Abstract
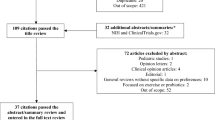
Inflammatory bowel disease (IBD) is a chronic illness with periods of varying disease activity called flares and remissions. Since IBD impacts quality of life, patients make IBD disease management decisions every day. Previous research indicates limited insight about factors that influence decisions regarding disease management and the types of decisions IBD patients make. The purpose of this integrative review is to identify types of treatment and non-treatment decisions and the factors that influence decision making regarding disease management among individuals with IBD. An integrative literature review was performed based on the Whittemore and Knafl framework. PubMed, Web of Science, and PsychINFO were searched for relevant articles, from 2010–2016, using the key terms: decision making, patient preferences, self-management, self-care, nutrition, diet, stress, symptom, Colitis, Crohns, and IBD. Twenty-eight articles met the inclusion criteria. From these, research showed two types of decisions: treatment decisions related to medication and surgery, and non-treatment decisions focused on diet modification. Five themes that influence decisions were identified: experiencing symptoms, provider recommendations, convenience attributes, psychosocial factors, and informational needs. Most of the studies found a positive relationship between an increased number of symptoms and a patient’s willingness to engage in treatment decisions. Although support from providers is highly influential for treatment decisions, most studies reported that provider recommendations did not align with patient preferences. Future work is needed to understand factors that influence decisions among recently diagnosed patients, to focus on non-treatment-related decisions, and to clarify the role of psychosocial factors in promoting disease decision making among IBD patients. This integrative review identified that, for patients, experiencing symptoms is the most important factor that influences treatment and non-treatment decisions.

Similar content being viewed by others
References
Crohn’s and Colitis Foundation of America. Managing flares and other IBD symptoms. New York: Crohn’s and Colitis Foundation of America; 2009.
Crohn’s and Colitis Foundation of America. The facts about inflammatory bowel diseases. New York: Crohn’s and Colitis Foundation of America; 2015.
Leitner GC, Vogelsang H. Pharmacological- and non-pharmacological therapeutic approaches in inflammatory bowel disease in adults. World J Gastrointest Pharmacol Ther. 2016;7(1):5–20.
Ye Y, et al. The epidemiology and risk factors of inflammatory bowel disease. Int J Clin Exp Med. 2015;8(12):22529–42.
Jedel S, et al. A randomized controlled trial of mindfulness-based stress reduction to prevent flare-up in patients with inactive ulcerative colitis. Digestion. 2014;89(2):142–55.
Limdi JK, Aggarwal D, McLaughlin JT. Dietary practices and beliefs in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2016;22(1):164–70.
Grey M, et al. A revised self- and family management framework. Nurs Outlook. 2015;63(2):162–70.
Ryan P, Sawin KJ. The individual and family self-management theory: background and perspectives on context, process, and outcomes. Nurs Outlook. 2009;57(4):217–25.
Kaplan GG. The global burden of IBD: from 2015 to 2025. Nature Reviews. Gastroenterol Hepatol. 2015;12(12):720–7.
Herman ML, Kane SV. Treatment nonadherence in inflammatory bowel disease: identification, scope, and management strategies. Inflamm Bowel Dis. 2015;21(12):2979–84.
Higgins PD, et al. Systematic review: impact of non-adherence to 5-aminosalicylic acid products on the frequency and cost of ulcerative colitis flares. Aliment Pharmacol Ther. 2009;29(3):247–57.
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–53.
Rini C, et al. Interpersonal influences on patients’ surgical decision making: the role of close others. J Behav Med. 2011;34(5):396–407.
Kahn SA, et al. Patient perceptions of fecal microbiota transplantation for ulcerative colitis. Inflamm Bowel Dis. 2013;19(7):1506–13.
Allison M, et al. Surgery in young adults with inflammatory bowel disease: a narrative account. Int J Nurs Stud. 2013;50(11):1566–75.
Byrne CM, et al. Patient and clinician preferences for surgical and medical treatment options in Ulcerative Colitis. Colorectal Dis. 2014;16(4):285–92.
Siegel CA, et al. When should ulcerative colitis patients undergo colectomy for dysplasia? Mismatch between patient preferences and physician recommendations. Inflamm Bowel Dis. 2010;16(10):1658–62.
Brown LK, et al. Proximity to disease and perception of utility: physicians’ vs patients’ assessment of treatment options for ulcerative colitis. Dis Colon Rectum. 2011;54(12):1529–36.
Bewtra M, et al. Patient preferences for surgical versus medical therapy for ulcerative colitis. Inflamm Bowel Dis. 2014;20(1):103–14.
Lichtenstein G, et al. Assessing drug treatment preferences of patients with Crohn’s Disease. Patient: Patient-Cent Outcomes Res. 2010;3(2):113–23.
Vavricka SR, et al. Systematic assessment of factors influencing preferences of Crohn’s disease patients in selecting an anti-tumor necrosis factor agent (Choose TNF trial). Inflamm Bowel Dis. 2012;18(8):1523–30.
Kim ES, et al. Factors contributing to the preference of Korean patients with Crohn’s disease when selecting an anti-tumor necrosis factor agent (CHOICE Study). Gut Liver. 2016;10(3):391–8.
Hodgkins P, et al. Patient preferences for first-line oral treatment for mild-to-moderate ulcerative colitis: a discrete-choice experiment. Patient. 2012;5(1):33–44.
Peyrin-Biroulet L, et al. Patient perspectives on biosimilars: a survey by the European Federation of Crohn’s and Ulcerative Colitis associations. J Crohns Colitis. 2017;11(1):128–33.
Bewtra M, Johnson FR. Assessing patient preferences for treatment options and process of care in inflammatory bowel disease: a critical review of quantitative data. Patient. 2013;6(4):241–55.
Casellas F, et al. Patient preferences for inflammatory bowel disease treatment objectives. Dig Liver Dis. 2017;49(2):152–6.
Peyrin-Biroulet L, et al. Treatment satisfaction, preferences and perception gaps between patients and physicians in the ulcerative colitis CARES study: a real world-based study. Dig Liver Dis. 2016;48(6):601–7.
van Deen WK, et al. Value redefined for inflammatory bowel disease patients: a choice-based conjoint analysis of patients’ preferences. Qual Life Res. 2017;26(2):455–65.
Carpio D, et al. Perception of disease burden and treatment satisfaction in patients with ulcerative colitis from outpatient clinics in Spain: UC-LIFE survey. Eur J Gastroenterol Hepatol. 2016;28(9):1056–64.
Siegel CA, et al. Novel statistical approach to determine inflammatory bowel disease: patients’ perspectives on shared decision making. Patient. 2016;9(1):79–89.
Kemp K, et al. An exploration of the follow-up up needs of patients with inflammatory bowel disease. J Crohns Colitis. 2013;7(9):e386–95.
Vagianos K, et al. What are adults with inflammatory bowel disease (IBD) eating? A closer look at the dietary habits of a population-based Canadian IBD Cohort. J Parenter Enteral Nutr. 2016;40(3):405–11.
Zallot C, et al. Dietary beliefs and behavior among inflammatory bowel disease patients. Inflamm Bowel Dis. 2013;19(1):66–72.
Schreiber S, et al. Perception gaps between patients with ulcerative colitis and healthcare professionals: an online survey. BMC Gastroenterol. 2012;12:108.
Thompson KD, et al. Patients with ulcerative colitis are more concerned about complications of their disease than side effects of medications. Inflamm Bowel Dis. 2016;22(4):940–7.
Bernstein KI, et al. Information needs and preferences of recently diagnosed patients with inflammatory bowel disease. Inflamm Bowel Dis. 2011;17(2):590–8.
Pittet V, et al. Information needs and concerns of patients with inflammatory bowel disease: what can we learn from participants in a bilingual clinical cohort? PLoS One. 2016;11(3):e0150620.
Wong S, et al. The information needs and preferences of persons with longstanding inflammatory bowel disease. Can J Gastroenterol. 2012;26(8):525–31.
Johnson FR, et al. Are gastroenterologists less tolerant of treatment risks than patients? Benefit-risk preferences in Crohn’s disease management. J Manag Care Pharm. 2010;16(8):616–28.
Keefer L, Kane S. Self-management techniques in IBD. In: Cross RK, Watson AR, editors. Telemanagement of inflammatory bowel disease. Berlin: Springer; 2016. p. 55–70.
Khanna R, et al. Endoscopic scoring indices for evaluation of disease activity in Crohn’s disease. Cochrane Database Syst Rev. 2016;8:Cd010642.
Novak K, et al. Clinic-based point of care transabdominal ultrasound for monitoring Crohn’s disease: impact on clinical decision making. J Crohns Colitis. 2015;9(9):795–801.
Walsh AJ, Bryant RV, Travis SPL. Current best practice for disease activity assessment in IBD. Nat Rev Gastroenterol Hepatol. 2016;13(10):567–79.
Muhlbacher AC, Juhnke C. Patient preferences versus physicians’ judgement: does it make a difference in healthcare decision making? Appl Health Econ Health Policy. 2013;11(3):163–80.
Goldberg HB, Shorten A. Differences between patient and provider perceptions of informed decision making about epidural analgesia use during childbirth. J Perinat Educ. 2014;23(2):104–12.
Tanaka M, et al. Coping strategies for possible flare-ups and their perceived effectiveness in patients with inflammatory bowel disease. Gastroenterol Nurs. 2016;39(1):42–7.
Cohan JN, et al. A novel decision aid for surgical patients with ulcerative colitis: results of a pilot study. Dis Colon Rectum. 2016;59(6):520–8.
Baker DM, et al. A systematic review of internet decision-making resources for patients considering surgery for ulcerative colitis. Inflamm Bowel Dis. 2017;23(8):1293–300.
Acknowledgements
Dr. Barbara Given critically reviewed and provided feedback on the draft manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with Ethical Standards
Kendra Kamp obtained funding for this project from the Jonas Foundation, Michigan State University College of Nursing, George and Margaret Lorimer Parsons Nursing Endowed Scholarship, and the William and Angeline Keehner Scholarship. Kendra has no conflicts of interests to disclose. Kelly Brittain has no conflicts of interests to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kamp, K.J., Brittain, K. Factors that Influence Treatment and Non-treatment Decision Making Among Individuals with Inflammatory Bowel Disease: An Integrative Review. Patient 11, 271–284 (2018). https://doi.org/10.1007/s40271-017-0294-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-017-0294-0