73(7):1158–63. https://doi.org/10.1097/00007890-200204150-00027.
Sureshkumar KK, Nghiem DD. Use of mycophenolate mofetil in immunosuppressive protocols in elderly renal transplant recipients. Transplantation. 2003;76(2):441–2. https://doi.org/10.1097/01.TP.0000074313.67552.46.
Seyda M, Quante M, Uehara H, Slegtenhorst BR, Elkhal A, Tullius SG. Immunosenescence in renal transplantation: a changing balance of innate and adaptive immunity. Curr Opin Organ Transplant. 2015;20(4):417–23. https://doi.org/10.1097/MOT.0000000000000210.
Neri F, Furian L, Cavallin F, Ravaioli M, Silvestre C, Donato P, et al. How does age affect the outcome of kidney transplantation in elderly recipients? Clin Transpl. 2017;31(10). https://doi.org/10.1111/ctr.13036.
Lehner LJ, Staeck O, Halleck F, Liefeldt L, Bamoulid J, Budde K. Need for optimized immunosuppression in elderly kidney transplant recipients. Transplant Rev (Orlando). 2015;29(4):237–9. https://doi.org/10.1016/j.trre.2015.08.001.
Hod T, Goldfarb-Rumyantzev AS. Clinical issues in renal transplantation in the elderly. Clin Transpl. 2015;29(2):167–75. https://doi.org/10.1111/ctr.12481.
Rana A, Murthy B, Pallister Z, Kueht M, Cotton R, Galvan NTN, et al. Profiling risk for acute rejection in kidney transplantation: recipient age is a robust risk factor. J Nephrol. 2017;30(6):859–68. https://doi.org/10.1007/s40620-016-0354-x.
Mendonca HM, Dos Reis MA, de Castro de Cintra SR, Camara NO, Pacheco-Silva A. Renal transplantation outcomes: a comparative analysis between elderly and younger recipients. Clin Transpl. 2007;21(6):755–60. https://doi.org/10.1111/j.1399-0012.2007.00734.x.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Cardiovascular Health Study Collaborative Research G. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–56. https://doi.org/10.1093/gerona/56.3.m146.
• McAdams-DeMarco MA, Law A, King E, Orandi B, Salter M, Gupta N, et al. Frailty and mortality in kidney transplant recipients. Am J Transplant. 2015;15(1):149–54. https://doi.org/10.1111/ajt.12992This reference highlights the association of frailty with mortality in kidney transplant recipients.
• McAdams-DeMarco MA, Isaacs K, Darko L, Salter ML, Gupta N, King EA, et al. Changes in frailty after kidney transplantation. J Am Geriatr Soc. 2015;63(10):2152–7. https://doi.org/10.1111/jgs.13657This reference provides a description of changes in frailty in older kidney transplant recipients at the time of transplant and in post-transplant period.
Garonzik-Wang JM, Govindan P, Grinnan JW, Liu M, Ali HM, Chakraborty A, et al. Frailty and delayed graft function in kidney transplant recipients. Arch Surg. 2012;147(2):190–3. https://doi.org/10.1001/archsurg.2011.1229.
• McAdams-Demarco MA, Grams ME, Hall EC, Coresh J, Segev DL. Early hospital readmission after kidney transplantation: patient and center-level associations. Am J Transplant. 2012;12(12):3283–8. https://doi.org/10.1111/j.1600-6143.2012.04285.xThis reference highlights the association of frailty with early hospital admissions in kidney transplant recipients.
• McAdams-DeMarco MA, Law A, Tan J, Delp C, King EA, Orandi B, et al. Frailty, mycophenolate reduction, and graft loss in kidney transplant recipients. Transplantation. 2015;99(4):805–10. https://doi.org/10.1097/TP.0000000000000444This study describes incidence of mycophenolate dose reduction due to side effects in frail kidney transplant recipients, and older adults, and mycophenolate dose reduction to be associated with increased risk of graft loss.
Yoshikawa TT, Norman DC. Geriatric infectious diseases: current concepts on diagnosis and management. J Am Geriatr Soc. 2017;65(3):631–41. https://doi.org/10.1111/jgs.14731.
Malinis MO, Luo J, Zhang Y, Asch W, Deshpande R, Akhtar S. Frailty is predictive of early post-transplant infection in older renal transplant recipients [abstract]. https://atcmeetingabstracts.com/abstract/frailty-is-predictive-of-early-post-transplant-infection-in-older-renal-transplant-recipients/. .
Norman JGA, Naik A, Cibrik D, Norman S. The association of frailty with risk of cytomegalovirus and BK infection. Am Transpl Congress. 2019.
Zhou Q, Fan L, Lai X, Tan L, Zhang X. Estimating extra length of stay and risk factors of mortality attributable to healthcare-associated infection at a Chinese university hospital: a multi-state model. BMC Infect Dis. 2019;19(1):975. https://doi.org/10.1186/s12879-019-4474-5.
Serra-Burriel M, Keys M, Campillo-Artero C, Agodi A, Barchitta M, Gikas A, et al. Impact of multi-drug resistant bacteria on economic and clinical outcomes of healthcare-associated infections in adults: systematic review and meta-analysis. PLoS One. 2020;15(1):e0227139. https://doi.org/10.1371/journal.pone.0227139 PubMed PMID: 31923281; PMCID: PMC6953842 following competing interests: MSB acknowledges research grants from Horizon2020, EiTHealth and ISCI programs outside of the submitted work, MK;CCA;AA;MB;CP;GLC declare no competing interests.
Tang M, Quanstrom K, Jin C, Suskind AM. Recurrent urinary tract infections are associated with frailty in older adults. Urology. 2019;123:24–7. https://doi.org/10.1016/j.urology.2018.09.025.
Gulliford MC, Charlton J, Winter JR, Sun X, Rezel-Potts E, Bunce C, et al. Probability of sepsis after infection consultations in primary care in the United Kingdom in 2002-2017: population-based cohort study and decision analytic model. PLoS Med. 2020;17(7):e1003202. https://doi.org/10.1371/journal.pmed.1003202.
Cichero JAY. Age-related changes to eating and swallowing impact frailty: aspiration, choking risk, modified food texture and autonomy of choice. Geriatrics (Basel). 2018;3(4). https://doi.org/10.3390/geriatrics3040069.
Goldman JD, Julian K. Urinary tract infections in solid organ transplant recipients: Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transpl. 2019;33(9):e13507. https://doi.org/10.1111/ctr.13507.
Skogberg K, Lyytikainen O, Ollgren J, Nuorti JP, Ruutu P. Population-based burden of bloodstream infections in Finland. Clin Microbiol Infect. 2012;18(6):E170–6. https://doi.org/10.1111/j.1469-0691.2012.03845.x.
Yahav D, Eliakim-Raz N, Leibovici L, Paul M. Bloodstream infections in older patients. Virulence. 2016;7(3):341–52. https://doi.org/10.1080/21505594.2015.1132142.
Reunes S, Rombaut V, Vogelaers D, Brusselaers N, Lizy C, Cankurtaran M, et al. Risk factors and mortality for nosocomial bloodstream infections in elderly patients. Eur J Intern Med. 2011;22(5):e39–44. https://doi.org/10.1016/j.ejim.2011.02.004.
Kritikos A, Manuel O. Bloodstream infections after solid-organ transplantation. Virulence. 2016;7(3):329–40. https://doi.org/10.1080/21505594.2016.1139279.
Al-Hasan MN, Razonable RR, Eckel-Passow JE, Baddour LM. Incidence rate and outcome of Gram-negative bloodstream infection in solid organ transplant recipients. Am J Transplant. 2009;9(4):835–43. https://doi.org/10.1111/j.1600-6143.2009.02559.x.
Silva M Jr, Marra AR, Pereira CA, Medina-Pestana JO, Camargo LF. Bloodstream infection after kidney transplantation: epidemiology, microbiology, associated risk factors, and outcome. Transplantation. 2010;90(5):581–7. https://doi.org/10.1097/TP.0b013e3181e8a680.
Moreno A, Cervera C, Gavalda J, Rovira M, de la Camara R, Jarque I, et al. Bloodstream infections among transplant recipients: results of a nationwide surveillance in Spain. Am J Transplant. 2007;7(11):2579–86. https://doi.org/10.1111/j.1600-6143.2007.01964.x.
• Razonable RR, Humar A. Cytomegalovirus in solid organ transplant recipients-Guidelines of the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transpl. 2019;33(9):e13512. https://doi.org/10.1111/ctr.13512This reference is a guideline from the American Society of Transplant Infectious Disease Community of Practice for the prevention, diagnosis, clinical manifestations, complications, and management of cytomegalovirus infection in solid organ transplant recipients.
Azevedo LS, Pierrotti LC, Abdala E, Costa SF, Strabelli TM, Campos SV, et al. Cytomegalovirus infection in transplant recipients. Clinics (Sao Paulo). 2015;70(7):515–23. https://doi.org/10.6061/clinics/2015(07)09.
Smedbraten YV, Sagedal S, Leivestad T, Mjoen G, Osnes K, Rollag H, et al. The impact of early cytomegalovirus infection after kidney transplantation on long-term graft and patient survival. Clin Transpl. 2014;28(1):120–6. https://doi.org/10.1111/ctr.12288.
Garcia-Testal A, Olague Diaz P, Bonilla Escobar BA, Criado-Alvarez JJ, Sanchez PJ. Analysis of cytomegalovirus infection and its consequences in renal transplantation: a decade analysis. Med Clin (Barc). 2011;137(8):335–9. https://doi.org/10.1016/j.medcli.2010.12.023.
• Hemmersbach-Miller M, Alexander BD, Pieper CF, Schmader KE. Age matters: older age as a risk factor for CMV reactivation in the CMV serostatus-positive kidney transplant recipient. Eur J Clin Microbiol Infect Dis. 2020;39(3):455–63. https://doi.org/10.1007/s10096-019-03744-3This study describes increased risk of cytomegalovirus reactivation in CMV seropositive older kidney transplant recipients.
Luna E, Caravaca F, Ferreira F, Fernandez N, Martin P, Vargas ML, et al. Effect of cytomegalovirus infection on survival of older kidney transplant patients (D+/R+): impact of valganciclovir prophylaxis versus preemptive therapy. Transplant Proc. 2016;48(9):2931–7. https://doi.org/10.1016/j.transproceed.2016.06.062.
Souquette A, Frere J, Smithey M, Sauce D, Thomas PG. A constant companion: immune recognition and response to cytomegalovirus with aging and implications for immune fitness. Geroscience. 2017;39(3):293–303. https://doi.org/10.1007/s11357-017-9982-x.
Blum A, Giladi M, Weinberg M, Kaplan G, Pasternack H, Laniado S, et al. High anti-cytomegalovirus (CMV) IgG antibody titer is associated with coronary artery disease and may predict post-coronary balloon angioplasty restenosis. Am J Cardiol. 1998;81(7):866–8. https://doi.org/10.1016/s0002-9149(98)00019-8.
Freeman RB Jr. The ‘indirect’ effects of cytomegalovirus infection. Am J Transplant. 2009;9(11):2453–8. https://doi.org/10.1111/j.1600-6143.2009.02824.x.
Grahame-Clarke C. Human cytomegalovirus, endothelial function and atherosclerosis. Herpes. 2005;12(2):42–5.
Mathei C, Vaes B, Wallemacq P, Degryse J. Associations between cytomegalovirus infection and functional impairment and frailty in the BELFRAIL Cohort. J Am Geriatr Soc. 2011;59(12):2201–8. https://doi.org/10.1111/j.1532-5415.2011.03719.x.
Leitheiser S, Harner A, Waller JL, Turrentine J, Baer S, Kheda M, et al. Risk factors associated with invasive fungal infections in kidney transplant patients. Am J Med Sci. 2020;359(2):108–16. https://doi.org/10.1016/j.amjms.2019.10.008.
Miller R, Assi M, Practice ASTIDCo. Endemic fungal infections in solid organ transplant recipients-Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transpl. 2019;33(9):e13553. https://doi.org/10.1111/ctr.13553.
• Danziger-Isakov L, Kumar D, Practice AICo. Vaccination of solid organ transplant candidates and recipients: guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transpl. 2019;33(9):e13563. https://doi.org/10.1111/ctr.13563This reference is a guideline from the American Society of Transplant Infectious Disease Community of Practice and highlights the necessity and timeline of vaccinations in solid organ transplant candidates and recipients.
Chadban SJ, Ahn C, Axelrod DA, Foster BJ, Kasiske BL, Kher V, et al. KDIGO Clinical Practice Guideline on the Evaluation and Management of Candidates for Kidney Transplantation. Transplantation. 2020;104(4S1 Suppl 1):S11–S103. https://doi.org/10.1097/TP.0000000000003136.
Dendle C, Stuart RL, Polkinghorne KR, Balloch A, Kanellis J, Ling J, et al. Seroresponses and safety of 13-valent pneumococcal conjugate vaccination in kidney transplant recipients. Transpl Infect Dis. 2018;20(2):e12866. https://doi.org/10.1111/tid.12866.
Jain SR, Kumar D. Vaccination for the post-kidney transplant population. Curr Opin Nephrol Hypertens. 2019;28(6):581–6. https://doi.org/10.1097/MNH.0000000000000546.
Miller-Handley H, Paulsen G, Hooper DK, Lake M, Lazear D, Danziger-Isakov L. Durability of the hepatitis B vaccination in pediatric renal transplant recipients. Clin Transpl. 2018;32(5):e13247. https://doi.org/10.1111/ctr.13247.
• Vink P, Ramon Torrell JM, Sanchez Fructuoso A, Kim SJ, Kim SI, Zaltzman J, et al. Immunogenicity and safety of the adjuvanted recombinant zoster vaccine in chronically immunosuppressed adults following renal transplant: a phase 3, randomized clinical trial. Clin Infect Dis. 2020;70(2):181–90. https://doi.org/10.1093/cid/ciz177This randomized clinical trial highlights the safety and immunogenicity of the recombinant zoster vaccine in kidney transplant recipients.
Avery RK. Influenza vaccines in the setting of solid-organ transplantation: are they safe? Curr Opin Infect Dis. 2012;25(4):464–8. https://doi.org/10.1097/QCO.0b013e328355a79b.
Chong PP, Avery RK. A comprehensive review of immunization practices in solid organ transplant and hematopoietic stem cell transplant recipients. Clin Ther. 2017;39(8):1581–98. https://doi.org/10.1016/j.clinthera.2017.07.005.
Hurst FP, Lee JJ, Jindal RM, Agodoa LY, Abbott KC. Outcomes associated with influenza vaccination in the first year after kidney transplantation. Clin J Am Soc Nephrol. 2011;6(5):1192–7. https://doi.org/10.2215/CJN.05430610.
White-Williams C, Brown R, Kirklin J, St Clair K, Keck S, O’Donnell J, et al. Improving clinical practice: should we give influenza vaccinations to heart transplant patients? J Heart Lung Transplant. 2006;25(3):320–3. https://doi.org/10.1016/j.healun.2005.09.015.
• Dooling KL, Guo A, Patel M, Lee GM, Moore K, Belongia EA, et al. Recommendations of the Advisory Committee on Immunization Practices for use of herpes zoster vaccines. MMWR Morb Mortal Wkly Rep. 2018;67(3):103–8. https://doi.org/10.15585/mmwr.mm6703a5This reference highlights guidelines by the Advisory Committee on Immunization Practices for use of Zoster vaccine in adults.
• Malinis M, Boucher HW, Practice ASTIDCo. Screening of donor and candidate prior to solid organ transplantation-Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transpl. 2019;33(9):e13548. https://doi.org/10.1111/ctr.13548.This reference is a guideline from the American Society of Transplant Infectious Disease community of practice on recommendations for transplant donor and candidate screening prior to transplantation.
• Rajagopalan S. Tuberculosis in older adults. Clin Geriatr Med. 2016;32(3):479–91. https://doi.org/10.1016/j.cger.2016.02.006This review highlights clinical nuances in tuberculosis and its diagnostic tests in older adults.
Centers for Disease C, Prevention. Tuberculosis transmission in a renal dialysis center--Nevada, 2003. MMWR Morb Mortal Wkly Rep. 2004;53(37):873–5.
Abbara A, Collin SM, Kon OM, Buell K, Sullivan A, Barrett J, et al. Time to diagnosis of tuberculosis is greater in older patients: a retrospective cohort review. ERJ Open Res. 2019;5(4). https://doi.org/10.1183/23120541.00228-2018S.M. Collin has nothing to disclose. Conflict of interest: O.M. Kon has nothing to disclose. Conflict of interest: K. Buell has nothing to disclose. Conflict of interest: A. Sullivan has nothing to disclose. Conflict of interest: J. Barrett has nothing to disclose. Conflict of interest: T. Corrah has nothing to disclose. Conflict of interest: A. McGregor has nothing to disclose. Conflict of interest: T. Hansel has nothing to disclose. Conflict of interest: L. John has nothing to disclose. Conflict of interest: R.N. Davidson has nothing to disclose.
Anand M, Nayyar E, Concepcion B, Salani M, Schaefer H. Tuberculosis in kidney transplant recipients: a case series. World J Transplant. 2017;7(3):213–21. https://doi.org/10.5500/wjt.v7.i3.213.
Kafle M, Sigdel MR, Shrestha M, Nepali R, Chhetri S, Shah DS. Tuberculosis in living donor kidney transplant recipients. Transplantation. 2018;102:S664. https://doi.org/10.1097/01.tp.0000543597.47545.0a.
Funding
KME is supported in part by NIH/NIA R01 AG054366 and NIH/NCATS Colorado CTSA Grant Number UL1 TR002535.
Author information
Authors and Affiliations
Contributions
MZA performed a review of the literature and drafted the manuscript. KME, as the senior author, contributed by outlining content and critical reviewing and revisioning the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Disclaimer
The contents are the authors’ sole responsibility and do not necessarily represent official NIH views.
Conflict of interest
KME has received research funding (to the university) from Gilead Sciences and has consulted (payments to the university) for ViiV/GSK and Theratechnologies.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Frailty and Gerontology
Rights and permissions
About this article
Cite this article
Abidi, M.Z., Erlandson, K.M. A Comprehensive Review of Infections in Older Kidney Transplant Recipients. Curr Transpl Rep 8, 90–99 (2021). https://doi.org/10.1007/s40472-021-00320-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-021-00320-7