Abstract
Purpose of Review
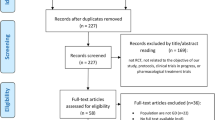
Cognitive behaviour therapy is the gold standard for the treatment of gambling disorder. Obstacles remain regarding its efficacy, namely relapses and difficulty in implementing cognitive restructuring for some clients. Given these observations, behavioural interventions for gambling disorder, such as exposure therapy, which aims to decrease gambling craving, may be effective as a complementary or alternative intervention to cognitive behaviour therapy. This systematic review and meta-analysis aims to explore how exposure therapy for gambling disorder has been studied and to evaluate its efficacy. To answer these questions, 3406 studies, retrieved using PsycNet, Medline and Google Scholar, were screened.
Recent Findings
After two screenings, 13 papers were selected for the systematic review and five were statistically combined for the meta-analysis. Quantitative results support exposure therapy’s efficacy to decrease gambling craving at post-intervention (g = − 0.955) and at last follow-up (6 or 12 months; − 1.010). Results also show a large decrease in gambling severity as documented by screening instruments (− 1.087) as well as time spent gambling (− 2.136) at post-intervention. Furthermore, a large decrease in gambling measured via screening instruments (− 1.162) and erroneous beliefs (− 1.308) was found at last follow-up.
Summary
This is the first meta-analysis on behavioural exposure therapy for gambling disorder. Results support that exposure therapy reduces gambling cravings and severity, as well as time spent gambling and erroneous beliefs. These results are discussed in comparison to other therapeutic approaches and are interpreted according to the high risk of bias in included studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gambling disorder (GD) is recognised as a persistent and recurrent problematic gambling behaviour leading to clinically significant impairment or distress [1]. To this day, cognitive behaviour therapy (CBT) is the most empirically validated treatment for GD [2•, 3]. CBT integrates behavioural interventions with aspects of cognitive therapy. It is used alone or in combination with motivational interventions. A recent systematic review of treatments for problem gambling found some benefits of CBT in the short term; only a few studies demonstrated long-term benefits [4].
Many problem gambling etiological models consider erroneous beliefs as a significant contributing factor in developing GD [5–8]. Given this contribution, it is natural that many CBT interventions include and may primarily rely on cognitive restructuring. Cognitive restructuring comprises both the identification of erroneous thoughts and the restructuring of those thoughts. The most used technique to identify erroneous beliefs is exposure to a gambling scenario [9•]. Cognitive therapy by itself could have no better benefits in the short or long term relative to an active control condition (exposure therapy) [4]
Recent addiction management literature [10, 11] also demonstrates that exposure to a gambling scenario may also be used as a stand-alone therapy. The rationale for exposure therapy is that by definition, addiction is a learned behaviour resulting from the coupling of substance use and pleasure, and can therefore be un-learned. In order to support the unlearning process, cue-exposure therapy presents individuals with relevant drug cues to extinguish the conditioned response [12–14]. This conceptualisation is based on learning theory, according to which drugs represent an unconditioned stimulus, and the effects are the unconditioned responses. By associative learning, neutral stimuli such as visual, olfactory, tactile and auditory cues can elicit a conditioned craving response, as these cues are frequently paired with drug use [13, 15, 16].
Exposure in the Gambling Literature
Exposure has taken different forms in gambling treatment, such as imaginal desensitisation and exposure with response prevention [17–20]. These variations of exposure therapy share the same core conceptualisation as cue-exposure therapy for addiction and can take the form of imaginal, in vivo or virtual reality exposure [21, 22]. Battersby et al. [21] use exposure therapy to specifically target gambling craving. Gambling craving can manifest as physical sensations such as heart palpitations or muscle tension, emotional states like stress and increased arousal, or as thoughts pertaining to different aspects of gambling (i.e. dreams of winning or negative flashbacks; [23]). To extinguish craving induced by gambling cues, Battersby et al. [21] use graded exposure where initial cues elicit less craving, thus making them easier to cope with and progressively become more challenging. Authors suggest that this type of graded exposure makes it easier for patients to concentrate on cravings elicited by the cue and experience a reduction of craving over time. It is expected that cravings will diminish over the course of therapy through a process called habituation.
To date, only one study has sought to summarise exposure therapy’s efficacy for the treatment of GD. In their 2008 narrative review, Dowling, Jackson and Thomas [18] concluded that exposure therapy appears to be a promising technique for the treatment of GD, yet requires further empirical evidence to confirm its efficacy. This review did not predetermine which outcome measures would be used to quantify exposure therapy’s efficacy in treating GD. Given the key role of craving in exposure therapy’s rationale [21], an investigation of exposure therapy should first establish its efficacy in lowering the craving to gamble. Dowling et al.’s [18] review included studies that contained data on perceived self-efficacy in controlling gambling behaviour [24] making it another important outcome to investigate. Perceived self-efficacy is defined as an individual’s belief in their ability to resist an opportunity to gamble in a given situation [25, 26]. A systematic review by Chrétien et al. [9•] found that reported gambling behaviour (i.e. the amount of time and money spent gambling) and severity of problem gambling measured with screening instruments were the most commonly documented efficacy variables in GD therapy studies. Lastly, erroneous beliefs are often documented in GD intervention studies [9•], as they are believed to be central to GD aetiology and maintenance [5–7]. Documenting exposure therapy’s efficacy in lowering erroneous beliefs will provide a way to contrast its efficacy to other therapeutic approaches.
Objectives
The main objective of this systematic review and meta-analysis was to document the use of exposure therapy as a behavioural treatment of GD and to evaluate its efficacy. To do so, the current study sought to determine to what extent exposure therapy reduces: (1) gambling craving; (2) severity of problem gambling; (3) gambling behaviour; (4) erroneous beliefs; and (5) increases perceived self-efficacy.
Method
Protocol
This systematic review and meta-analysis was conducted according to the recommendations outlined in the Cochrane Handboock for Systematic Reviews of Interventions [27]. Findings were reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [28].
Search Strategy
In order to be included in the meta-analysis, potential studies must have (1) an exposure therapy condition; (2) one or more of the following measurements: severity of GD, gambling behaviours (money spent, time spent, etc.), craving intensity and perceived self-efficacy; (3) data for pathological or at-risk gamblers according to a screening instrument or clinical interview; (4) been written in French or English; and (5) been published since 1980, year of the introduction of pathological gambling in the DSM-III. Studies that documented the efficacy of CBT programs with exposure therapy as one of the treatment components were excluded.
A three-step systematic review of the literature was conducted to identify relevant studies. First, the electronic databases PsychNET (via APA), MEDLINE (via PubMed) and Google Scholar were screened up to July 1st, 2019. For PsychNET and Google Scholar, the following search equation was used: {exposure OR virtual reality OR imaginal desensitization OR imaginal relaxation OR “in vivo”} AND {gambl*} in any field and index terms. For Medline, the following search strategy was used: {exposure therapy OR Virtual Reality Exposure Therapy OR Desensitization, Psychologic} AND {gambl*} where the first part of the criteria was in MESH terms. These strategies were developed with the help of a specialised social sciences librarian. The reference lists of selected articles were also retrieved from the databases to identify other potential eligible studies. Lastly, authors of selected studies were contacted by e-mail to inquire about unpublished data. No paper was added to the screening by the use of the last two strategies.
Study Selection
First, study eligibility was determined by reading article titles and abstracts. For the first step of article screening, interrater agreement between the first author and a graduate research assistant was based on a random sample of 10% of the studies. The first author carried out the rest of the screening. Studies that passed the initial screening were then read in their entirety. For this second selection, interrater agreement was based on the full-sample and carried out by the first author and an undergraduate research assistant. Disagreements were settled by consensus.
Data Extraction
As suggested by the Cochrane Collaboration [27], a data extraction form was developed to gather all relevant study information. The data extraction form included information on authors, methodology (experimental design, condition assignment), participant characteristics, outcome measures and results. A double data entry was carried out by the first author and a trained undergraduate research assistant. Disagreements were settled by consensus.
Assessment of Risk of Bias in Included Studies
In accordance with the Cochrane Risk of Bias assessment tool [27], each of the following study’s risk of bias was rated “High”, “Low” or “Unclear”: random sequence generation (selection bias); allocation concealment (selection bias); blinding of participants, personnel and outcome assessors (detection bias); incomplete outcome data (attrition bias); selective outcome reporting (reporting bias); and other potential threats to validity (see [28] for a complete description).
Outcome Measures
Gambling craving was the primary outcome variable in this study. Secondary outcome variables included the time and money spent gambling, the frequency of gambling, GD screening scores and erroneous beliefs and perceived self-efficacy measured with validated self-report questionnaires.
Unit of Analysis
Analyses compared data for a number of outcome variables from baseline to post-intervention and last follow-up using Hedges’ g as the measure of effect [29, 30]. Hedges’ g provides a standardized mean difference with a correction for small sample size and is interpreted as a z score, where the output represents the number of pooled standard differences between two timepoints [29, 31]. In the present study, a negative Hedges’ g indicates a decrease in the given variable at post-intervention or last follow-up. Hedges’ g is interpreted similarly to Cohen’s d, where 0.2, 0.5 and 0.8 represent small, medium and large effects, respectively [29, 32]. Effect sizes were calculated using Biostat software Comprehensive Meta-analysis (Biostat Inc., Engelwood, NJ) using timepoint means, standard deviations and pre-post-correlation estimates for each variable. Pre-post-correlation estimates were calculated using data from other gambling clinical studies [33, 34]. Forest plots were also calculated according to these analyses, including Hedges’s g, variance and global effect size for each variable according to a random measure effect with a 95% confidence interval.
Results
Descriptive Data Analysis
Sample
As shown in Fig. 1, 3406 publications were initially screened, and from those, 3393 were excluded. Most of these articles were excluded because they did not include exposure therapy. Interrater agreement reached 95.1% for the screening and 99% for the full sample. Thirteen articles were retained for the final sample.Footnote 1 Even though four were single-case studies and one had only two participants, these studies are included in the study descriptive as they provide input on how exposure therapy has been used on gambling treatment. The meta-analysis therefore includes six studies.
From 13 selected studies, 948 participants were allocated to an exposure condition. Excluding single-case studies [36, 39, 42, 47], the mean number of participants was 104.9 (SD = 104.1, median = 49). Participants from 12 studies [34,35,36,37,38,39, 41,42,43, 44••, 45, 46••] reported gambling mostly or exclusively on electronic gambling machines, while the majority of participants in the remaining study [40] bet on horse races.
Eight of the included studies provided baseline descriptive data on time spent gambling [34, 36,37,38,39, 43, 44••, 47] and four on money spent on gambling[34, 37,38,39]. Participants in these studies spent an average of 6.9 h per week (SD = 2.2, min = 3.8, max = 12.8) gambling and had spent an average of $441.40 USD per week on gambling (SD = 455.30, median = 150). Table 1 provides data on participant characteristics, study localisation as well as included studies referencing number for the current article.
Intervention
Nine studies were carried out in outpatient settings [34, 35, 37,38,39, 42, 43, 44••, 45, 46••], three in inpatient settings [36, 40, 41] and one study did not specify the context of treatment [47]. Three studies used in vivo exposure [37,38,39], three imaginal exposure [34, 35, 40] and seven used a mix of both techniques [36, 41,42,43, 44••, 45, 46••, 47]. Six of the seven studies using both imaginal and in vivo exposure included a gradual increase in difficulty by first using imaginal exposure and then in vivo exposure [36, 42, 43, 44••, 45, 46••, 47]. Participants met with a therapist 7.4 times on average (median = 9.5) and took part in an average of 23.1 exposure sessions (either with the therapist or as betweensession homework; SD = 19.9, median = 14). Table 2 provides characteristics of the exposure session for each study.
Theory and Learning Processes Behind Exposure Therapy
Five studies considered habituation to be the mechanism of action of the intervention [36, 42, 43, 44••, 45, 47]. One study aimed to lower gambling behaviour and craving, a definition considered similar to habituation for the current review [37]. Two studies involved altering the behaviour completion mechanism such that participants would no longer feel compelled to gamble in a gambling environment [40, 41]. One study [38] aimed to increase participants’ perceived self-efficacy through craving resistance. The remaining studies did not describe their intervention’s mechanism of action [34, 35, 39, 46••]
Outcome Variables
The most common outcome variables were time spent gambling at post-intervention [34, 36, 39, 43, 44••, 46••]; gambling craving using the Gambling Urge Scale [48; 45, 46••], visual analogue scale [34, 35] or categorical scale [40]; erroneous beliefs using the Gambling-Related Cognitions Scale [49; 36, 45, 46••] and the Gambling Beliefs Questionnaire [50; 35]; and subjective indicators [37,38,39, 47]. Studies also used three GD screening instruments: three used the Victorian Gambling Screen [VGS; 51; 36, 45, 46••], three used the South Oaks Gambling Screen [SOGS; 52; 42, 43, 44••, 47] and one used the Canadian Problem Gambling Index [53; 36]. Table 3 provides a detailed account of the gambling related outcomes for the selected studies.
Risk of Bias in Selected Studies
Risk of bias of the included studies is presented in Table 4. The studies included in this review had a high risk of bias due to the lack of blinding of study personnel, random sequence generation and allocation concealment.
Meta-analyses
Four variables were analysed at post-treatment and at the longest available follow-up. Five studies [35, 37, 39, 47] had too few participants (≤ 2) and therefore could not be statistically combined for Hedges’ g. One study [38] combined outcome variables in the Inadaptation Scale [54], making it impossible to include them in analyses. Two more studies [40, 41] also contained selected outcome variables measured categorically and were thereby unable to be pooled with the continuous data from the other studies. For studies included in the meta-analyses [34, 37, 43, 44••, 45], last follow-up is either 6 [46••] or 12 months [34, 37, 45]. No analysis could be carried out on perceived self-efficacy, as only one study had enough participants for this outcome.
Figure 2 shows the forest plot for each analysis according to a random effects model with 95% confidence interval. Included variables pertained to gambling craving, GD screening instruments, time spent gambling and erroneous beliefs.
Craving
Three studies were included in the analyses of exposure therapy’s impact on craving post-treatment [34, 45, 46••]. Pooled results show a decrease in mean Gambling Urge Scale [32] and visual analogue scale scores from 12.31 (sdpooled = 6.49) to 8.17 (sdpooled = 6.12). This decrease is equivalent to a Hedge’s g of − 0.955 (CI = [− 1.78, − 0.13]), p = 0.024, corresponding to a large effect [29, 32].
Two studies were included in the analyses of exposure therapy’s impact on craving at last measure [45, 46••]. Pooled mean scores on the Gambling Urge Scale [48] decreased from 13.71 (sdpooled = 7.32) to 2.89 (sdpooled = 10.21) at last measure. This decrease is equivalent to a Hedge’s g of − 1.010 (CI = [− 1.51, − 0.51]), p < 0,001, corresponding to a large effect [29, 31, 32].
GD Screening Instruments
Three studies totalling four groups [44••, 45, 46••] were included in the analysis of exposure therapy’s impact on GD screening instruments at post-intervention. SOGS pooled average scores decreased from 9.57 (sdpooled = 4.33) to 4.01 (sdpooled = 4.37) in two groups [44••] and VGS pooled scores decreased from 38.14 (sdpooled = 10.87) to 29.13 (sdpooled = 10.01) at post-intervention for the two other groups [45, 46••]. Hedges’ g was − 1.09 (CI = − 1.54, − 0.64), p < 0.001, corresponding to a large effect [29, 32].
Given that the two groups [44••] documenting SOGS score did not have follow-up measures, VGS score in the two remaining studies [45, 46••] represents GD screening instrument scores for the last measure. Pooled VGS scores decreased from 38.14 (sdpooled = 10.87) to 15.83 (sdpooled = 16.33) at last measure, equivalent to a Hedge’s g of − 1.69 (CI = [− 2.750, − 0.63]), p = 0.002, which indicates a large effect [29, 32].
Time Spent Gambling
Four studies (totalling five groups; 1R, 4R, 10R, 11R, 13R) were included in the analysis of exposure therapy’s impact on time spent gambling at post intervention. The average hours spent gambling per month decreased from 18.51 (sdpooled = 6.52) to 3.21 (sdpooled = 4.33) h post-treatment. A large effect was observed for this outcome with a Hedge’s g of − 2.16 (CI = [− 3.05, − 1.27), p < 0.001 [29, 32].
Two studies were included in the analysis of exposure therapy’s impact on time spent gambling at last measure [39, 46••]. Mean hours spent gambling per month fell from 18.02 (sdpooled = 8.05) to 2.90 (sdpooled = 2.72). Hedge’s g was non-significant, − 2.45 (CI = [− 5.34, 0.44]), p = 0.096.
Erroneous Beliefs
Two studies were included in the analyses of exposure therapy’s impact on erroneous beliefs at post intervention [45, 46••]. Pooled mean Gambling Related Cognitions Scale [49] scores decreased from 68 (sdpooled = 21.5) to 55.4 (sdpooled = 19.5) which was also non-significant, Hedge’s g = − 0.65 (CI = [− 1.34, 0.04]), p = 0.064.
Two studies were included in the analyses of exposure therapy’s impact on erroneous beliefs at last measure [45, 46••]. Pooled Gambling Related Cognitions Scale [48] mean scores decreased from 68 (sdpooled = 21.5) to 34.15 (sdpooled = 25.14). A large effect was observed for this measure, Hedge’s g = − 1.31 (CI = [− 2.00, − 0.62]), p < 0.001 [29, 32].
Table 5 summarises data relating to quantitative analyses for each outcome.
Discussion
This systematic review and meta-analysis aimed to describe how exposure therapy is implemented in the treatment of GD, as well as its efficacy in reducing cravings, gambling behaviour and screening test scores, as well as decreasing erroneous beliefs and improving perceived self-efficacy.
Studies Description
To date, exposure therapy for GD has been most widely studied in predominantly male participants, with more recent studies striving to include more women in their samples. Exposure therapy for GD was studied in two countries, Australia and Spain, and participants mainly preferred electronic gambling machines. Participants were mostly seen individually and in outpatient settings.
Most studies presented a mix of imaginal and in vivo exposure with exposure intensity gradually progressing as participants became increasingly capable of successfully confronting each cue. Most exposure therapy studies were theoretically based on habituation, such that exposure to different gambling cues induces craving, yet as the craving is not acted upon, it decreases and would ultimately be extinguished. This rationale is akin to systematic desensitisation as originally developed in the 1950s [55].
Only three studies had therapeutic mechanisms other than habituation. McConaghy et al.’s studies [40, 41] conceptualise exposure therapy as a means of altering the behaviour completion mechanism, leading patients to no longer feel compelled to gamble in a gambling environment. McConaghy et al. (1988) [40] conclude that it is not possible to determine if the behaviour completion mechanism better explains exposure therapy’s efficacy. Echeburúa el al. [38] conceptualise that exposure therapy raises perceived self-efficacy to not gamble when faced with gambling situations. This conceptualisation resembles that of more recent inhibitory learning views of exposure therapy for anxiety [56]. According to this model, exposure does not produce the unlearning between a cue and a conditioned response but rather produces a new learning that inhibits the conditioned response. Combining this conceptualisation to Echeburúa et al.’s (2000) [38], craving would be the conditioned response and increased self-efficacy would be the new learning brought about by exposure, which would in turn reduce the craving to gamble. Given that this conceptualisation has yet to be applied to GD, future studies in line with this understanding would further clarify how exposure therapy works, while potentially providing a treatment description that better reflects participants’ subjective experience.
Last of all, the analysis of selected studies shows a high risk of bias as a result of insufficient blinding of study personnel, random sequence generation and allocation concealment. Moreover, only two to three studies conducted in Spain and Australia could be included in each meta-analysis. This highlights the necessity for more methodologically sound studies to evaluate exposure therapy for GD in order to better ascertain its efficacy.
Exposure Therapy’s Efficacy
Exposure therapy had a large effect on craving reduction at post intervention and was even larger at 6- and 12-month follow-up. Confidence intervals were also closer to the corresponding g measure, indicating that results are more homogenous at follow-up. These results from the limited literature on exposure therapy support its efficacy in lowering gambling cravings. The effect of exposure therapy was larger at follow-up, which is similar to other studies of CBT [see 57]. Improved results at follow-up may be attributable to participants’ continued application of techniques learned in therapy; however, this has yet to be empirically tested. It is important to mention that one study did not include follow-up data on gambling craving, which may explain the more homogenous results and higher effect size data. Overall, it is surprising that only five of the 13 studies tested exposure therapy’s effect on reducing craving, given this variable’s crucial importance to treatment rationale.
From a statistical viewpoint, a large decrease of gambling screening instruments score was attained at post-treatment. Using SOGS’s cut-off scores, pooled means decreased from “probable pathological gambler” to “potential pathological gambler”. Using VGS cut-off scores, pooled mean results decreased at post-intervention while remaining in the “problem gambler” range. For final follow-up, pooled mean results indicate a score of “borderline gambling”. These large decreases remain lower than what was obtained from CBT in comparison to control in Cowlishaw et al.’s (2012) meta-analysis [2•]. Looking at other therapies investigated in the same meta-analysis, exposure therapy’s efficacy to lower participants gambling screening scores indicate that it is the next best intervention to reduce GD severity. This result is preliminary as it was derived from only a few studies with a high risk of bias. Nevertheless, these preliminary results are encouraging and support the efficacy of exposure therapy to reduce the severity of gambling behaviour.
Results show that exposure therapy produces a substantial decrease in time spent gambling at post-intervention, yet these results became non-significant at 6 to 12 months post-intervention. Given that confidence intervals were particularly large at last follow-up, the loss of significance may be attributable to the larger variance resulting from a small number of combined studies comprising few participants. Further studies with larger sample sizes are likely required to detect statistical significance. Still, Echeburúa et al. (2000) [38] have argued that adding relapse prevention after exposure therapy produces more therapeutic success than exposure therapy alone after 12 months. The effect of supplementing exposure therapy with relapse prevention should therefore also be studied in order to establish its added value.
Meta-analysis of two studies shows that exposure therapy resulted in a non-significant decrease in participants’ erroneous beliefs at post-intervention, yet showed a large and significant effect at 6 and 12 months. These results appear in line with past studies suggesting that higher levels of erroneous beliefs are associated to with higher levels of problem gambling severity [34, 58, 59]. Further studies evaluating the impact of exposure therapy, a behaviour intervention, on erroneous beliefs will be necessary to better understand the exact mechanism driving the effect.
Limits and Strengths
This meta-analysis was limited by the studies included for analyses as these were few, at high risk of bias, and performed in only two countries (Australian and Spain). The literature search did not identify any randomised controlled trials (RCTs). In comparison, Cowlishaw et al. (2012) [2•], who evaluated GD therapies including CBT, motivational interviewing therapy, integrative therapy and other psychotherapeutic interventions, found 14 RCTs. It is difficult to determine why exposure therapy has yet to be tested with a RCT design, but it is encouraging to see that 30% of the included studies used an empirical design with a lower risk of bias [44••, 45, 46••]. Another limitation of this study is that studies were included regardless of their risk of bias due to the small number of studies meeting the inclusion criteria. It was therefore necessary to combine this small number of studies while remaining critical of results in order to ascertain the pertinence of investigating exposure therapy’s efficacy for GD in future studies. Furthermore, the current meta-analysis used pre-post analyses within-participants due to the lack of studies involving a control group; the pre-post design is known to overestimate effect sizes in comparison to those computed from controlled studies [30]. The rigorous study selection, with two independent interrater agreements and double selection of data from selected studies, is the main strength of the study. It is hoped that findings from the present study showing the benefits of exposure therapy for GD will promote further, more methodologically rigorous studies in order to reliably establish exposure therapy’s efficacy for treating GD.
Conclusion
This study is the first meta-analysis on behavioural exposure therapy for GD. Pooled results from a small number of studies demonstrate a positive effect of exposure therapy for GD. The present study’s results show that exposure therapy reduces gambling cravings and severity, as well as time spent gambling and erroneous beliefs. Future studies should investigate the efficacy of standardized exposure therapy using a treatment manual in RCTs to obtain more reliable outcome data. Evaluating by which process exposure therapy leads to clinical efficacy would also help in understanding the link between each efficacy variable. Overall, this study supports exposure therapy as a promising approach to the treatment of GD and may assist in broadening therapeutic options for individuals suffering from GD.
Data Availability
Data may be obtained via request.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Fifth ed. Arlington, VA: American Psychiatric Publishing; 2013.
• Cowlishaw S, Merkouris S, Dowling N, Anderson C, Jackson A, Thomas S. Psychological therapies for pathological and problem gambling. Cochrane Database Syst Rev. 2012;(11). https://doi.org/10.1002/14651858.CD008937.pub2. This meta-analysis is the basis of comparison gambling disorder’s gold standard intervention, cognitive behaviour therapy.
Gooding P, Tarrier N. A systematic review and meta-analysis of cognitive-behavioural interventions to reduce problem gambling: hedging our bets? Behav Res Ther. 2009;47(7):592–607.
Petry NM, Ginley MK, Rash CJ. A systematic review of treatments for problem gambling. Psychol Addict Behav. 2017;31(8):951. https://doi.org/10.1037/adb0000290.
Fortune EE, Goodie AS. Cognitive distortions as a component and treatment focus of pathological gambling: a review. Psychol Addict Behav. 2012;26(2):298. https://doi.org/10.1037/a0026422.
Gaboury A, Ladouceur R. Erroneous perceptions and gambling. J Soc Behav Pers. 1989;4(4):411–20.
Sharpe L. A reformulated cognitive–behavioral model of problem gambling: a biopsychosocial perspective. Clin Psychol Rev. 2002;22(1):1–25. https://doi.org/10.1016/S0272-7358(00)00087-8.
Blaszczynski A, Nower L. A pathways model of problem and pathological gambling. Addiction. 2002;97(5):487–99. https://doi.org/10.1046/j.1360-0443.2002.00015.x.
• Chrétien M, Giroux I, Goulet A, Jacques C, Bouchard S. Cognitive restructuring of gambling-related thoughts: a systematic review. Addict Behav. 2017;75:108–21. https://doi.org/10.1016/j.addbeh.2017.07.001. This systematic review highlights several gambling disorder therapy’s pertinent efficacy indicators. It influenced selected outcome variables for the current meta-analysis.
Mellentin AI, Skøt L, Nielsen B, Schippers GM, Nielsen AS, Stenager E, et al. Cue exposure therapy for the treatment of alcohol use disorders: a meta-analytic review. Clin Psychol Rev. 2017;57:195–207. https://doi.org/10.1016/j.cpr.2017.07.006.
Trahan MH, Maynard BR, Smith KS, Farina AS, Khoo YM. Virtual reality exposure therapy on alcohol and nicotine: a systematic review. Res Soc Work Pract. 2019;29(8):876–91. https://doi.org/10.1177/1049731518823073.
Conklin CA, Tiffany ST. Cue-exposure treatment: time for change. Addiction. 2002;97(9):1219–21. https://doi.org/10.1046/j.1360-0443.2002.00205.x.
Drummond DC, Cooper T, Glautier SP. Conditioned learning in alcohol dependence: implications for cue exposure treatment. Br J Addict. 1990;85(6):725–43. https://doi.org/10.1111/j.1360-0443.1990.tb01685.x.
Marlatt GA. Cue exposure and relapse prevention in the treatment of addictive behaviors. Addict Behav. 1990;15(4):395–9. https://doi.org/10.1016/0306-4603(90)90048-3.
Everitt BJ, Robbins TW. Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat Neurosci. 2005;8(11):1481–9. https://doi.org/10.1038/nn1579.
Pavlov IP, e Anrep GV. Conditioned reflexes: Courier Corporation. 2003.
Bouchard S, Loranger C, Robillard G, Fournier P-M, Fortin-Gagnon É, Jacques C, et al. Guide d’utilisation des environnements virtuels pour les problèmes de jeu pathologique (version 2.0). Gatineau, Qc: Laboratoire de Cyberpsychologie de l’UQO; 2013.
Dowling N, Jackson AC, Thomas SA. Behavioral interventions in the treatment of pathological gambling: a review of activity scheduling and desensitization. Int J Behav Consult Ther. 2008;4(2):172. https://doi.org/10.1037/h0100841.
McConaghy N, Armstrong MS, Blaszczynski A, Allcock C. Controlled comparison of aversive therapy and imaginal desensitization in compulsive gambling. Br J Psychiatry. 1983;142(4):366–72. https://doi.org/10.1192/bjp.142.4.366.
Park CB, Park SM, Gwak AR, Sohn BK, Lee JY, Jung HY, et al. The effect of repeated exposure to virtual gambling cues on the urge to gamble. Addict Behav. 2015;41:61–4. https://doi.org/10.1016/j.addbeh.2014.09.027.
Battersby M, Oakes J, Tolchard B, Forbes A, Pols R. Cognitive behavioral therapy for problem gamblers. In: In the pursuit of winning. US: Springer; 2008. p. 179–97. https://doi.org/10.1007/978-0-387-72173-6_11.
Bouchard S, Robillard G, Giroux I, Jacques C, Loranger C, St-Pierre M, et al. Using virtual reality in the treatment of gambling disorder: the development of a new tool for cognitive behavior therapy. Front Psychiatry. 2017;8:27. https://doi.org/10.3389/fpsyt.2017.00027.
Morasco BJ, Weinstock J, Ledgerwood DM, Petry NM. Psychological factors that promote and inhibit pathological gambling. Cogn Behav Pract. 2007;14(2):208–17. https://doi.org/10.1016/j.cbpra.2006.02.005.
Symes BA, Nicki RM. A preliminary consideration of cue-exposure, response-prevention treatment for pathological gambling behaviour: two case studies. J Gambl Stud. 1997;13(2):145–57. https://doi.org/10.1023/A:1024951301959.
Casey LM, Oei TP, Melville KM, Bourke E, Newcombe PA. Measuring self-efficacy in gambling: the gambling refusal self-efficacy questionnaire. J Gambl Stud. 2008;24(2):229–46. https://doi.org/10.1007/s10899-007-9076-2.
Oei TP, Hasking PA, Young RM. Drinking refusal self-efficacy questionnaire-revised (DRSEQ-R): a new factor structure with confirmatory factor analysis. Drug Alcohol Depend. 2005;78(3):297–307. https://doi.org/10.1016/j.drugalcdep.2004.11.010.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions version 6.0 (updated July 2019). Cochrane; 2019. Retrieved June 24, 2020, from http://www.training.cochrane.org/handbook.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. https://doi.org/10.1371/journal.pmed1000097.
Hedges LV. Distribution theory for Glass’s estimator of effect size and related estimators. J Educ Stat. 1981;6(2):107–28. https://doi.org/10.2307/1164588.
Borenstein M, Hedges LV, Higgins JP, Rothstein HR. Introduction to meta-analysis. John Wiley & Sons; 2011.
Glen S. Hedges’ g: definition, formula. 2016. Retrieved June 24, 2020, from https://www.statisticshowto.com/hedges-g/.
Cohen J. Statistical power analysis for the behavioral sciences. 1977.
Sylvain C, Ladouceur R, Boisvert J-M. Cognitive and behavioral treatment of pathological gambling: a controlled study. J Consult Clin Psychol. 1997;65(5):727–32. https://doi.org/10.1037/0022-006X.65.5.727.
Blaszczynski A, Drobny J, Steel Z. Home-based imaginal desensitisation in pathological gambling: short-term outcomes. Behav Chang. 2005;22(01):13–21. https://doi.org/10.1375/bech.22.1.13.66782.
Blaszczynski A, Ladouceur R, Nower L, Sharpe L. Comparing changes in erroneous beliefs/perceptions, subjective arousal and heart rate between cognitive therapy and imaginal desensitization in the treatment of pathological gambling. 2003.
Dham P, Larsen A, Baigent M. Exposure based therapy for problem gambling in a patient with Alzheimer’s dementia. Australasian Psychiatr. 2015;23(5):510–2. https://doi.org/10.1177/1039856215598868.
Echeburúa E, Báez C, Fernández-Montalvo J. Comparative effectiveness of three therapeutic modalities in the psychological treatment of pathological gambling: long-term outcome. Behav Cogn Psychother. 1996;24(1):51–72. https://doi.org/10.1017/S1352465800016830.
Echeburúa E, Fernández-Montalvo J, Báez C. Relapse prevention in the treatment of slot-machine pathological gambling: long-term outcome. Behav Ther. 2000;31(2):351–64. https://doi.org/10.1016/S0005-7894(00)80019-2.
Echeburúa E, Fernández-Montalvo J. Psychological treatment of slot machine pathological gambling: a case study. Clin Case Stud. 2002;1(3):240–53. https://doi.org/10.1177/15350102001003004.
McConaghy N, Armstrong MS, Blaszczynski A, Allcock C. Behavior completion versus stimulus control in compulsive gambling: implications for behavioral assessment. Behav Modif. 1988;12(3):371–84. https://doi.org/10.1177/01454455880123004.
McConaghy N, Blaszczynski A, Frankova A. Comparison of imaginal desensitisation with other behavioural treatments of pathological gambling. A two-to nine-year follow-up. Br J Psychiatry. 1991;159(3):390–3. https://doi.org/10.1192/bjp.159.3.390.
Oakes J, Battersby MW, Pols RG, Cromarty P. Exposure therapy for problem gambling via videoconferencing: a case report. J Gambl Stud. 2008;24(1):107. https://doi.org/10.1007/s10899-007-9074-4.
Riley B, Smith D, Oakes J. Exposure therapy for problem gambling in rural communities: a program model and early outcomes. Aust J Rural Health. 2011;19(3):142–6. https://doi.org/10.1111/j.1440-1584.2011.01199.x. [Metropolian group]
•• Riley B, Smith D, Oakes J. Exposure therapy for problem gambling in rural communities: a program model and early outcomes. Aust J Rural Health. 2011;19(3):142–6. https://doi.org/10.1111/j.1440-1584.2011.01199.x. [Rural group]. This community study comparing the same therapy in two communities has the largest sample using exposure therapy. The application of the protocol in clinical settings provides confidence in its application with diverse clinical presentations.
Smith D, Harvey P, Battersby M, Pols R, Oakes J, Baigent M. Treatment outcomes and predictors of drop out for problem gamblers in South Australia: a cohort study. Aust N Z J Psychiatry. 2010;44(10):911–20. https://doi.org/10.3109/00048674.2010.493502.
•• Smith DP, Battersby MW, Harvey PW, Pols RG, Ladouceur R. Cognitive versus exposure therapy for problem gambling: randomised controlled trial. Behav Res Ther. 2015;69:100–10. https://doi.org/10.1016/j.brat.2015.04.008. This randomized trial gives a detailed and rigorous appreciation of its protocol and analysis while describing every step of exposure therapy. It also documents exposure therapy’s impact on several pertinent variables.
Tolchard B, Thomas L, Battersby M. Single-session exposure therapy for problem gambling: a single-case experimental design. Behav Chang. 2006;23(2):148–55. https://doi.org/10.1375/bech.23.2.148.
Raylu N, Oei TP. The gambling urge scale: development, confirmatory factor validation, and psychometric properties. Psychol Addict Behav. 2004a;18(2):100. https://doi.org/10.1037/0893-164X.18.2.100.
Raylu N, Oei TP. The gambling related cognitions scale (GRCS): development, confirmatory factor validation and psychometric properties. Addiction. 2004b;99(6):757–69. https://doi.org/10.1111/j.1360-0443.2004.00753.x.
Joukhador J, Blaszczynski A, Maccallum F. Superstitious beliefs in gambling among problem and non-problem gamblers: preliminary data. J Gambl Stud. 2004;20(2):171–80. https://doi.org/10.1023/B:JOGS.0000022308.27774.2b.
Tolchard B, Battersby MW. The Victorian gambling screen: reliability and validation in a clinical population. J Gambl Stud. 2010;26(4):623–38. https://doi.org/10.1375/bech.23.2.148.
Lesieur HR, Blume SB. The south oaks gambling screen (SOGS): a new instrument for the identification of pathological gamblers. Am J Psychiatr. 1987;144(9). https://doi.org/10.1176/ajp.144.9.1184.
Ferris JA, Wynne HJ. The Canadian problem gambling index. Ottawa, ON: Canadian Centre on Substance Abuse; 2001. p. 1–59.
Echeburúa E, Corral P. Escala de inadaptación [Inadaptation scale]. Unpublished manuscript; 1987.
Wolpe J. Reciprocal inhibition therapy. 1958.
Craske MG, Treanor M, Conway CC, Zbozinek T, Vervliet B. Maximizing exposure therapy: an inhibitory learning approach. Behav Res Ther. 2014;58:10–23. https://doi.org/10.1016/j.brat.2014.04.006.
Carlbring P, Jonsson J, Josephson H, Forsberg L. Motivational interviewing versus cognitive behavioral group therapy in the treatment of problem and pathological gambling: a randomized controlled trial. Cogn Behav Ther. 2010;39(2):92–103. https://doi.org/10.1080/16506070903190245.
Lévesque D, Sévigny S, Giroux I, Jacques C. Psychological vulnerability and problem gambling: the Mediational role of cognitive distortions. J Gambl Stud. 2018;34(3):807–22. https://doi.org/10.1007/s10899-017-9740-0.
Oei TPS, Lin J, Raylu N. The relationship between gambling cognitions, psychological states, and gambling: a cross-cultural study of Chinese and Caucasians in Australia. J Cross-Cult Psychol. 2008;39(2):147–61.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
Waived by the comité d’éthique de la recherche en psychologie et en sciences de l’éducation de l’Université Laval on 20/04/2018.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
Stéphane Bouchard is president of, and owns shares in, Cliniques et Développement In Virtuo, a company that distributes virtual environments, and any conflict of interest is managed under UQO’s conflict of interest policy. The other authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Gambling
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bergeron, PY., Giroux, I., Chrétien, M. et al. Exposure Therapy for Gambling Disorder: Systematic Review and Meta-analysis. Curr Addict Rep 9, 179–194 (2022). https://doi.org/10.1007/s40429-022-00428-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-022-00428-5