Abstract
Purpose of Review
Non-directed living kidney donors (NDDs) are unique from the traditional directed living donors in terms of the circumstances that led NDDs to undergo a donation. The purpose of this study was to synthesize and discuss key similarities, differences, and existing gaps in the literature comparing their kidney donation process experiences and post-donation outcomes among directed and non-directed donors.
Recent Findings
A total of eight recent studies were reviewed as part of this study. These studies provided insights into the socioeconomic, physical, and mental health outcomes experienced by NDDs and directed donors throughout the various stages of the evaluation and donation process. Among the studies, NDDs were generally not found to demonstrate having substantial differences as compared to the traditional directed donor within the realms of physical and psychosocial health outcomes post-donation. However, NDDs did have fewer financial burdens as compared to directed donors, which may be related to the differences in demographic characteristics and the limited study sample sizes.
Summary
Recent evidence on outcomes among non-directed living donors as compared with directed donors should inform efforts to enhance the evaluation and post-donation experiences for this special population. While future studies remain warranted, the current literature signals that further improvements can be made by revisiting the current evaluation screening protocols for living kidney donation as well as the donation system’s infrastructure to help yield enhanced outcomes and experiences among both directed and non-directed donors.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hart A, Smith JM, Skeans MA, Gustafson SK, Wilk AR, Castro S, et al. OPTN/SRTR 2018 annual data report: kidney. Am J Transplant. 2020;20(Suppl s1):20–130.
Organ Procurement and Transplantation Network. Living non-directed donors. US Department of Health and Human Services. Last updated Dec 2015. Last accessed on February 24, 2020. Retrieved from: https://optn.transplant.hrsa.gov/resources/ethics/living-non-directed-organ-donation/.
Dor FJ, Massey EK, Frunza M, Johnson R, Lennerling A, Lovén C, et al. New classification of ELPAT for living organ donation. Transplantation. 2011;91(9):935–8. https://doi.org/10.1097/TP.0b013e3182129236.
Lentine KL, Schnitzler MA, Xiao H, Saab G, Salvalaggio PR, Axelrod D, et al. Racial variation in medical outcomes among living kidney donors. N Engl J Med. 2010;363(8):724–32. https://doi.org/10.1056/NEJMoa1000950.
Muzaale AD, Massie AB, Wang MC, Montgomery RA, McBride MA, Wainright JL, et al. Risk of end-stage renal disease following live kidney donation. JAMA. 2014;311(6):579–86.
Wainright JL, Robinson AM, Wilk AR, Klassen DK, Cherikh WS, Stewart DE. Risk of ESRD in prior living kidney donors. Am J Transplant. 2018;18(5):1129–39.
Lentine KL, Lam NN, Segev DL. Risks of living kidney donation: current state of knowledge on outcomes important to donors. Clin J Am Soc Nephrol. 2019;14(4):597–608. https://doi.org/10.2215/CJN.11220918.
Gross CR, Messersmith EE, Hong BA, Jowsey SG, Jacobs C, Gillespie BW, et al. RELIVE study group: health-related quality of life in kidney donors from the last five decades: results from the RELIVE study. Am J Transplant. 2013;13:2924–34.
Ibrahim HN, Foley RN, Reule SA, Spong R, Kukla A, Issa N, et al. Renal function profile in white kidney donors: the first 4 decades. J Am Soc Nephrol. 2016;27(9):2885–93.
Massie AB, Muzaale AD, Luo X, Chow EKH, Locke JE, Nguyen AQ, et al. Quantifying postdonation risk of ESRD in living kidney donors. J Am Soc Nephrol. 2017;28(9):2749–55.
Muzaale AD, Massie AB, Al Ammary F, Henderson ML, Purnell TS, Holscher CM, et al. Donor-recipient relationship and risk of ESKD in live kidney donors of varied racial groups. Am J Kidney Dis. 2019. https://doi.org/10.1053/j.ajkd.2019.08.020.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
Timmerman L, Timman R, Laging M, Zuidema WC, Beck DK, IJzermans JNM, et al. Predicting mental health after living kidney donation: the importance of psychological factors. Br J Health Psychol. 2016;21(3):533–54 This study identified psychological risk factors that influence living donors’ mental health during the donation process and after donation.
Maple H, Chilcot J, Burnapp L, Gibbs P, Santhouse A, Norton S, et al. Motivations, outcomes, and characteristics of unspecified (nondirected altruistic) kidney donors in the United Kingdom. Transplantation. 2014;98(11):1182–9.
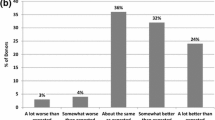
Rodrigue JR, Schutzer ME, Paek M, Morrissey P. Altruistic kidney donation to a stranger: psychosocial and functional outcomes at two US transplant centers. Transplantation. 2011;91(7):772–8 Study authors compared the psychosocial and functional outcomes of altruistic living donors to a stranger with traditional living donors who have a longstanding relationship with the recipient.
Wiseman JF, Jacobs CL, Larson DB, Berglund DM, Garvey CA, Ibrahim HN, et al. Financial burden borne by laparoscopic living kidney donors. Transplantation. 2017;101(9):2253–7.
Przech S, Garg AX, Arnold JB, Barnieh L, Cuerden MS, Dipchand C, et al. Financial costs incurred by living kidney donors: a prospective cohort study. J Am Soc Nephrol. 2018;29(12):2847–57 Study authors concluded that on average, total financial costs were higher in spousal compared with non-spousal living donors, and also higher in directed donors compared with non-directed donors.
Larson DB, Wiseman JF, Vock DM, Berglund DM, Roman AM, Ibrahim HN, et al. Financial burden associated with time to return to work after living kidney donation. Am J Transplant. 2019;19(1):204–7.
Shaw RM, Bell LJ. ‘Because you can’t live on love’: living kidney donors’ perspectives on compensation and payment for organ donation. Health Expect. 2015;18(6):3201–12.
Hays R, Thomas AE, Mathias E, Mezrich J, Mandelbrot DA. Barriers to the use of a federal travel grant by living kidney donors. Clin Transpl. 2017;31:e12876.
Reimbursement of travel and subsistence expenses toward living organ donation program eligibility guidelines, 85 Fed Reg 59530 (September 22, 2020).
Removing financial disincentives to living organ donation, 84 Fed Reg 59438 (September 22, 2020) (codified at 42 CFR Pt 121).
Funding
This work was supported in part by grant K01HS024600 (PI: Dr. Purnell) from the Agency for Healthcare Research and Quality. The funders had no role in the design and conduct of the study, interpretation of the data, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Live Kidney Donation
Rights and permissions
About this article
Cite this article
Perkins, J.A., Vargas, G.B., Johnson, M. et al. Psychological and Socioeconomic Outcomes Among Directed and Non-directed Living Kidney Donors. Curr Transpl Rep 8, 35–43 (2021). https://doi.org/10.1007/s40472-021-00314-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-021-00314-5