Abstract
Purpose
Dental bleaching in paediatric patients can be used to address discolouration of teeth due to trauma, endodontic treatment, or enamel and dentine defects. Despite being a minimally invasive and successful treatment, the use of bleaching products in children and young people remains controversial. This evaluation was designed to provide insight into the child’s perspective on dental bleaching and the influence that this treatment has upon their life.
Method
A dental bleaching patient reported outcome measure (PROM) was developed and piloted in 2019. Data were collected from 3 UK units (January–March 2020). Children attending these units for bleaching reviews were invited to complete the PROM.
Results
Twenty seven PROM questionnaires were completed including 19 courses of external bleaching and 8 courses of internal/external bleaching. The average age was 14 years old (9–17 years). The common indications for bleaching were Amelogenesis Imperfecta, dental trauma and Molar Incisor Hypomineralisation. Patients reported improvements in their appearance (89%) and self-confidence (81%). Sensitivity was the most common side effect, reported in 63% of cases.
Conclusion
This PROM supports the use of dental bleaching in children and young people when treating dental disease that causes discolouration. Bleaching not only improved the appearance of teeth, but also patients’ self-confidence. Sensitivity is a common side effect and clinicians should discuss this common risk and its management with patients and their families.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In paediatric patients, discolouration of teeth is caused by dental trauma and dental anomalies such as molar incisor hypomineralisation (MIH), amelogenesis imperfecta (AI), dentinogenesis imperfecta (DI) and fluorosis.
It has been reported that dental conditions with visible aesthetic differences in the incisor teeth are associated with higher levels of dissatisfaction in appearance and have the potential to negatively impact on children’s oral health-related quality of life (Parekh et al. 2014; Porritt et al. 2011; Rodd et al. 2011). Aesthetic management with minimally invasive interventions has been proven to increase children’s self-esteem and quality of life, hence is considered preferable to invasive treatment (Hasmun et al. 2018; Lundgren et al. 2015). Dental bleaching is one such minimally invasive treatment that, following adequate protocols, has shown good results in children and adolescents as shown in Figs. 1 and 2 (Donly et al. 2005; Greenwall-Cohen et al. 2018; Haywood and Sword 2017).
However, in the UK, an ethical and legal dilemma exists following the application of the European Communities Directive 2011/84/EU (2011) which prohibits the use of hydrogen peroxide in concentrations above 0.1% in patients under 18 years of age. After the introduction of this directive, the UK regulatory body, the General Dental Council, produced a statement that bleaching can be performed in those under 18 years old but only ‘wholly for the purpose of treating or preventing disease’ (2016). The provision of dental bleaching has since been severely restricted following concerns regarding indemnity cover (Walshaw et al. 2019). Currently bleaching regulation in the UK is covered by the European Union (Withdrawal) Act (2018) and therefore there have been no changes since leaving the European Union.
Globally, different approaches towards bleaching in children and adolescents have been taken with The American Academy of Pediatric Dentistry bleaching policy for example encouraging the judicious use of bleaching for child and adolescent patients under the guidance of a dentist (American Academy of Pediatric Dentistry 2021). Internationally therefore inconsistencies lie between what treatments dentists are supported to offer to young patients with discoloured teeth.
A recent European survey of paediatric dentists found that 56% of the respondents were unaware of regulations in their country or workplace on bleaching for children and 68% did not provide bleaching for children with dental anomalies (Monteiro et al. 2020). Unfortunately, in cases where dental bleaching was not offered, alternatives were generally more destructive and required greater maintenance. In some instances, treatment was not offered until children reached 18 years of age, which may well be at the detriment to the child’s psychological wellbeing (Marshman et al. 2009). Deterrents to bleaching often include concerns with sensitivity and gingival irritation, both of which have been shown to be transient, with irritation shown to be preventable with well-designed trays (Greenwall-Cohen et al. 2018).
A service evaluation of dental bleaching conducted at the Eastman Dental Hospital in 2018/19 highlighted a lack of comprehensive documentation of bleaching techniques used for patients and therefore drawing conclusions from the data was difficult. Additionally, following a literature search, the authors found limited papers on understanding the child’s perspective on dental bleaching. For this reason, an alternative prospective evaluation was sought in the form of a Patient Reported Outcome Measures (PROMs) questionnaire. Used in healthcare, PROMs are a series of questions completed by patients to ascertain their opinions on their health and care and measure health gain following procedures (NHS Digital 2020). In this evaluation, a self-completed questionnaire measured each patient’s health status and indicators of quality of life upon completion of a course of bleaching.
Aims and objectives
To identify paediatric patient’s satisfaction following dental bleaching treatment, including:
-
The indications for dental bleaching in children
-
The duration of bleaching courses and whether this is used in combination with other treatments to obtain satisfactory results
-
Whether bleaching improved young people’s perception of their appearance
-
What side effects patients experienced
-
Whether patients would recommend bleaching
Materials and methods
The PROMs questionnaire was developed with the UK AI clinical excellence network (UK AI CEN) which is made up of 48 consultants and specialists across at least 15 UK centres. Once the PROM was developed, all members of the UK AI CEN were invited to participate. Five UK centres expressed an interest in participating.
The questionnaire was developed in September 2019 by the authors and peer reviewed with the UK AI CEN as well as piloted with 8 patients (8–16 years) at the Eastman and Newcastle Dental Hospitals. The reading age of the final questionnaire was 11 years, therefore parents were asked to help younger children (Readable© 2020). The font size was increased following feedback from the pilot evaluation but all other feedback was positive. The final questionnaire was electronically shared with a named clinician at each unit, to be printed in black and white, in one A4 sheet, as shown in Fig. 3. It was given to families for completion chairside or in the waiting room during their outpatient visits with a simple explanation that this was anonymous, voluntary and would not affect their on-going care. The PROM questionnaire was registered according to local clinical governance procedures at each unit.
Due to the COVID-19 pandemic, a reduced data collection period was accepted (01/01/2020–16/03/2020). Unfortunately, with the redeployment of staff and lack of patients undergoing routine care, only three units were able to collect and submit results: Eastman Dental Hospital, Newcastle Dental Hospital and Birmingham Dental Hospital. Descriptive statistics were produced using Microsoft Excel 2010. With a small sample size, statistical analysis was not appropriate and therefore only descriptive statistics are reported in the results.
Results
A total of 33 PROM questionnaires were collected. All patients fully completed the questionnaires, however clinician recorded data from six questionnaires was not fully completed and therefore these questionnaires were excluded from analysis.
Characteristics and diagnosis
Table 1 shows the demographics from all 33 questionnaires collected. Descriptive analysis of the questionnaire results was then undertaken for only the fully completed data sets (27 patients) which were analysed (10 male and 17 female, mean age 14 years, range 9–17 years).
AI was the most common reason for dental bleaching to be undertaken, with trauma being the next most frequently recorded diagnosis. Only in two AI cases was the phenotype recorded and so the specific types of AI cases treated could not be further analysed. Of the two patients recorded with a diagnosis of ‘other’ one was stated to have hypomineralisation and the other a ‘poor dental appearance’.
Treatment undertaken
The majority of cases (n = 19, 70%) underwent external bleaching alone. The remainder underwent both internal and external bleaching (walking technique) due to trauma or endodontic treatment.
The average duration for external bleaching was 7.8 weeks (2–36 weeks). For the eight courses of internal/external bleaching, the average duration was 9 weeks (1–24 weeks). Only in eight cases (all external bleaching) was another treatment required, with one case needing two additional treatments (Fig. 4).
Patient-reported outcomes
Twenty-four patients (89%) reported an improvement in the appearance of their teeth after bleaching with the remaining three patients reporting that their teeth had a similar appearance to before. Twenty-two patients (81%) self-reported improvements in their confidence following bleaching with 16 patients (59%) reporting feeling very confident after bleaching in comparison to just 1 reporting feeling confident before (4%) as shown in Fig. 5.
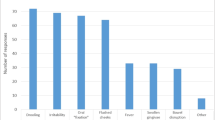
Most patients (n = 17, 63%) reported some sensitivity, however other side effects including any gingival/periodontal problems were not reported (Fig. 6). Two reported sensitivity to be ‘a lot’ with only one then stopping the course of treatment as a result, and this patient still stated that they would recommend dental bleaching. Overall, most patients in the sample (n = 23, 85%) similarly stated that they would recommend bleaching to a friend (Fig. 7), with six making further additional comments in relation to the positive effects of bleaching including ‘It is a great thing to do if you are less confident about your teeth’ and ‘It was very easy and convenient to use’.
Discussion
Tooth discolouration commonly affects anterior teeth and can present an aesthetic concern to patients regardless of age (Marshman et al. 2009) and result in more negative social judgement for adolescents than for peers without discoloured teeth (Al Khayyal et al. 2021). Puberty and secondary education are times when children often become more aware of their own appearance and therefore feelings towards their dental appearance may arise (Rodd et al. 2011). The age range of 9–17 year olds in this UK sample, with an average age of 14 years, reflects this affected population well and demonstrates that bleaching was not a treatment choice for those in the primary dentition.
The results of this study show that internal bleaching is commonly provided for teeth that have had endodontic treatment following dental trauma. Those teeth undergoing a course of combined internal and external bleaching did not require further treatments, suggesting that bleaching alone may be effective in these cases.
Additional treatments were shown to be provided to many patients undergoing external bleaching, with microabrasion the most common adjunct. This may partly be due to external bleaching being more commonly used in cases of anomalies where a greater proportion of the dentition is commonly affected, often to different degrees of severity. Regrettably, this study did not take into account whether these additional treatments were completed before or after the course of bleaching and so the effectiveness of undergoing dental bleaching in isolation as a first-line approach cannot be fully determined.
This study’s results showing that many patients reported low levels of confidence correlates with studies reporting that visible incisor differences are associated with higher levels of dissatisfaction with appearance and have the potential to negatively impact on children’s oral health-related quality of life (Rodd et al. 2011; Lundgren et al. 2015; Dantas-Neta et al. 2016). It was reassuring to see that the vast majority of patients reported seeing an improvement and none reported a worsening in the appearance of their teeth. This demonstrates the vast impact that dental aesthetic concerns have on our young people and the need to appropriately address these issues should not be underestimated.
Although sensitivity was reported by the majority of patients, with only one patient stopping their course of treatment as a result and none of those effected by sensitivity going on to say that they would not recommend bleaching, this study suggests that for most the sensitivity was tolerable and that patients perceived the benefits of bleaching to outweigh any discomfort from this. Sensitivity is a commonly reported side effect of bleaching and it has been found to be transient. Furthermore, bleaching-related sensitivity in children and adolescents seems to be reduced when compared to adults (Donly et al. 2005). It is also of note that as a baseline, 72% of young people with a diagnosis of AI report experiencing pain or sensitivity from their teeth (Lyne et al. 2021). As AI was the most common diagnosis leading to dental bleaching in this study, it must be remembered that they are likely to have had a degree of baseline sensitivity prior to bleaching. In respect of the unique challenges that AI brings to both patients and dental practitioners, the decision to bleach especially for those suffering from hypocalcified and hypomature defects, often would have differing goals and long-term outcomes compared to other patients seeking dental bleaching and may preclude its use altogether. The importance of informing patients and families of risks prior to dental bleaching to gain appropriate consent cannot be underestimated with high-quality patient information leaflets forming part of this process., and the need for the treating clinician to prepare families to combat sensitivity should it occur. For example, instead of using bleaching product every night, the child alternates with a sensitive toothpaste or CPP-ACP in the bleaching tray instead, but if sensitivity is causing significant concern then treatment should be modified or ceased (Greenwall-Cohen et al. 2018).
The other adverse side effect reported was ‘a little bit’ of ‘gum problems’ in two patients within the sample but these patients continued with their bleaching course and both reported that they would still recommend it suggesting their ‘gum problems’ gave minimal discomfort to them. Gingival irritation is a well-known side effect and it is thought to be related to ill-fitting trays or failure to remove excess gel and can be reversed by eliminating over-extensions (Donly et al. 2005; Greenwall-Cohen et al. 2018).
These results suggest that dental bleaching for paediatric patients, in specialist-led centres, is successful. There are limitations of this study, especially with such a small sample. This was unfortunately due to some units having only few suitable patients during the data collection period and also the impact of COVID-19 reducing clinical activity and hence the data collection period ending sooner than planned. The patients involved in this study were also limited to those seen in paediatric dental departments in hospital outpatient settings. Time allocated to the consent process and the resources available to practitioners to fully inform families may often be greater in this setting as opposed to in local dental practices or community settings. The support available in such large trusts for practitioners to develop protocols and standard operating procedures for treatments such as bleaching will often also be greater than those in primary care and so such challenges to providing bleaching as a treatment option are different across these settings and not fully reflected in the sample used in this study. Gaining support from the wider paediatric dentistry community, societies and senior clinicians could challenge the current limited practices in many units and future validation of measures such as this PROM could be used both in the UK and internationally to conduct larger studies suitable for statistical analysis.
Conclusion
Considering the limitations of the present study the following conclusions can be made:
-
Dental bleaching can improve young people’s perception of their appearance and confidence when suffering from conditions that are related to dental discolouration
-
Advantages of dental bleaching include ease of application and minimal intervention precluding the need to remove healthy tooth structure
-
Despite the majority of children in this sample having Amelogenesis Imperfecta, sensitivity is usually not severe and is at a level which patients are able to tolerate
-
Gingival irritation is uncommon with dental bleaching
References
Al Khayyal M, Al Halabi M, Hussein I, Salami A, Rodd H, Hassan A, Kowash M. How do schoolchildren view other children who have discolored teeth? J Int Soc Prevent Communit Dent. 2021;11:340–7. https://doi.org/10.4103/jispcd.JISPCD_46_21.
American Academy of Pediatric Dentistry. Policy on the use of dental bleaching for child and adolescent patients. The Reference Manual of Pediatric Dentistry. Chicago, Ill.: American Academy of Pediatric Dentistry; 2021:116–9.
Dantas-Neta NB, Moura LF, Cruz PF, Moura MS, Paiva SM, Martins CC, Lima MD. Impact of molar-incisor hypomineralization on oral health-related quality of life in schoolchildren. Braz Oral Res. 2016;30(1): e117. https://doi.org/10.1590/1807-3107BOR-2016.vol30.0117.
Donly KJ, Kennedy P, Segura A, Gerlach RW. Effectiveness and safety of tooth bleaching in teenagers. Pediatr Dent. 2005;27(4):298–302.
General Dental Council. Position statement on tooth whitening. 2016. https://www.gdc-uk.org/docs/defaultsource/what-is-the-legal-position/tooth-whitening-positionstatementf08f3f9796b446d88663d00f035d4c13.pdf?sfvrsn=16f71e9_7. Accessed Mar 2021.
Greenwall-Cohen J, Greenwall L, Haywood V, Harley K. Tooth whitening for the under-18-year-old patient. Br Dent J. 2018;225(1):19–26. https://doi.org/10.1038/sj.bdj.2018.527.
Hasmun N, Lawson J, Vettore MV, Elcock C, Zaitoun H, Rodd H. Change in oral health-related quality of life following minimally invasive aesthetic treatment for children with molar incisor hypomineralisation: a prospective study. Dent J (Basel). 2018;6(4):61. https://doi.org/10.3390/dj6040061.
Haywood VB, Sword RJ. Tooth bleaching questions answered. Br Dent J. 2017;223(5):369–80. https://doi.org/10.1038/sj.bdj.2017.767.
Lundgren GP, Karsten A, Dahllöf G. Oral health-related quality of life before and after crown therapy in young patients with amelogenesis imperfecta. Health Qual Life Outcomes. 2015;13:197. https://doi.org/10.1186/s12955-015-0393-3.
Lyne A, Parekh S, Patel N, Lafferty F, Brown C, Rodd H, Monteiro J. Patient-reported outcome measure for children and young people with amelogenesis imperfecta. Br Dent J. 2021. https://doi.org/10.1038/s41415-021-3329-9.
Marshman Z, Gibson B, Robinson PG. The impact of developmental defects of enamel on young people in the UK. Community Dent Oral Epidemiol. 2009;37(1):45–57. https://doi.org/10.1111/j.1600-0528.2008.00453.x.
Monteiro J, Ashley PF, Parekh S. Vital bleaching for children with dental anomalies: EAPD members’ survey. Eur Arch Paediatr Dent. 2020;21(5):565–71. https://doi.org/10.1007/s40368-019-00494-w.
NHS Digital. Patient Reported Outcome Measures (PROMs). 2020. https://digital.nhs.uk/data-andinformation/data-tools-and-services/data-services/patient-reported-outcome-measures-proms. Accessed Mar 2021.
Parekh S, Almehateb M, Cunningham SJ. How do children with amelogenesis imperfecta feel about their teeth? Int J Paediatr Dent. 2014;24(5):326–35. https://doi.org/10.1111/ipd.12080.
Porritt JM, Rodd HD, Baker SB. Quality of life impacts following childhood dento-alveolar trauma. Dent Traumatol. 2011;27(1):2–9. https://doi.org/10.1111/j.1600-9657.2010.00943.x.
Readable. Test your readability. https://readable.com/test-your-readability/. Accessed Nov 2021.
Rodd HD, Marshman Z, Porritt J, Bradbury J, Baker SR. Oral health-related quality of life of children in relation to dental appearance and educational transition. Br Dent J. 2011;211(2):E4. https://doi.org/10.1038/sj.bdj.2011.574.
The Council of the European Union. Council directive 2011/84/EU. Official Journal of the European Union 2011; OJ L 283:36–38.
UK Public General Acts. European Union (Withdrawal) Act 2018 Chapter 16. 2018. https://www.legislation.gov.uk/ukpga/2018/16/pdfs/ukpga_20180016_en.pdf. Accessed Nov 2021.
Walshaw EG, Kandiah P, Rodd H. A trilogy of tragedies—paediatric dental tooth whitening. Br Dent J. 2019;227(11):959–60. https://doi.org/10.1038/s41415-019-0950-y.
Acknowledgements
The authors would like to thank the staff, patients and families that took part in piloting and completing this study and those who consented to use of their clinical images. Thank you to Aspasia Katsimpali and Dimitra Saliakelli for contributing clinical images to this publication.
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
KW, AL, SP and JM contributed to conception, design, data acquisition, analysis and interpretation, drafted and revised the manuscript. KOD and CB contributed to data acquisition. All authors critically revised the drafts and subsequent final paper and approved changes prior to publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wood, K., Lyne, A., O’Donnell, K. et al. Patient-reported outcome measures for children and adolescents having dental bleaching in the UK. Eur Arch Paediatr Dent 23, 579–586 (2022). https://doi.org/10.1007/s40368-022-00721-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40368-022-00721-x