Abstract
Background
Objective
This study aimed to systematically synthesise the cost-effectiveness of screening strategies to detect heterozygous familial hypercholesterolemia (FH).
Methods
We searched seven databases from inception to 2 February , 2023, for eligible cost-effective analysis (CEA) that evaluated screening strategies for FH versus the standard care for FH detection. Independent reviewers performed the screening, data extraction and quality evaluation. Cost results were adapted to 2022 US dollars (US$) to facilitate comparisons between studies using the same screening strategies. Cost-effectiveness thresholds were based on the original study criteria.
Results
A total of 21 studies evaluating 62 strategies were included in this review, most of the studies (95%) adopted a healthcare perspective in the base case, and majority were set in high-income countries. Strategies analysed included cascade screening (23 strategies), opportunistic screening (13 strategies), systematic screening (11 strategies) and population-wide screening (15 strategies). Most of the strategies relied on genetic diagnosis for case ascertainment. The most common comparator was no screening, but some studies compared the proposed strategy versus current screening strategies or versus the best next alternative. Six studies evaluated screening in children while the remaining were targeted at adults. From a healthcare perspective, cascade screening was cost-effective in 78% of the studies [cost-adapted incremental cost-effectiveness ratios (ICERs) ranged from dominant to 2022 US$ 104,877], opportunistic screening in 85% (ICERs from US$4959 to US$41,705), systematic screening in 80% (ICERs from US$2763 to US$69,969) and population-wide screening in 60% (ICERs from US$1484 to US$223,240). The most common driver of ICER identified in the sensitivity analysis was the long-term cost of lipid-lowering treatment.
Conclusions
Based on reported willingness to pay thresholds for each setting, most CEA studies concluded that screening for FH compared with no screening was cost-effective, regardless of the screening strategy. Cascade screening resulted in the largest health benefits per person tested.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Familial hypercholesterolemia results in high levels of cholesterol that lead to premature cardiovascular disease if undetected and untreated. |
Many studies have evaluated the cost-effectiveness of different strategies for the screening for familial hypercholesterolemia, including cascade screening, systematic, opportunistic and population wide screening. |
Most of the studies reported ICERs below the willingness-to-pay thresholds in each setting. Combining strategies may optimise the cost-effectiveness. |
1 Introduction
Heterozygous Familial Hypercholesterolemia (FH) is characterised by elevated levels of low-density lipoprotein cholesterol (LDL-C), leading to premature atherosclerosis, and significantly raising the susceptibility to cardiovascular disease (CVD) [1]. With an estimated prevalence of 1:311, FH impacts more than 34 million people worldwide, making it one of the most common monogenic disorders [2]. The early onset and high incidence of cardiovascular events among FH patients result in substantial morbidity, mortality and economic burden for patients and healthcare systems [3,4,5].
Statins are safe, effective and cost-effective for reducing the risk of premature CVD in FH patients [6]. Owing to the asymptomatic nature of atherosclerosis development, screening plays a pivotal role in identifying individuals with FH to enable early intervention and prevent cardiovascular events [6]. However, under-detection remains one of the major barriers to care for FH patients and reimbursed screening strategies are still rare, although some high-income countries have started national programs in the last few years [7, 8]. Still, only a handful of countries are achieving even 10% detection rates [9, 10]. This may in part be related to limited reports on the value of screening for FH, particularly in children.
Understanding the long-term health and economic implications of the different screening strategies for FH can aid implementation policies [11]. Previous systematic reviews have collated health economic evidence on screening strategies for FH [12, 13]. However, the broader testing and implementation of new screening strategies (i.e. universal or systematic) and their implementation in diverse populations (i.e. children) warrants an evidence update. This updated systematic review examined the cost-effectiveness of published FH screening strategies, synthesised screening, and modelling characteristics as well as model drivers. By determining the most contemporary cost-effective approaches, policymakers and healthcare providers can make informed decisions regarding the implementation of FH screening programs, ultimately reducing the burden of disease for individuals, healthcare systems, and society.
2 Methods
This study was conducted and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines. The quality of the included studies was evaluated using the Drummond checklist [14], and the quality of reporting of each study was evaluated using the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement [15]. The PRISMA checklist is available in Appendix 1 of the supplementary material. The study protocol was prospectively registered in PROSPERO (CRD42023396039).
2.1 Eligibility criteria for study selection
The following characteristics composed the inclusion criteria (i) the population of interest were any individuals with heterozygous FH; (ii) the intervention was any screening strategy for the detection (including using lipid levels, clinical diagnosis and/or genetic testing for case ascertainment) of FH; (iii) the comparator was the standard of care for FH detection in each setting; and (iv) the outcome was the incremental cost-effectiveness ratio (ICER) of the screening strategy compared with the standard of care. We excluded (i) studies evaluating management strategies for FH if they did not include a prior screening component and (ii) studies not providing a comparative economic outcome (i.e. an ICER). Publications other than original research articles (i.e. reviews, opinion letters, systematic reviews and meta-analyses) were also excluded from this systematic review.
2.2 Search strategy
CM and ZA developed the search strategy according to Medical Subject Heading (MeSH) terms and the current literature on the topic. The search was based on the concepts of FH, screening and economic evaluation. The literature search was conducted in MEDLINE via Ovid, EMBASE via Ovid, Scopus, the Cochrane Library, the Economic Literature Database (EconLit) via EBSCOHost, the International HTA Database (INAHTA) and the NHS Economic Evaluation Database (EED) and Database of Abstracts of Reviews of Effects (DARE). We searched for studies published from inception to 2 February 2023. Combinations of terms of MeSH and keywords were used to identify eligible studies in the search strategy. The full search strategies are available in Appendix 2. The language was restricted to English and Spanish. The reference lists of included studies and previous reviews of interest were also screened for additional studies. Four reviewers in independent pairs (TA, AL, CM and PD) screened titles and abstracts, and four reviewers screened the full text of selected studies (TA, CM, AL and PD). Discrepancies were resolved by CM. Conference abstracts were excluded under the assumption that they may not provide as much granular detail needed to perform a thorough analysis of the methods and the results.
2.3 Data extraction and synthesis
Data extraction was performed using a data extraction template adapted for the outcomes of interest. Collected data included the author, year of publication, country of setting, the objective of the study, intervention, comparator, general characterisation of the model (model type, perspective, time horizon, treatment arms, discount rate and currency year), baseline risks and treatment effectiveness and their data sources, types of costs, total costs, total outcomes, ICERs and results from sensitivity analyses. Studies were grouped by screening strategy in data extraction summaries. Screening strategies were defined as cost-effective on the basis of each study’s willingness to pay (WTP) threshold.
2.4 Quality assessment
Quality assessment was performed independently by four reviewers in independent pairs (ML, DA, YB and CM). The methodological quality of the studies was assessed using the Drummond checklist [14] and reporting quality was assessed using the 28 items checklist provided in the CHEERS statement (2022 version) [15]. If any reviewer was also an author in an evaluated study, that reviewer was excluded from evaluating and resolving discrepancies, and a different reviewer completed the assessment. Any other discrepancies were resolved by CM. The results for each Drummond and CHEERS item were summarised in a colour histogram with “yes”, “no” and “unclear” categories, depending on the criteria fulfilment. On the basis of the fulfilment of each criterion, each item was rated with 1 point (green), 0.5 points (yellow) or 0 points (red). For reporting the results, the total percentage of criteria fulfilment for each study was calculated. Items that were not applicable to the study were subtracted from the total number of items for the score.
2.5 Cost adjustments methods
To be able to compare ICERs in a common currency and cost-effectiveness plane, all costs were adapted to 2022 US dollars (US$) using the cost-adjustment method previously validated and published by Ademi et al. [16]. Briefly, the methodology follows three steps: first, the total direct medical costs of each study were adjusted for the level of healthcare resource utilisation between each country and the USA. Second, the prices of healthcare in each country were adjusted with the US prices, and third, costs were adjusted for inflation in the common setting of choice (i.e., the USA). Further details for the cost adaptation process and the adaptation tables with each adjustment factor are presented in Appendix 3.
Beyond cost adaptation to a common cost-effectiveness plane, Table 3 includes the cost-effectiveness thresholds (CET) for each jurisdiction calculated by Woods et al. [17] based on the opportunity costs in each setting. These CETs are based on empirical estimations of opportunity costs and the relationship between each country’s gross domestic product and the value of statistical life. The CETs reported in Table 3 correspond to those reported by Woods et al. [17] in US$ and adjusted for purchasing power parities and have been adjusted for inflation to 2022 US$ using data from the Organisation for Economic Cooperation and Development (OECD).
3 Results
3.1 Search results
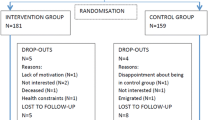
After duplicate removal, our search strategy resulted in 2314 unique records. After title and abstract screening, 99 studies were included in the full-text screening process. From these 99 studies, 20 were deemed eligible according to the inclusion and exclusion criteria and were selected for data extraction and quality appraisal. Upon further revision, two publications were deemed to be duplicate reports of the same study, and thus only one [18] was kept for data extraction and evaluation. Two further studies fulfilling the criteria were included as articles in-press [19, 20] after the search was concluded but before starting the data extraction and quality appraisal. In total, this systematic review includes 21 studies. The searching, screening and inclusion procedure is summarised in the PRISMA flowchart in Fig. 1.
3.2 Quality appraisal
Overall, the quality of the studies was deemed very high, with most studies obtaining above 85% fulfilment of criteria in both the Drummond and the CHEERS checklist (Fig. 2). The overall average percentages for the Drummond checklist were 90% and for CHEERS 88%. The percentages of fulfilment for each study were similar in both checklists. The item with most negative scores in Drummond was item 16 (“Quantities of resource use are reported separately from their unit costs”), while in CHEERS it was the early planning of health economic analysis. The Drummond and CHEERS assessment results can be found in Appendices 4 and 5.
Cost-adapted results from different health strategies (healthcare perspective) presented in a common cost-effectiveness plane for costs (2022 USD) and QALYs. Strategies were included in the cost-effectiveness plane if they reported health benefits and costs per person, if costs were adaptable to 2023 USD and if the comparator was standard of care (i.e. for studies that evaluated several strategies and compared several against the next best alternative, only the one comparing against standard of care was included). Strategies that did not fulfil these criteria could not be presented in a common same cost-effectiveness plane. 1. Marang et al. [28], 2. Oliva et al. [31], 3. Nherera et al. [24], 4. Ademi et al. (2014) [20], 5. Lazaro et al. [32], 6. Kerr et al. [25], 7. McKay et al. [26], 8. Crosland et al. [30], 9. Ademi et al. (2020) [21], 10. Ontario Health [37], 11. Spencer et al. [34], 12.Marquina et al. (2021) [23], 13. Ademi et al. (2023) [18], 14. Marquina et al. (2023) [19]
3.3 General characteristics of the included studies
Of the 21 included studies, five studies were set in Australia [20, 21, 22, 23], four in the UK [24, 25, 26, 27], three in the Netherlands [19, 28, 29], two in England and Wales [18, 30], two in Spain [31, 32], two in the USA [33, 34], one in Poland [35], one in Argentina [36], and one in Canada [37]. All the studies were reported in English. All studies were published in peer-reviewed journals except the one set in Canada, which was published by Ontario’s Health Technology Assessment (HTA) agency [37]. None of the studies were set in low or middle-income countries. Most studies evaluated more than one screening strategy or different types of case ascertainment (and hence the number of strategies evaluated is larger than the total number of included studies). Of the selected studies, 17 evaluated cascade screening, either as a standalone strategy [18, 19, 22, 23, 24, 25, 28, 29, 31, 33, 37] or in combination with other strategies [26, 30, 32, 35, 36, 38]. Six studies evaluated a population-wide screening strategy [18, 21, 26, 34, 35, 36], four evaluated an opportunistic strategy (in most cases followed by cascade screening) [18, 32, 35, 38], and three evaluated a systematic screening strategy using electronic medical records [20, 27, 30]. General characteristics for the included studies are presented in Table 1.
Most of the studies (80%) used a lifetime horizon for the evaluation, while Ademi et al. [23] and Lazaro et al. [32] used a 10-year horizon, Spencer et al. [34] a 20-year, and Jones et al. [27] a 12-weeks horizon. In all. 6 studies used a decision tree for their analysis [18, 24, 27, 29, 32, 36] mostly based on life-table data, and 13 used a decision tree followed by a Markov model [19, 20, 21, 22, 23, 25, 26, 30, 33, 34, 35, 37, 38]. In addition, two studies did not describe the analytical design [28, 31]. Most studies (71%) reported cost per QALY gained as the main outcome of interest, four reported cost per life year gained (LYG) [18, 28, 29, 31] (of note, all four were published before 2010), one study reported both cost per quality-adjusted life-year (QALY) and cost per LYG as the main outcome [36], and one study reported cost per FH case detected [27]. For studies that reported QALYs, 10 studies used the EQ-5D instrument for the utility weights [19, 20, 21, 22, 23, 24, 32, 33, 37, 38]. Out of the 21 included studies, 6 included strategies focusing on children (from age 1–10 years) [19, 22, 26, 36, 38] or adolescents (16 years) [18] as their target population, and the remaining focused on adult populations.
From the included studies, only three reported the number needed to screen (i.e. the number of people that needs to undergo screening to avoid one adverse outcome).
3.4 Screening strategies
There were four main screening strategies that were evaluated: (1) cascade screening, which involved the screening of relatives of an index case with diagnosed or suspected FH; (2) opportunistic screening, which involved offering screening to any individual with or without symptoms as they present to a health care practice or other institutions (i.e. schools) for reasons unrelated to the disease; (3) systematic screening, which usually involved screening of some form of medical records to detect potential FH cases and differs from universal screening in that a prior step trying to identify high-risk individuals is conducted before the actual FH case ascertainment; and (4) population-wide screening, which involved the screening of a whole defined segment of the population with no prior criteria for detecting high-risk individuals.
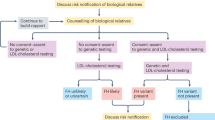
3.4.1 Cascade screening
Of the 21 included studies, 17 evaluated cascade screening either as a standalone strategy [18, 19, 22, 23, 24, 25, 28, 29, 31, 33, 37] or in combination with other strategies [26, 30, 32, 35, 36, 38]. Of note, we defined cascade screening as a standalone strategy if the studies did not include the costs and process of finding the index cases. All the studies included genetic testing for case ascertainment, either alone, in combination, or in comparison with other clinical and/or lipid level-based diagnostic tools. Of the studies that compared ascertainment methods, Nherera et al. [24] compared genetic versus genetic plus clinical, Chen et al. [33] compared cascades screening using genetic testing versus cascade screening using lipid testing and lipid testing plus an adherence program and McKay et al. [26] and Crosland et al. [30] compared seven and eight different ascertainment strategies, respectively. Three studies evaluated national cascade screening strategies in the Netherlands (both in adult relatives [28, 29] and children [19]), in Spain [31, 32] and in the UK [18, 26]. In addition, the Ontario HTA reported an analysis of cascade screening for first-, second- or third-degree relatives using lipid testing, cholesterol testing or both [37]. From the studies that evaluated cascade screening, five did not define the relatives or family members tested (first or second degree).
3.4.2 Opportunistic screening
Four studies [18, 22, 35, 38] evaluated some type of opportunistic screening. Marks et al. [18] evaluated three forms of opportunistic screening: (i) by offering lipid testing to all individuals presenting to a primary care practice, (ii) by offering lipid testing only to 16-year-olds presenting at a primary care practice, and (iii) by testing patients after a premature myocardial infarction (MI). In all cases, the first screening step involved lipid testing followed by case ascertainment using genetic testing or clinical criteria. Lazaro et al. [32] evaluated the implementation of the national program for FH in Spain. In this study, adult individuals and their first-degree relatives (either adult or children) are offered genetic testing for FH after a high cholesterol result in a routine lipid panel, thus combining opportunistic cholesterol screening with cascade screening. Pelczarska et al. [35] evaluated the screening of individuals after an acute CVD event using clinical or genetic ascertainment. Finally, Martin et al. [38] evaluated the screening of 1–2 year old children receiving a scheduled immunisation at a healthcare practice by testing blood samples for high cholesterol levels, followed by genetic testing if total cholesterol was above the 95th percentile. If results were positive for FH, both parents were offered cascade screening (again via lipid testing and genetic testing). The study used the model previously published by Ademi et al. [22] to estimate long-term outcomes.
3.4.3 Systematic screening
Three studies evaluated the systematic screening of electronic medical records to detect potential FH patients (11 strategies in total). From the eight different strategies evaluated, Crosland et al. [30] included the systematic screening of electronic medical records from primary or secondary care or both, with individuals identified using the Simon Broome or the Dutch Lipid Network criteria, followed by genetic testing and cascade screening. Marquina et al. [20] evaluated the systematic screening of electronic medical records in primary care to identify potential FH cases using the Dutch Lipid Network Criteria, followed by a care management plan for positive cases. Finally, Jones et al. [27] evaluated the cost-effectiveness of FH case finding in the UK using electronic medical records and five different algorithms compared with no active screening. The authors reported the ICER in terms of cost per FH case found over a short time-horizon (12 weeks).
3.4.4 Population-wide screening
Six studies evaluated a population-wide screening strategy [18, 21, 26, 34, 35, 36] (15 strategies in total). Marks et al. [18] evaluated a strategy involving sending invitations to all primary care patients (either with no age restrictions or focused on 16 year olds) followed by lipid testing and clinical or genetic ascertainment. McKay et al. [26] analysed seven different population-wide screening strategies, based on cholesterol or genetic testing, with or without following with cascade screening. Pelczarska et al. [35] evaluated a population-wide screening strategy in Poland that involved screening individuals getting their first job (with clinical or genetic ascertainment) and a population-wide screening of all children aged 6 years (with genetic ascertainment). Both Spencer et al. [34] in the USA and Marquina et al. [21] in Australia evaluated the population-wide screening using genetic testing. In Spencer et al. [34] the authors target a population of 20 years olds, while Marquina et al. [21] captured a population aged 18–40 years [20]. Finally, Araujo et al. [36] evaluated the population-wide screening of children at 6 years old in Argentina using cholesterol levels as the first testing criteria.
3.5 Perspective, costs and benefits
All the studies but four adopted a healthcare perspective for the base case analysis: three studies evaluated both a healthcare and a societal perspective [19, 20, 32], and Chen et al. [33], adopted a societal perspective. Additionally, nine studies included a societal perspective in sensitivity analyses. In terms of the costs included, most studies included testing costs, the costs of acute and chronic management for CVD and the cost of routine healthcare visits. All the studies but two [27, 38] included the long-term costs of lipid-lowering treatment. In the study by Jones et al. [27] the short time horizon was not designed to capture subsequent treatment or CVD (acute or chronic) costs. While indirect cost can refer to a variety of items, in the included studies indirect costs mainly referred to productivity losses. Costs were discounted in all but two studies [27, 28] (of note, Jones et al. [27] used a 12-week time horizon which does not warrant discounting). Discounting rates varied from 1.5% in Canada [37] to 5% in Australia [20, 21, 22, 23], and Marks et al. [18] used a 6% discount for costs only in England and Wales. Only Nherera et al. [24] and Chen et al. [33] included adverse events from subsequent cholesterol-lowering treatment in the model. Details on costs and benefits are presented in Table 2.
In terms of incremental health outcomes per person screened, the largest benefits per person were reported for cascade screening for a child population (2.54 QALY gained) [19] while the lowest health benefits were reported for population-wide screening (0.001 QALYs gained) [34]. For opportunistic screening, health gains per person screened varied between 0.085 and 0.05 QALYs gained (of note, two of the studies evaluating opportunistic screening did not report granular outcomes per person). For systematic screening, health gains per person varied between 0.058 and 0.012 QALYs, both reported by Crosland et al. [30] and for population-wide screening, the health gains per person screened varied between 0.006 [21] and 0.001 QALYs [34].
3.6 Cost-adaptation to 2022 USD
To allow a comparison between the results of the studies in the different settings, costs were adapted to 2022 US$. Costs per person were adapted from studies that reported granular costs per person screening, evaluated a healthcare perspective and provided information on the currency year. Marks et al. [18] and Martin et al. [38] were excluded from adaptation process a due to lack of information. In addition, Wonderling et al. [29], Pelczarska et al. [35], and Araujo et al. [36] were not included in the adaptation process as the study setting had a different currency that the one used for results reporting. The cost adapted ICERs are reported in 2022 US$ unless indicated otherwise. Table 2 includes original and adapted costs per person screened and Table 3 presents original, adapted ICERs and opportunity costs CET (USD/QALY).
3.7 Cost-effectiveness results
Overall, 77% of ICERs evaluating a healthcare perspective for any screening strategy were found to be cost-effective under the original analysis criteria and willingness-to-pay thresholds for the base-case. All were cost-effective when the comparator was no screening. From a societal perspective, four out of five reported ICERs resulted in cost-effective results. All cost-effectiveness results are presented in Table 3.
As a standalone strategy, cascade screening was evaluated in 23 analyses and was found cost-effective in 78% of the reported ICERs, with healthcare ICER values ranging from dominant in cascade screening for children in Australia [22] to US$104,877 in cascade screening of third-degree relatives using lipid plus genetic testing in Canada [37]. The HTA report by Ontario health [37] also found cascade screening not to be cost-effective (compared with no screening) for second- and third-degree relatives using genetic or sequential (genetic plus lipids) testing. However, in this study cascade screening for first degree relatives was found cost-effective for both lipid and genetic testing. Only Chen et al. [33] reported results that were not cost-effective from a societal perspective (i.e. including costs from lost productivity). The study was set in the USA and evaluated cascade screening on the basis of genetic ascertainment compared with the current standard of care of cascade screening with lipid testing resulting in an ICER of US$519,813/QALY gained (for a US$100,000 willingness-to-pay threshold) [33]. Chen et al. reported one of the largest costs per person screened (incremental cost of US$5,198 per person).
From the 4 studies focusing on opportunistic screening, there were 10 reported ICERs resulting from opportunistic screening as a standalone strategy and 3 ICERs for opportunistic screening followed by cascade screening, all from a healthcare perspective. All but two strategies (opportunistic screening with genetic ascertainment after an acute CVD event and opportunistic screening in 16-year old people presenting to primary care, both evaluated by Marks et al. [18]) resulted in cost-effective ICERs. This translated to 85% of cost-effective results for opportunistic screening, with ICERs between US$1,484 to US$41,705.
From the three studies evaluating systematic screening, there were 10 strategies evaluated with 11 reported ICERs, 10 from a healthcare perspective [20, 27, 30] and 1 from a societal perspective [20]. All strategies but two were found to be cost-effective (80% cost-effective from a healthcare perspective and 100% cost-effective from a societal perspective). ICERs ranged between $2763 and $69,969 (both reported by Crosland et al. [30]). The upper range ICER corresponds to systematic screening of primary and secondary care electronic medical records using either the Simon Broome or the Dutch Lipid Network criteria and was found no cost-effective compared with the next best alternative (i.e. screening of primary care electronic medical records only).
For population-wide screening, 15 strategies were evaluated in six different studies, with ICERs ranging from US$1484 and US$223,240 per QALY gained. As a standalone, seven strategies yielded cost-effective results [18, 21, 35, 36] in the UK, Australia, Poland and Argentina, and one strategy did not show cost-effective results in the US [34]. From the remaining eight strategies, all combining population-wide screening with cascade screening, four were found cost-effective in Spain and the UK, whilst four were not cost-effective (of note, all the no cost-effective strategies were compared against the best next alternative, not against the standard of care).
3.8 Model drivers- and robustness of the results
Most studies included one-way sensitivity analysis, scenario analysis and probabilistic sensitivity analysis. According to results from one-way analysis, the most common driver impacting the model results for all strategies was the long-term or chronic costs of lipid-lowering treatment, which was mentioned in 17 studies. Most models were also sensitive to adherence to lipid-lowering treatment, discounting rates and the size effect of the lipid-lowering treatment. For population-wide screening, the cost per test was also found to be a key driver for the main outcomes. In all, 11 of the included studies [3, 19, 20, 21, 22, 23, 26, 27, 30, 31, 33, 37] reported results from probabilistic sensitivity analyses. All of them reported results above 50% of the simulations yielding cost-effective results. The lowest proportion of cost-effective simulations was reported by Crosland et al. (57% of simulations cost-effective) and eight studies reported a proportion of cost-effective simulations above 90% [19, 20, 21, 22, 23, 24, 26, 31].
4 Discussion
Overall, most screening strategies for FH were found to be cost-effective compared with standard of care that usually included no active screening. Cascade screening was the most evaluated strategy (in total, the 21 studies included 23 evaluations of cascade screening as a standalone strategy) and were found to be cost-effective in 78% of the analysis. Opportunistic screening was found to be cost-effective in 85% of the evaluated strategies, while systematic screening was cost-effective 80% and population-wide screening in 60%, although in four out of the five strategies that were not cost-effective for population-wide screening, the comparator was the next best alternative, not the standard of care.
Our results are mostly consistent with previous evidence synthesis studies [12, 13] but include a larger variety of strategies, reflecting contemporary literature. Cascade screening has been consistently demonstrated to be cost-effective across different settings, with ICERs from healthcare perspective ranging from cost-saving to US$104,877 (2022 US$). Indeed, cascade screening targeting children has shown cost-effective results in all the included studies. This finding directly contradicts the latest recommendations against screening for FH in children and adolescents in the community, a recommendation derived from limited US data and cholesterol testing alone [39]. Cascade screening also resulted in the larger health gains per person screened and per person detected. In the studies included, only Chen et al. [33] reported that cascade screening was not cost-effective from a societal perspective when comparing cascade screening using genetic testing versus lipid testing (i.e. the current standard of care in the modelled population). However, the authors reported that the current cascade screening with lipid testing will be cost-effective with a program targeted to increase statin adherence. The study identified the high cost of FH sequencing as the main parameter driving the results. For the overall studies on cascade screening, the increased prevalence of FH in relatives of FH subjects (i.e. having a higher risk target population) may contribute to explaining the positive results. The choice of case ascertainment for cascade screening has yielded controversial results, with some studies showing good cost-effectiveness compared with cholesterol testing alone [24] and others showing ICERs above WTP [33]. Of note, lipid testing may fail to detect up to 20% of FH patients, due to overlapping in the LDL-C levels of FH and non-FH individuals [40]. Many efforts have been made to implement and promote cascade screening for FH at a national level in different contexts. However, despite the clear economic evidence most of these initiatives still have limited scope. Efforts to optimise cascade screening include comprehensive programs to raise awareness among primary care physicians as well as among FH index cases and their relatives. Paediatric patients can be most effectively detected using genetic cascade testing from affected parents, but additional methods of screening will be required to identify a sizeable proportion of the population, as suggested by Wald et al. [41].
For opportunistic screening, a key advantage is the immediate availability of the population of interests, since screening is done usually at a point of care during routine clinic visits. This can reduce program costs in comparison to broader population-level screening strategies, though overall case detection numbers may be lower. Systematic screening strategies have started to be considered only more recently; leveraging electronic medical records offers the opportunity to detect potential high-risk patients at a fraction of the cost of other screening strategies, since the information to assess high risk of FH has already been collected. However, this strategy relies heavily on the use of electronic medical records (which are not implemented in all contexts) and it can underestimate the resources needed to mobilise healthcare practitioners and patients and to confirm diagnoses. ICERs for systematic screening varied depending on the type of patients included (primary versus secondary prevention) and the diagnostic algorithm applied. Moreover, the comparator was also a key consideration, since all the non-cost-effective strategies were comparing against the next best systematic screening alternative, not against the standard of care for FH detection in each setting. Finally, population-wide screening has mostly showed cost-effective results (only one study reported results above the willingness to pay threshold when comparing against standard of care), but is the strategy with the largest variability, with ICERs varying from US$1484 in the study Marks et al. [18] set in the UK to US$195,485 in the study Spencer et al. [34] set in the USA (without following with cascade screening). Population screening was also the strategy with the largest variability in the targeted populations, which could contribute to explaining the wide range of results. The diverse results could also be an artefact of the relatively small number of studies that assessed population screening, with only five studies including it as a strategy.
While not an inherent feature of screening per se, most analyses showed that adherence to long-term treatment is one of the main drivers of cost-effectiveness. The results have two major implications. First, it is important to keep lipid-lowering costs low. Second, it is key to keep adherence rates high. While low adherence would imply lower lipid-lowering costs in the model, low adherence has been shown to affect CVD risk reduction, and thus it can result in more acute CVD events and chronic management costs, which will reduce the cost-effectiveness of screening and early detection.
4.1 Limitations of this systematic review
Our review has several limitations. The generalisation of the cost-effectiveness results is debatable, since all the studies were set in Western countries, which can make it difficult to translate to other contexts such as low- and middle-income countries. Indeed, the only country included in the evaluations without universal healthcare access (the USA) has shown large differences in cost-effectiveness with the remaining countries. Generalisation is also difficult due to the different comparators and types of costs included in each study, even for the same type of screening. On the other hand, the fact that most studies found FH screening to be cost-effective, even when applying different criteria or when set in different context, speaks to the robustness of the conclusions. Regarding the cost adaptation, the estimated costs and ICERs derived from the adaptation of cost cannot be directly interpreted as the true ICERs for the USA. These cost adaptation exercises should be approached as an approximation of the cost-effectiveness levels to be expected for a common setting. Nevertheless, the overall cost-effectiveness results in the four analysed strategies were consistent when adapted to the US setting. Finally, our study did not include articles published in non-English/Spanish languages, which can be a source of publication bias.
4.2 Limitations of the reviewed cost-effectiveness studies
The cost-effectiveness studies analysed also had some limitations. First, the lack of publicly available models limits the capacity to compare between settings and countries, since many model features remain obscure. Second, most studies did not report key screening features such as the number needed to screen or the screening uptake. Even when the uptake was reported, it was likely an overestimation or a best-case scenario. Third, most of the included studies only adopted a healthcare perspective in their analyses, overlooking the wider societal implications of screening policies. Another major consideration was the presentation of the ICERs only against the best next alternative in some studies, with non-existence of a universal standard care comparator. Therefore, the generalisability of the results for other contexts is also challenging.
5 Conclusions
Most of the screening strategies assessed showed cost-effective results and were robust to the sensitivity and scenario analyses. Cascade screening showed the greatest health benefit per person screened, but studies may have missed a significant proportion of the undetected FH population by focusing only on relatives of index cases. Novel strategies, including systematic screening and population-wide screening may be cost-effective in combination with cascade screening to raise overall detection rates. Thus, the upcoming challenge in FH detection could be implementing a seamless application of the various screening methods reviewed and their integration with cost-effective management of disease.
References
Watts GF, Sullivan DR, Hare DL, Kostner KM, Horton AE, Bell DA, et al. Integrated guidance for enhancing the care of familial hypercholesterolaemia in Australia∗. Heart Lung Circ. 2021;30(3):324–49.
Hu P, Dharmayat KI, Stevens CAT, Sharabiani MTA, Jones RS, Watts GF, et al. Prevalence of familial hypercholesterolemia among the general population and patients with atherosclerotic cardiovascular disease. Circulation. 2020;141(22):1742–59.
Ademi Z, Marquina C, Zomer E, Bailey C, Owen A, Pang J, et al. The economic impact of familial hypercholesterolemia on productivity. J Clin Lipidol. 2020;14(6):799-806.e3.
Patel P, Hu Y, Kolinovsky A, Geng Z, Ruhl J, Krishnamurthy S, et al. Hidden burden of electronic health record-identified familial hypercholesterolemia: clinical outcomes and cost of medical care. J Am Heart Assoc. 2019;8(13): e011822.
Araujo LR. Estimated costs of hospitalization due to coronary artery disease attributable to familial hypercholesterolemia in the Brazilian public health system. Arch Endocrinol Metab. 2018;62(3):303–8.
Versmissen J, Oosterveer DM, Yazdanpanah M, Defesche JC, Basart DC, Liem AH, et al. Efficacy of statins in familial hypercholesterolaemia: a long term cohort study. BMJ. 2008;337: a2423.
Page C, Zheng H, Wang H, Rai TS, O’Kane M, Hart P, et al. A comparison of the Netherlands, Norway and UK familial hypercholesterolemia screening programmes with implications for target setting and the UK’s NHS long term plan. PLOS Glob Public Health. 2023;3(4): e0001795.
Singh S, Bittner V. Familial hypercholesterolemia–epidemiology, diagnosis, and screening. Curr Atheroscler Rep. 2015;17(2):482.
Federation WH. Familial Hypercholesterolemia: country mapping survey—preliminary analysis. World Heart Federation, FH Europe; 2022.
Vallejo-Vaz AJ, De Marco M, Stevens CAT, Akram A, Freiberger T, Hovingh GK, et al. Overview of the current status of familial hypercholesterolaemia care in over 60 countries—The EAS Familial Hypercholesterolaemia Studies Collaboration (FHSC). Atherosclerosis. 2018;277:234–55.
Watts GF, Gidding SS, Hegele RA, Raal FJ, Sturm AC, Jones LK, et al. International Atherosclerosis Society guidance for implementing best practice in the care of familial hypercholesterolaemia. Nat Rev Cardiol. 2023;20(12):845–69.
Ademi Z, Watts GF, Juniper A, Liew D. A systematic review of economic evaluations of the detection and treatment of familial hypercholesterolemia. Int J Cardiol. 2013;167(6):2391–6.
Jahn B, Santamaria J, Dieplinger H, Binder CJ, Ebenbichler C, Scholl-Bürgi S, et al. Familial hypercholesterolemia: a systematic review of modeling studies on screening interventions. Atherosclerosis. 2022;355:15–29.
Drummond MFS, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2015.
Husereau D, Drummond M, Augustovski F, de Bekker-Grob E, Briggs AH, Carswell C, et al. Consolidated health economic evaluation reporting standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. Pharmacoeconomics. 2022;40(6):601–9.
Ademi Z, Tomonaga Y, van Stiphout J, Glinz D, Gloy VL, Raatz H, et al. Adaptation of cost-effectiveness analyses to a single country: the case of bariatric surgery for obesity and overweight. Swiss Med Wkly. 2018;148(2324): w14626.
Woods B, Revill P, Sculpher M, Claxton K. Country-level cost-effectiveness thresholds: initial estimates and the need for further research. Value Health. 2016;19(8):929–35.
Marks D, Wonderling D, Thorogood M, Lambert H, Humphries SE, Neil HA. Cost effectiveness analysis of different approaches of screening for familial hypercholesterolaemia. BMJ. 2002;324(7349):1303.
Ademi Z, Norman R, Pang J, Sijbrands E, Watts GF, Hutten BA, et al. Cost-effectiveness and return on investment of a nationwide case-finding program for familial hypercholesterolemia in children in the Netherlands. JAMA Pediatr. 2023;177(6):625–32.
Marquina C, Morton J, Brett T, Lloyd M, Radford J, Heal C, et al. Enhancing the detection and care of heterozygous familial hypercholesterolemia in primary care: cost-effectiveness and return on investment. Circ Genom Precis Med. 2023;16(3):267–74.
Marquina C, Lacaze P, Tiller J, Riaz M, Sturm AC, Nelson MR, et al. Population genomic screening of young adults for familial hypercholesterolaemia: a cost-effectiveness analysis. Eur Heart J. 2022;43(34):3243–54.
Ademi Z, Norman R, Pang J, Liew D, Zoungas S, Sijbrands E, et al. Health economic evaluation of screening and treating children with familial hypercholesterolemia early in life: many happy returns on investment? Atherosclerosis. 2020;304:1–8.
Ademi Z, Watts GF, Pang J, Sijbrands EJ, van Bockxmeer FM, O’Leary P, et al. Cascade screening based on genetic testing is cost-effective: evidence for the implementation of models of care for familial hypercholesterolemia. J Clin Lipidol. 2014;8(4):390–400.
Nherera L, Marks D, Minhas R, Thorogood M, Humphries SE. Probabilistic cost-effectiveness analysis of cascade screening for familial hypercholesterolaemia using alternative diagnostic and identification strategies. Heart. 2011;97(14):1175–81.
Kerr M, Pears R, Miedzybrodzka Z, Haralambos K, Cather M, Watson M, et al. Cost effectiveness of cascade testing for familial hypercholesterolaemia, based on data from familial hypercholesterolaemia services in the UK. Eur Heart J. 2017;38(23):1832–9.
McKay AJ, Hogan H, Humphries SE, Marks D, Ray KK, Miners A. Universal screening at age 1–2 years as an adjunct to cascade testing for familial hypercholesterolaemia in the UK: a cost-utility analysis. Atherosclerosis. 2018;275:434–43.
Jones M, Akyea RK, Payne K, Humphries SE, Abdul-Hamid H, Weng S, et al. Cost-effectiveness of screening algorithms for familial hypercholesterolaemia in primary care. J Pers Med. 2022;12(3):330.
Marang-van-de-Mheen PJ, ten Asbroek AH, Bonneux L, Bonsel GJ, Klazinga NS. Cost-effectiveness of a family and DNA based screening programme on familial hypercholesterolaemia in The Netherlands. Eur Heart J. 2002;23(24):1922–30.
Wonderling D, Umans-Eckenhausen MA, Marks D, Defesche JC, Kastelein JJ, Thorogood M. Cost-effectiveness analysis of the genetic screening program for familial hypercholesterolemia in The Netherlands. Semin Vasc Med. 2004;4(1):97–104.
Crosland P, Maconachie R, Buckner S, McGuire H, Humphries SE, Qureshi N. Cost-utility analysis of searching electronic health records and cascade testing to identify and diagnose familial hypercholesterolaemia in England and Wales. Atherosclerosis. 2018;275:80–7.
Oliva J, López-Bastida J, Moreno SG, Mata P, Alonso R. Cost-effectiveness analysis of a genetic screening program in the close relatives of Spanish patients with familial hypercholesterolemia. Rev Esp Cardiol. 2009;62(1):57–65.
Lázaro P, Pérez-de-Isla L, Watts GF, Alonso R, Norman R, Muñiz O, et al. Cost-effectiveness of a cascade screening program for the early detection of familial hypercholesterolemia. J Clin Lipidol. 2017;11(1):260–71.
Chen CX, Hay JW. Cost-effectiveness analysis of alternative screening and treatment strategies for heterozygous familial hypercholesterolemia in the United States. Int J Cardiol. 2015;181:417–24.
Spencer SJ, Jones LK, Guzauskas GF, Hao J, Williams MS, Peterson JF, et al. Cost-effectiveness of population-wide genomic screening for familial hypercholesterolemia in the United States. J Clin Lipidol. 2022;16(5):667–75.
Pelczarska A, Jakubczyk M, Jakubiak-Lasocka J, Banach M, Myśliwiec M, Gruchała M, et al. The cost-effectiveness of screening strategies for familial hypercholesterolaemia in Poland. Atherosclerosis. 2018;270:132–8.
Araujo MB, Zerbino MC. Cost-effectiveness of pediatric universal screening for familial hypercholesterolemia in Argentina. Value Health Reg Issues. 2023;33:33–41.
Health O. Genetic testing for familial hypercholesterolemia: health technology assessment. Ont Health Technol Assess Ser. 2022;22(3):1–155.
Martin AC, Hooper AJ, Norman R, Nguyen LT, Burnett JR, Bell DA, et al. Pilot study of universal screening of children and child-parent cascade testing for familial hypercholesterolaemia in Australia. J Paediatr Child Health. 2022;58(2):281–7.
Barry MJ, Nicholson WK, Silverstein M, Chelmow D, Coker TR, Davis EM, et al. Screening for lipid disorders in children and adolescents: US preventive services task force recommendation statement. JAMA. 2023;330(3):253–60.
Lee C, Rivera-Valerio M, Bangash H, Prokop L, Kullo IJ. New case detection by cascade testing in familial hypercholesterolemia: a systematic review of the literature. Circ Genom Precis Med. 2019;12(11): e002723.
Wald DS, Bestwick JP. Reaching detection targets in familial hypercholesterolaemia: comparison of identification strategies. Atherosclerosis. 2020;293:57–61.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Conflict of Interest
DA, YB, TA, AL and PD report no conflict of interest. CM, JIM, ML and ZA are authors in some of the studies included in this systematic review; no other conflict of interest. GFW reports honoraria for lectures and advisory boards or research grants from Amgen, outside the submitted work.
Data Availability
Not applicable.
Author Contributions
CM contributed to study conceptualisation, quality appraisal, data extraction, and cost-adaptation processes and wrote the first manuscript. JD, ML, DA, TA, PD, AL and YB contributed to data extraction, quality appraisal and editing of the manuscript. GW contributed to the editing of the manuscript. ZA contributed to study conceptualisation, editing of the manuscript, supervision and is the study guarantor.
Compliance with Ethical Standards
Ethics approval was not required for this study as it relied on published and publicly available data.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Marquina, C., Morton, J., Lloyd, M. et al. Cost-Effectiveness of Screening Strategies for Familial Hypercholesterolaemia: An Updated Systematic Review. PharmacoEconomics 42, 373–392 (2024). https://doi.org/10.1007/s40273-023-01347-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-023-01347-7