Abstract
Purpose of Review
We summarized data on the experience of people who withdraw from living kidney donation for non-medical reasons and suggest transplant centers strategies to enhance support for this population.
Recent Findings
Reported rates of opting out vary widely, from 0.2 to 22%. Individuals often describe more than one factor that contributed to their decision not to donate. Limited data suggests that most who withdraw from donation do not experience a long-term negative impact on their relationship with their intended recipient. For a minority, however, the decision to opt out may occasionally strain relationships and create significant emotional distress. Non-specific statements of ineligibility to donate may alleviate these complications, but they are rarely used.
Summary
The psychosocial impact of opting out of donation is complex and merits further research.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Simmons RG, Hickey K, Kjellstrand CM, Simmons RL. Family tension in the search for a kidney donor. JAMA. 1971;215(6):909–12.
Simmons RG, Marine SK, Simmons RL. Gift of life: the effect of organ transplantation on individual, family, and societal dynamics. New Brunswick, NJ: Transaction Publishers; 1987.
• Thiessen C, Kulkarni S, Reese PP, Gordon EJ. A call for research on individuals who opt out of living kidney donation: challenges and opportunities. Transplantation. 2016;100:2527–32. In this article, we argue that improving our understanding of opting out is important for the transplant community, offer suggestions for addressing the unique challenges of designing studies with this population, and delineate several avenues for future rearch on opting out.
Thiessen C, Iskander R, Kulkarni S. Support for individuals who opt out of living kidney donation: a survey of practices at US transplant centers. 2018 in press.
Organ procurement and transplantation network. National data. 2017; https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/. Accessed 1 Nov 2017.
Global Observatory on Donation and Transplantation. Global data. http://www.transplant-observatory.org/export-database/. Accessed 1 Nov 2017.
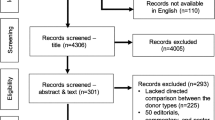
• Bailey PK, CRV T, MacNeill S, et al. A multicenter cohort study of potential living kidney donors provides predictors of living kidney donation and non-donation. Kidney Int. 2017;92(5):1249–60. This multi-center study offers an exceptionally detailed breakdown of the ultimate status (e.g. donor, withdrawal from donation, ineligible to donate) of 856 individuals beginning living kidney donor evaluation in the UK. The authors also present the first multivariable analysis of factors associated with the decision opt out of donation
AlBugami M, Asian G, Alotabie F, Bel'eed-Akkari K. Why are living kidney donors declined? Am J Transplant. 2016;16(S1):37.
Connaughton DM, Harmon G, Cooney A, et al. The Irish living kidney donor program - why potential donors do not proceed to live kidney donation? Clin Transpl. 2016;30(1):17–25.
Stewart Z. The majority of living kidney donor candidates fail to complete a full donor evaluation: the University of Iowa experience. Am J Transplant. 2014;14(S2):85–6.
Romagnoli J, Salerno MP, Calia R, Bianchi V, Pedroso JA, Spagnoletti G, et al. Expanding the living donor pool, “1st act”: analysis of the causes of exclusion of potential kidney donors. Transplant Proc. 2013;45(7):2632–4.
Garcia-Roca R, Choudhury N, Tzvetanov I, Jeon H, Oberholzer J, Benedetti E. Understanding racial disparity in living donor kidney transplantation. Am J Transplant. 2013;13(Supplement 5):190.
Perlis N, Connelly M, D'A Honey JR, Pace KT, Stewart R. Evaluating potential live-renal donors: causes for rejection, deferral and planned procedure type, a single-centre experience. Can Urol Assoc J. 2013;7(1–2):41–5.
Weng FL, Dhillon N, Lin Y, Mulgaonkar S, Patel AM. Racial differences in outcomes of the evaluation of potential live kidney donors: a retrospective cohort study. Am J Nephrol. 2012;35(5):409–15.
Veerappan I, Neelakantan N, Tamilarasi V, John GT. Medical and non-medical factors that affect voluntary living-related kidney donation: a single-center study. Indian J Nephrol. 2011;21(1):14–20.
Roodnat JI, van de Wetering J, Zuidema W, et al. Ethnically diverse populations and their participation in living kidney donation programs. Transplantation. 2010;89(10):1263–9.
Wafa EW, Donia AF, Ali-El-Dein B, et al. Evaluation and selection of potential live kidney donors. J Urol. 2004;171(4):1424–7.
Calder FR, Chang RW. Panning for gold: screening for potential live kidney donors. Nephrol Dial Transplant. 2004;19(5):1276–80.
Trevitt R, Whittaker C, Ball EA, FitzGerald L. Drop-out rate during living donor selection. EDTNA ERCA J. 2001;27(2):88–91.
Binet I, Bock AH, Vogelbach P, et al. Outcome in emotionally related living kidney donor transplantation. Nephrol Dial Transplant. 1997;12(9):1940–8.
Thiessen C, Gannon J, Gray D, et al. How potential living kidney donors (LKDs) view ESRD risk: a multi-center study. Am J Transplant. 2017;17(S3):791.
Thiessen C, Jaji Z, Joyce M, et al. Opting out: a single-centre pilot study assessing the reasons for and the psychosocial impact of withdrawing from living kidney donor evaluation. J Med Ethics. 2017;43(11):756–61.
Altobelli L. An altruistic living donor’s story. Narrat Inq Bioeth. 2012;2(1):7–10.
Franklin PM, Crombie AK. Live related renal transplantation: psychological, social, and cultural issues. Transplantation. 2003;76(8):1247–52.
Satel S. Desperately seeking a kidney. The New York Times 16 December, 2007.
• Bauman S. Surgery for the soul. Narrat Inq Bioeth. 2012;2(1):10-11 This entire issue of Narrative Inquiry in Bioethics is devoted to first-person accounts from living donors and family members of deceased donors.
Yu K, Thiessen C, Li S, et al. Potential living kidney donors (LKD) concerns about opting out and preference for an ‘alibi’. Am J Transplant. 2017;17(S3):807–8.
Fellner CH, Marshall JR. Kidney donors: the myth of informed consent. Amer J Psychiat. 1970;126(9):1245–51.
Simmerling M, Angelos P, Frader J, Franklin J, Leventhal J, Abecassis M. Primum non nocere: beneficient deception. DePaul L Rev. 2007;57:243–50.
Simmerling M, Frader J, Franklin J, Angelos P. When duties collide: beneficence and veracity in the evaluation of living organ donors. Curr Opin Organ Transplant. 2007;12(2):188–92.
Ross LF. What the medical excuse teaches us about the potential living donor as patient. Am J Transplant. 2010;10(4):731–6.
Spital A. Providing a medical excuse to organ donor candidates who feel trapped: concerns and replies. Camb Q Healthc Ethics. 2008;17:124–7.
Yu K, Kulkarni S, Gannon J, Reese P, Gordon E, Thiessen C. Attitudes toward living kidney transplantation among potential transplant candidates. Am J Transplant. 2016;16(S3):518.
Heath A. The essence of giving—a transplant story. Narrat Inq Bioeth. 2012;2(1):14–7.
Flynn J. Kidney donation story. Narrat Inq Bioeth. 2012;2(1):11–4.
Thiessen C, Kim YA, Formica R, Bia M, Kulkarni S. Opting out: confidentiality and availability of an 'alibi' for potential living kidney donors in the USA. J Med Ethics. 2015;41(7):506–10.
Organ procurement and transplantation network. Policy 14: living donation. 2017; https://optn.transplant.hrsa.gov/media/1200/optn_policies.pdf - nameddest=Policy_14, 2 November 2017.
Kulkarni S, Thiessen C, Formica RN, Schilsky M, Mulligan D, D'Aquila R. The long-term follow-up and support for living organ donors: a center-based initiative founded on developing a Community of Living Donors. Am J Transplant. 2016;16(12):3385–91.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Sanjay Kulkarni declares no conflict of interest.
Carrie Thiessen and Sanjay Kulkarni reports grants from Greenwall Foundation, outside the submitted work. Sanjay Kulkarni received an investigator-initiated grant from Alexion, outside the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Live Kidney Donation
Rights and permissions
About this article
Cite this article
Thiessen, C., Kulkarni, S. The Psychosocial Impact of Withdrawing from Living Kidney Donation. Curr Transpl Rep 5, 64–71 (2018). https://doi.org/10.1007/s40472-018-0185-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-018-0185-x