Abstract
Purpose of Review
Cognitive impairment is common in kidney transplant recipients and affects quality of life, graft survival, morbidity, and mortality. In this review article we discuss the epidemiology, diagnosis, pathophysiology, and future directions for cognitive impairment in kidney transplantation. We describe the potential role of pre-transplant cognition, immunosuppression, and peri-transplant factors in post-transplant cognitive impairment.
Recent Findings
A majority of patients with kidney transplant have cognitive impairment. Cognitive impairment affects both pre-transplant evaluation and post-transplant outcomes. Failure to identify patients with cognitive impairment can withhold appropriate care and timely intervention.
Summary
Cognitive impairment is common in kidney transplant and affects outcomes. Studies addressing modifiable risk factors and possible interventions to slow cognitive decline in patients with kidney disease are needed.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Gupta A, Montgomery RN, Bedros V, et al. Subclinical cognitive impairment and listing for kidney transplantation. Clinical journal of the American Society of Nephrology : CJASN. 2019;14(4):567–75 This study highlights the importance of subclinical cognitive impairment in the selection of patients for kidney transplantation. Patients with cognitive impairment have a lower liklihood of being listed for kidney transplant and take longer to get listed.
Patzer RE, Serper M, Reese PP, Przytula K, Koval R, Ladner DP, et al. Medication understanding, non-adherence, and clinical outcomes among adult kidney transplant recipients. Clin Transpl. 2016;30(10):1294–305.
• McAdams-DeMarco MA, Bae S, Chu N, et al. Dementia and Alzheimer’s disease among older kidney transplant recipients. J Am Soc Nephrol. 2017;28(5):1575–83 This study reflects the high burden of dementia in older patients with kidney transplant.
van den Ham EC, Kooman JP, Schols AM, et al. Similarities in skeletal muscle strength and exercise capacity between renal transplant and hemodialysis patients. Am J Transplant Off J Am Soc Transplant Am Soc Transplant Surg. 2005;5(8):1957–65.
Haugen CE, Mountford A, Warsame F, Berkowitz R, Bae S, G. Thomas A, et al. Incidence, risk factors, and sequelae of post-kidney transplant delirium. J Am Soc Nephrol. 2018;29(6):1752–9.
Murray AM, Tupper DE, Knopman DS, Gilbertson DT, Pederson SL, Li S, et al. Cognitive impairment in hemodialysis patients is common. Neurology. 2006;67(2):216–23.
Kalirao P, Pederson S, Foley RN, Kolste A, Tupper D, Zaun D, et al. Cognitive impairment in peritoneal dialysis patients. Am J Kidney Dis. 2011;57(4):612–20.
Haugen CE, Chu NM, Ying H, Warsame F, Holscher CM, Desai NM, et al. Frailty and access to kidney transplantation. Clinical journal of the American Society of Nephrology : CJASN. 2019;14(4):576–82.
Griva K, Thompson D, Jayasena D, Davenport A, Harrison M, Newman SP. Cognitive functioning pre- to post-kidney transplantation--a prospective study. Nephrol Dial Transplant. 2006;21(11):3275–82.
Radic J, Ljutic D, Radic M, Kovacic V, Dodig-Curkovic K, Sain M. Kidney transplantation improves cognitive and psychomotor functions in adult hemodialysis patients. Am J Nephrol. 2011;34(5):399–406.
Ozcan H, Yucel A, Avsar UZ, et al. Kidney transplantation is superior to hemodialysis and peritoneal dialysis in terms of cognitive function, anxiety, and depression symptoms in chronic kidney disease. Transplant Proc. 2015;47(5):1348–51.
Kramer L, Madl C, Stockenhuber F, Yeganehfar W, Eisenhuber E, Derfler K, et al. Beneficial effect of renal transplantation on cognitive brain function. Kidney Int. 1996;49(3):833–8.
• Gupta A, Lepping RJ, Yu AS, et al. Cognitive function and white matter changes associated with renal transplantation. Am J Nephrol. 2016;43(1):50–7 In this study there was an improvement in cognition and changes in white matter integrity after kidney transplantation. Furthermore, the tracts with improvement in diffusion tensor imaging metrics were associated with domains of cognition that improved after transplant.
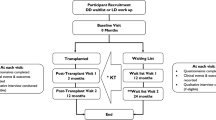
•• Chu NM, Gross AL, Shaffer AA, et al. Frailty and changes in cognitive function after kidney transplantation. Journal of the American Society of Nephrology. 2019;30(2):336 This study shows an association between change in cognitive impairment and frailty pre- to post-kidney transplantation.
Nohre M, Bauer-Hohmann M, Klewitz F, et al. Prevalence and correlates of cognitive impairment in kidney transplant patients using the DemTect-results of a KTx360 substudy. Front Psychiatry. 2019;10:791.
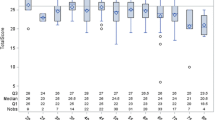
•• Gupta A, Mahnken JD, Johnson DK, et al. Prevalence and correlates of cognitive impairment in kidney transplant recipients. BMC nephrology. 2017;18(1):158 This study highlights the high prevalence of cognitive impairmnt in kidney transplant recipients.
Unverzagt FW, Gao S, Baiyewu O, et al. Prevalence of cognitive impairment. Data from the Indianapolis Study of Health and Aging. Neurology. 2001;57(9):1655–62.
Kurella Tamura M, Wadley V, Yaffe K, McClure LA, Howard G, Go R, et al. Kidney function and cognitive impairment in US adults: the reasons for geographic and Racial Differences in Stroke (REGARDS) study. Am J Kidney Dis. 2008;52(2):227–34.
Knopman DS, Petersen RC. Mild cognitive impairment and mild dementia: a clinical perspective. Mayo Clin Proc. 2014;89(10):1452–9.
Langa KM, Levine DA. The diagnosis and management of mild cognitive impairment: a clinical review. Jama. 2014;312(23):2551–61.
• Gupta A, Thomas TS, Klein JA, et al. Discrepancies between perceived and measured cognition in kidney transplant recipients: implications for clinical management. Nephron. 2018;138(1):22–8 This study indicates that an objective assessment of cognition is required and perceived assessment of a patient’s cogniton is often inaccurate.
Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
Crum RM, Anthony JC, Bassett SS, Folstein MF. Population-based norms for the Mini-Mental State Examination by age and educational level. Jama. 1993;269(18):2386–91.
Nasreddine ZS, Phillips NA, Bedirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9.
Ciesielska N, Sokolowski R, Mazur E, Podhorecka M, Polak-Szabela A, Kedziora-Kornatowska K. Is the Montreal Cognitive Assessment (MoCA) test better suited than the Mini-Mental State Examination (MMSE) in mild cognitive impairment (MCI) detection among people aged over 60? Meta-analysis. Psychiatr Pol. 2016;50(5):1039–52.
Lee SH, Cho A, Min YK, Lee YK, Jung S. Comparison of the Montreal Cognitive Assessment and the Mini-Mental State Examination as screening tests in hemodialysis patients without symptoms. Ren Fail. 2018;40(1):323–30.
Solias A, Skapinakis P, Degleris N, Pantoleon M, Katirtzoglou E, Politis A. Mini Mental State Examination (MMSE): determination of cutoff scores according to age and educational level. Psychiatriki. 2014;25(4):245–56.
Creavin ST, Wisniewski S, Noel-Storr AH, et al. Mini-Mental State Examination (MMSE) for the detection of dementia in clinically unevaluated people aged 65 and over in community and primary care populations. Cochrane Database Syst Rev. 2016;1:Cd011145.
Michieletto F, Binkin N, Saugo M, Boorson S, Scanlan J. Use of the Mini-Cog test as a screening method for dementia in the Italian population: the Argento Study results. Ig Sanita Pubbl. 2006;62(2):159–72.
Carnero-Pardo C, Cruz-Orduna I, Espejo-Martinez B, Martos-Aparicio C, Lopez-Alcalde S, Olazaran J. Utility of the Mini-Cog for detection of cognitive impairment in primary care: data from two spanish studies. Int J Alzheimers Dis. 2013;2013:285462.
Bland RC, Newman SC. Mild dementia or cognitive impairment: the Modified Mini-Mental State Examination (3MS) as a screen for dementia. Can J Psychiatr. 2001;46(6):506–10.
Watanabe K, Watanabe T, Nakayama M. Cerebro-renal interactions: impact of uremic toxins on cognitive function. Neurotoxicology. 2014;44:184–93.
Seifter JL, Samuels MA. Uremic encephalopathy and other brain disorders associated with renal failure. Semin Neurol. 2011;31(2):139–43.
Kurella M, Chertow GM, Luan J, Yaffe K. Cognitive impairment in chronic kidney disease. J Am Geriatr Soc. 2004;52(11):1863–9.
Ito S, Nagasawa T, Abe M, Mori T. Strain vessel hypothesis: a viewpoint for linkage of albuminuria and cerebro-cardiovascular risk. Hypertens Res. 2009;32(2):115–21.
Elewa U, Sanchez-Nino MD, Martin-Cleary C, Fernandez-Fernandez B, Egido J, Ortiz A. Cardiovascular risk biomarkers in CKD: the inflammation link and the road less traveled. Int Urol Nephrol. 2012;44(6):1731–44.
Kaysen GA. The microinflammatory state in uremia: causes and potential consequences. J Am Soc Nephrol. 2001;12(7):1549–57.
Jing W, Jabbari B, Vaziri ND. Uremia induces upregulation of cerebral tissue oxidative/inflammatory cascade, down-regulation of Nrf2 pathway and disruption of blood brain barrier. Am J Transl Res. 2018;10(7):2137–47.
Vaziri ND. Oxidative stress in uremia: nature, mechanisms, and potential consequences. Semin Nephrol. 2004;24(5):469–73.
Kurella Tamura M, Chertow GM, Depner TA, Nissenson AR, Schiller B, Mehta RL, et al. Metabolic profiling of impaired cognitive function in patients receiving dialysis. J Am Soc Nephrol. 2016;27(12):3780–7.
Ohtsuki S, Asaba H, Takanaga H, Deguchi T, Hosoya KI, Otagiri M, et al. Role of blood-brain barrier organic anion transporter 3 (OAT3) in the efflux of indoxyl sulfate, a uremic toxin: its involvement in neurotransmitter metabolite clearance from the brain. J Neurochem. 2002;83(1):57–66.
Kloppenborg RP, Geerlings MI, Visseren FL, Mali WPTM, Vermeulen M, van der Graaf Y, et al. Homocysteine and progression of generalized small-vessel disease: the SMART-MR study. Neurology. 2014;82(9):777–83.
van den Kommer TN, Dik MG, Comijs HC, Jonker C, Deeg DJ. Homocysteine and inflammation: predictors of cognitive decline in older persons? Neurobiol Aging. 2010;31(10):1700–9.
Vannorsdall TD, Jinnah HA, Gordon B, Kraut M, Schretlen DJ. Cerebral ischemia mediates the effect of serum uric acid on cognitive function. Stroke. 2008;39(12):3418–20.
Prins ND, van Dijk EJ, den Heijer T, Vermeer SE, Koudstaal PJ, Oudkerk M, et al. Cerebral white matter lesions and the risk of dementia. Arch Neurol. 2004;61(10):1531–4.
Iadecola C. The pathobiology of vascular dementia. Neuron. 2013;80(4):844–66.
Drew DA, Bhadelia R, Tighiouart H, Novak V, Scott TM, Lou KV, et al. Anatomic brain disease in hemodialysis patients: a cross-sectional study. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2013;61(2):271–8.
Drew DA, Koo BB, Bhadelia R, Weiner DE, Duncan S, la Garza MMD, et al. White matter damage in maintenance hemodialysis patients: a diffusion tensor imaging study. BMC Nephrol. 2017;18(1):213.
Voineskos AN, Rajji TK, Lobaugh NJ, Miranda D, Shenton ME, Kennedy JL, et al. Age-related decline in white matter tract integrity and cognitive performance: a DTI tractography and structural equation modeling study. Neurobiol Aging. 2012;33(1):21–34.
Lau WL, Huisa BN, Fisher M. The cerebrovascular-chronic kidney disease connection: perspectives and mechanisms. Transl Stroke Res. 2017;8(1):67–76.
• Gupta A, Sarnak M, Montgomery R, Mahanken J, Lepping R, Brooks W, Burns J. Changes in cognition, cerebral blood flow and brain neurochemicals before and after kidney transplantation. Alzheimer's Association International Conference. 2019. This study demostrates change in brain blood flow and neurochemicals after kidney transplant indicating potenial reversibility of some of the brain alterations seen in kidney disease.
Kamano C, Komaba Y, Sakayori O, Iino Y, Katayama Y. Decreased cerebral blood flow in renal transplant recipients. Intern Med. 2002;41(9):677–83.
Michaelis T, Videen JS, Linsey MS, Ross BD. Dialysis and transplantation affect cerebral abnormalities of end-stage renal disease. J Magn Reson Imaging. 1996;6(2):341–7.
Tryc AB, Alwan G, Bokemeyer M, Goldbecker A, Hecker H, Haubitz M, et al. Cerebral metabolic alterations and cognitive dysfunction in chronic kidney disease. Nephrology Dialysis Transplantation. 2011;26(8):2635–41.
Haugen CE, Mountford A, Warsame F, Berkowitz R, Bae S, G. Thomas A, et al. Incidence, risk factors, and sequelae of post-kidney transplant delirium. Journal of the American Society of Nephrology : JASN. 2018;29(6):1752–9.
Fong TG, Davis D, Growdon ME, Albuquerque A, Inouye SK. The interface between delirium and dementia in elderly adults. The Lancet Neurology. 2015;14(8):823–32.
Aiello Bowles EJ, Larson EB, Pong RP, Walker RL, Anderson ML, Yu O, et al. Anesthesia exposure and risk of dementia and Alzheimer’s disease: a prospective study. J Am Geriatr Soc. 2016;64(3):602–7.
Wu L, Zhao H, Weng H, Ma D. Lasting effects of general anesthetics on the brain in the young and elderly: "mixed picture" of neurotoxicity, neuroprotection and cognitive impairment. J Anesth. 2019;33(2):321–35.
O’Brien H, O’Leary N, Scarlett S, O’Hare C, Kenny RA. Hospitalisation and surgery: are there hidden cognitive consequences? Evidence from The Irish Longitudinal study on Ageing (TILDA). Age Ageing. 2018;47(3):408–15.
Swarte JC, Douwes RM, Hu S, Vich Vila A, Eisenga MF, van Londen M, et al. Characteristics and Dysbiosis of the gut microbiome in renal transplant recipients. J Clin Med. 2020;9(2):386.
Song T, Rao Z, Tan Q, Qiu Y, Liu J, Huang Z, et al. Calcineurin inhibitors associated posterior reversible encephalopathy syndrome in solid organ transplantation: report of 2 cases and literature review. Medicine (Baltimore). 2016;95(14):e3173.
Wu Q, Marescaux C, Wolff V, Jeung MY, Kessler R, Lauer V, et al. Tacrolimus-associated posterior reversible encephalopathy syndrome after solid organ transplantation. Eur Neurol. 2010;64(3):169–77.
Stolp HB, Dziegielewska KM, Ek CJ, Potter AM, Saunders NR. Long-term changes in blood-brain barrier permeability and white matter following prolonged systemic inflammation in early development in the rat. Eur J Neurosci. 2005;22(11):2805–16.
Sakamoto Y, Makuuchi M, Harihara Y, Imamura H, Sato H. Higher intracerebral concentration of tacrolimus after intermittent than continuous administration to rats. Liver transplantation : official publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2001;7(12):1071–6.
Lanese DM, Conger JD. Effects of endothelin receptor antagonist on cyclosporine-induced vasoconstriction in isolated rat renal arterioles. J Clin Invest. 1993;91(5):2144–9.
Hirsch S, Reichold J, Schneider M, Székely G, Weber B. Topology and hemodynamics of the cortical cerebrovascular system. J Cereb Blood Flow Metab. 2012;32(6):952–67.
Snyder SH, Lai MM, Burnett PE. Immunophilins in the nervous system. Neuron. 1998;21(2):283–94.
Alonso A, Klink R. Differential electroresponsiveness of stellate and pyramidal-like cells of medial entorhinal cortex layer II. J Neurophysiol. 1993;70(1):128–43.
Koenigs M, Barbey AK, Postle BR, Grafman J. Superior parietal cortex is critical for the manipulation of information in working memory. J Neurosci. 2009;29(47):14980–6.
Yoon KH. Efficacy and cytokine modulating effects of tacrolimus in systemic lupus erythematosus: a review. J Biomed Biotechnol. 2010;2010:686480.
Rabinovitch A, Suarez-Pinzon W, Shapiro AMJ, Rajotte R, Power R. Combination therapy with sirolimus and interleukin-2 prevents spontaneous and recurrent autoimmune diabetes in NOD mice. Diabetes. 2002;51:638–45.
Keenan PA, Jacobson MW, Soleymani RM, Mayes MD, Stress ME, Yaldoo DT. The effect on memory of chronic prednisone treatment in patients with systemic disease. Neurology. 1996;47(6):1396–402.
Brown ES, Woolston DJ, Frol A, et al. Hippocampal volume, spectroscopy, cognition, and mood in patients receiving corticosteroid therapy. Biol Psychiatry. 2004;55(5):538–45.
Dixon BS, VanBuren JM, Rodrigue JR, et al. Cognitive changes associated with switching to frequent nocturnal hemodialysis or renal transplantation. BMC Nephrol. 2016;17:12.
Joshee P, Wood AG, Wood ER, Grunfeld EA. Meta-analysis of cognitive functioning in patients following kidney transplantation. Nephrol Dial Transplant. 2018;33(7):1268–77.
Gupta APT, Johnson D, Burns J. Sustained improvement in depression after renal transplantation: American Society of Nephrology Week; 2016.
Martinez-Sanchis S, Bernal MC, Montagud JV, et al. Effects of immunosuppressive drugs on the cognitive functioning of renal transplant recipients: a pilot study. J Clin Exp Neuropsychol. 2011;33(9):1016–24.
Harciarek M, Biedunkiewicz B, Lichodziejewska-Niemierko M, Debska-Slizien A, Rutkowski B. Continuous cognitive improvement 1 year following successful kidney transplant. Kidney Int. 2011;79(12):1353–60.
Castell JV, Geiger T, Gross V, et al. Plasma clearance, organ distribution and target cells of interleukin-6/hepatocyte-stimulating factor in the rat. Eur J Biochem. 1988;177(2):357–61.
• Chen HJ, Wen J, Qi R, et al. Re-establishing brain networks in patients with ESRD after successful kidney transplantation. Clinical journal of the American Society of Nephrology : CJASN. 2018;13(1):109–17 This paper demostrates reversibility of brain networks with a successful kidney transplant.
• Zhang LJ, Wen J, Liang X, et al. Brain default mode network changes after renal transplantation: a diffusion-tensor imaging and resting-state functional MR imaging study. Radiology. 2016;278(2):485–95 This study demostrates reversibility of diffusion tensor imaging and brain network alterations with a successful kidney transplant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Gupta reports grants from Novartis, Veloxis and NIH and consultancy from Novartis during the conduct of the study. None of these affects the work submitted by the authors.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Frailty and Gerontology
Rights and permissions
About this article
Cite this article
Jurgensen, A., Qannus, A.A. & Gupta, A. Cognitive Function in Kidney Transplantation. Curr Transpl Rep 7, 145–153 (2020). https://doi.org/10.1007/s40472-020-00284-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-020-00284-0