Abstract
Guselkumab (TREMFYA®), a fully human immunoglobulin G1λ (IgG1λ) monoclonal antibody that selectively targets interleukin (IL)-23, is an effective and generally well-tolerated treatment option for active psoriatic arthritis. Guselkumab is administered subcutaneously and can be used alone or in combination with methotrexate. In randomized, double-blind, placebo-controlled phase 3 trials in adults with active psoriatic arthritis and an inadequate response to or intolerance of standard treatment, guselkumab was effective in reducing disease activity and structural damage progression. Guselkumab conferred improvements in arthritis, enthesitis, dactylitis, psoriasis, axial symptoms, physical function and health-related quality of life. The clinical benefits of guselkumab for the diverse signs and symptoms of psoriatic arthritis increased or were maintained through two years of treatment, with no new safety signals emerging.
Plain Language Summary
Psoriatic arthritis is an inflammatory joint disease that commonly occurs in patients with psoriasis. While several drugs are now available for the treatment of psoriatic arthritis, patients often need to switch treatments due to inadequate efficacy or tolerability concerns. Guselkumab (TREMFYA®) treats psoriatic arthritis via a novel mechanism of action. In well-designed clinical trials, guselkumab provided durable improvements in the various signs and symptoms of psoriatic arthritis (including arthritis, joint inflammation and structural damage, skin disease and spinal manifestations). Guselkumab recipients reported gains in physical function and health-related quality of life. Guselkumab is an effective option for the treatment of active psoriatic arthritis and is generally well tolerated, with no new safety concerns identified during longer-term use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Digital Features for this Adis Drug Q&A can be found at https://doi.org/10.6084/m9.figshare.14331431. |
First-in-class fully human IgG1λ monoclonal antibody selectively targeting IL-23 |
Reduces disease activity in patients with active psoriatic arthritis despite standard treatment |
Improves diverse signs/symptoms of psoriatic arthritis |
Clinical benefits durable over longer-term treatment |
Favourable benefit-risk profile |
What is the rationale for developing guselkumab in psoriatic arthritis?
Psoriatic arthritis is a chronic inflammatory joint disease commonly associated with psoriasis [1, 2]; while relatively rare in the general population (with prevalence estimates of < 1% [3]), psoriatic arthritis occurs in ≈ 20–30% of patients affected by psoriasis [4,5,6]. There is considerable overlap in the pathophysiological features of the two conditions [1, 7]. Aside from psoriasis, clinical manifestations of psoriatic arthritis are diverse and include peripheral arthritis, enthesitis, dactylitis, spinal disease, nail lesions and uveitis [1, 7]. In order to prevent lasting structural damage and disability, early diagnosis and treatment is vital [8]. Treatment aims should include the achievement of disease remission or, alternatively, a state of low disease activity [9].
Historically, the treatment of psoriatic arthritis has been approached in a similar manner to that of rheumatoid arthritis, with the use of conventional synthetic disease-modifying antirheumatic drugs (DMARDs) such as methotrexate [8, 10]. However, evidence for the efficacy of these agents in treating the diverse features of psoriatic arthritis is limited [8, 10]. Increased understanding of the immunopathogenesis of psoriatic arthritis has facilitated the development of treatments that target specific signalling pathways implicated in the disease, and the last decade has seen a proliferation of novel treatment options for psoriatic arthritis, including biologic and targeted synthetic DMARDs [2, 10]. As patients often need to switch treatments due to a lack of efficacy, a loss of efficacy over time or tolerability concerns [11], the availability of effective and well-tolerated agents with distinct mechanisms of action is desirable. The interleukin (IL)-23/IL-17 axis cytokines have been implicated in the pathogenesis of both psoriasis and psoriatic arthritis, and the inhibition of IL-12/23 or IL-17A with monoclonal antibodies has proved an efficacious approach to the treatment of these conditions [7].
Guselkumab (TREMFYA®), a fully human immunoglobulin G1λ (IgG1λ) monoclonal antibody selectively targeting IL-23, was the first in its class to be approved for the treatment of moderate to severe plaque psoriasis in the EU and USA [12]. Use of guselkumab in this indication has been reviewed previously [12]. Guselkumab has since been approved for use in the treatment of psoriatic arthritis in several countries/regions including the EU [13], USA [14] and Japan [15]. Table 1 provides a summary of the prescribing information for guselkumab in the treatment of psoriatic arthritis in the aforementioned regions [13,14,15]. Consult local prescribing information for further details.
What are the pharmacological properties of guselkumab?
Guselkumab, a fully human IgG1λ monoclonal antibody, binds selectively to the p19 subunit of IL-23 with high affinity [13, 16]. In doing so, it blocks interaction between IL-23 and the cell surface IL-23 receptor, thus inhibiting IL-23-mediated signalling, activation and pro-inflammatory cytokine cascades [13].
Guselkumab reduced levels of acute phase proteins C-reactive protein (CRP) and serum amyloid A (SAA), IL-6, and Th17 effector cytokines (IL-17A, IL-17F and IL-22) as early as 4 weeks after treatment initiation in patients with active psoriatic arthritis in phase 3 clinical trials [17]. At week 24, levels of all aforementioned proteins were significantly (p < 0.05) reduced with each guselkumab regimen (100 mg administered subcutaneously at week 0, week 4, and either every 4 or every 8 weeks thereafter) relative to those at week 0. At baseline, patients had significantly (p < 0.05) higher levels of CRP, SAA, IL-6, IL-17A and IL-17F than healthy controls [17].
Guselkumab pharmacokinetics in patients with psoriatic arthritis are similar to those in patients with plaque psoriasis (previously reviewed [12]) [13, 14]. In brief, guselkumab exhibited linear pharmacokinetics in patients with moderate to severe psoriasis (subcutaneous dose range 10–300 mg) [18]. In patients with psoriatic arthritis administered subcutaneous guselkumab 100 mg at week 0, week 4 and every 8 weeks thereafter, steady-state trough serum concentrations were generally reached by week 20 [16]. When guselkumab 100 mg was administered in patients with psoriatic arthritis at week 0, week 4 and either every 8 weeks or 4 weeks thereafter, mean steady-state trough serum concentrations were ≈ 1.2 µg/mL and ≈ 3.8 µg/mL with the respective regimens [13]. The absolute bioavailablity of guselkumab after a single subcutaneous 100 mg dose was estimated to be ≈ 49% in healthy volunteers [13, 14]. In a population pharmacokinetic (PPK) analysis in patients with plaque psoriasis, guselkumab had an apparent volume of distribution of 13.5 L and clearance of 0.516 L/day in the final model; the model-derived elimination half-life was 18.1 days [19].
Like endogenous IgG, human IgG monoclonal antibodies such as guselkumab are expected to be eliminated via intracellular catabolism into amino acids and small peptides [13, 14]. Based on this elimination route, neither hepatic impairment nor abnormal kidney function is anticipated to impact guselkumab pharmacokinetics to any clinically meaningful extent [13]. Concomitant medications (e.g. NSAIDs, oral corticosteroids, conventional DMARDs including methotrexate) did not impact guselkumab clearance in PPK analyses [13, 14].
What is the efficacy of guselkumab in psoriatic arthritis?
Guselkumab 100 mg administered subcutaneously every 4 or 8 weeks is effective in treating active psoriatic arthritis in patients with an inadequate response to or intolerance of standard treatment [20,21,22]. The efficacy of guselkumab was demonstrated in the double-blind, multinational, phase 3 DISCOVER-1 [21] and DISCOVER-2 [20] trials. These trials enrolled adults meeting classification criteria for psoriatic arthritis, with ≥ 3 swollen joints, ≥ 3 tender joints and CRP ≥ 0.3 mg/dL [21] or ≥ 5 swollen joints, ≥ 5 tender joints and CRP ≥ 0.6 mg/dL [20] despite standard therapies. Eligibility criteria included psoriasis or a history thereof and an inadequate response to or intolerance of apremilast (discontinued > 4 weeks before study treatment), non-biologic DMARDs or NSAIDs for psoriatic arthritis [20, 21]. In DISCOVER-1, ≈ 30% of participants had previously received one or two tumour necrosis factor (TNF) inhibitors while the remaining participants were biologic-naïve [21]. All participants in DISCOVER-2 were biologic-naïve [20]. In each trial, patients were randomized to receive subcutaneous guselkumab 100 mg every 4 weeks (referred to hereafter as guselkumab 4-weekly), guselkumab 100 mg at week 0, week 4 and every 8 weeks thereafter (hereafter guselkumab 8-weekly), or placebo, with randomization stratified by baseline non-biologic DMARD use and either previous TNF inhibitor use [21] or CRP concentration [20]. Across trials, ≈ 58% of patients received methotrexate as background therapy [13]. After the 24-week placebo-controlled treatment period, there was an active treatment period up until week 52 [21] or week 100 [20]; at week 24, all placebo recipients commenced treatment with guselkumab 4-weekly [23, 24]. Results from the DISCOVER trials are supported by those from an earlier randomized, double-blind, placebo-controlled, multinational, phase 2a trial, in which a guselkumab 8-weekly regimen (n = 100 randomized) significantly improved the signs and symptoms of psoriatic arthritis relative to placebo (n = 49) in patients with active psoriatic arthritis despite standard therapy [22, 25].
Guselkumab 4-weekly and guselkumab 8-weekly significantly improved American College of Rheumatology 20% (ACR20) response rates relative to placebo at week 24 (primary endpoint; Table 2) of the DISCOVER trials [20, 21]. With both regimens, ACR20 response gains were consistent across subgroups based on demographic variables, disease characteristics at baseline (including skin disease severity [26]), and previous or baseline medication use (including methotrexate use at baseline and, in DISCOVER-1, previous TNF inhibitor use) [20, 21]. Treatment differences (nominal p < 0.05 vs placebo) in ACR20 were evident as early as week 4 (i.e. after a single injection) in DISCOVER-2 [20] and week 8 in DISCOVER-1 [21]. Improvements with the guselkumab regimens versus placebo were demonstrated across all individual ACR components at week 24 [13, 27]. At week 24, higher proportions of guselkumab 8-weekly and 4-weekly recipients than placebo recipients achieved an ACR 50% (ACR50) response in DISCOVER-1 (30% and 36% vs 9%) and DISCOVER-2 (31% and 33% vs 14%) [nominal p < 0.0001 for each comparison] [20, 21]. An ACR 70% (ACR70) response was achieved by 12% and 20% of guselkumab 8-weekly and 4-weekly recipients versus 6% of placebo recipients (nominal p = 0.0005 for guselkumab 4-weekly vs placebo) in DISCOVER-1 and 19% and 13% versus 4% in DISCOVER-2 (nominal p ≤ 0.0004 for each comparison) [20, 21].
Guselkumab also reduced disease activity based on rates of minimal disease activity achievement and change in the 28-joint disease activity score with CRP (DAS28-CRP) [20, 21]. Higher proportions of guselkumab 8-weekly and 4-weekly recipients than placebo recipients achieved a state of minimal disease activity in DISCOVER-1 (23% and 30% vs 11%; nominal p-values ≤ 0.012) and DISCOVER-2 (25% and 19% vs 6%; nominal p-values < 0.0001). In each trial, least squares mean (LSM) reductions from baseline to week 24 in DAS28-CRP were greater with each guselkumab regimen than with placebo (nominal p-values < 0.0001 for all comparisons) [20, 21].
With respect to the diverse signs and symptoms of psoriatic arthritis, guselkumab offered the following benefits over placebo at week 24 of the DISCOVER trials:
-
Skin disease Both guselkumab regimens significantly improved skin disease based on investigator’s global assessment response (Table 2) [20, 21]. Similarly, higher proportions of guselkumab 8-weekly and 4-weekly recipients than placebo recipients had psoriasis area and severity index (PASI) 75%, 90% and 100% improvements in each trial (nominal p ≤ 0.0005 for all) [20, 21].
-
Enthesitis and dactylitis Resolution of enthesitis was achieved by significantly higher proportions of guselkumab 8-weekly and 4-weekly recipients than placebo recipients (50% and 45% vs 29%; p < 0.05 for both comparisons) in a preplanned pooled analysis of DISCOVER-1 and DISCOVER-2 data from patients with enthesitis at baseline (n = 728) [20]. Resolution of dactylitis was observed in significantly higher proportions of guselkumab 8-weekly and 4-weekly recipients than placebo recipients (59% and 64% vs 42%; p < 0.05 for both comparisons) in a preplanned pooled analysis of data from patients with dactylitis at baseline (n = 473). Both guselkumab regimens afforded greater LSM improvement from baseline in Leeds enthesitis index score and dactylitis score relative to placebo (nominal p-values ≤ 0.0025) [20].
-
Axial symptoms Both guselkumab regimens afforded greater LSM improvement from baseline in Bath ankylosing spondylitis disease activity index (BASDAI), spinal pain, and ankylosing spondylitis disease activity score (ASDAS) with CRP relative to placebo (nominal p-values < 0.001) in a pooled analysis of DISCOVER-1 and DISCOVER-2 data from patients who were identified by physicians as having symptoms consistent with spondylitis and had sacroiliitis confirmed via prior radiograph/MRI or screening radiograph (n = 312) [28].
Guselkumab inhibited radiographic structural damage progression as assessed using psoriatic arthritis-modified van der Heijde-Sharp (vdHS) scores in DISCOVER-2 [20]. Guselkumab 4-weekly recipients demonstrated significantly less radiographic progression than placebo recipients at week 24 (LSM change from baseline in psoriatic arthritis-modified vdHS score 0.29 vs 0.95; p = 0.011), whilst guselkumab 8-weekly recipients demonstrated a non-significant reduction in progression relative to placebo recipients (0.52 vs 0.95) [20].
Both guselkumab regimens significantly improved physical function and health-related quality of life (HR-QOL) as assessed by change from baseline in health assessment questionnaire-disability index (HAQ-DI) and short form-36 (SF-36) physical component summary score at week 24 (Table 2) [20, 21]. Improvements relative to placebo in the change from baseline in SF-36 mental component summary score did not reach statistical significance (Table 2) [20, 21]. At week 24, guselkumab 8-weekly and 4-weekly recipients achieved greater reductions in fatigue (based on functional assessment of chronic illness therapy-fatigue scores) than placebo recipients in both trials (nominal p-values < 0.001) [16, 29].
The clinical benefits of guselkumab were sustained through longer-term treatment in both DISCOVER trials [23, 24]. In each trial, ACR20 response rates at week 52 were numerically higher than those at week 24 in patients randomized to guselkumab 8-weekly or 4-weekly (Table 2). ACR50 response rates increased to 39% and 54% in patients randomized to guselkumab 8-weekly and 4-weekly in DISCOVER-1 and to 48% and 46% in the respective groups in DISCOVER-2, while ACR70 response rates increased to 26% and 29% in DISCOVER-1 and 28% and 26% in DISCOVER-2 [23, 24]. At week 100 of DISCOVER-2, ACR20 response rates were 74% and 76% in patients randomized to guselkumab 8-weekly and 4-weekly [30]. ACR50 response rates were 55% and 56% in the respective groups, while ACR70 rates were 36% and 35% [30].
Guselkumab continued to suppress progression of structural damage seen on plain radiographs during the active treatment period of DISCOVER-2 [30]. In patients randomized to guselkumab 8-weekly and 4-weekly, the observed mean changes in total psoriatic arthritis-modified vdHS scores were 0.99 and 1.06, respectively, during weeks 0–52 and 0.46 and 0.75 during weeks 52–100. In patients randomized to placebo who switched to guselkumab 4-weekly at week 24, mean changes in total psoriatic arthritis-modified vdHS scores were 1.12, 0.34 and 0.13 during weeks 0–24, 24–52 and 52–100, respectively [30].
Guselkumab provided sustained skin responses, including IGA (Table 2) and PASI 75%, 90% and 100% responses, through one year of treatment in DISCOVER-1 and DISCOVER-2 [23, 24], with robust responses persisting through week 100 of the longer DISCOVER-2 trial [30]. In pooled analyses of DISCOVER-1 and DISCOVER-2 data from patients with enthesitis or dactylitis at baseline, enthesitis and dactylitis resolution rates at week 24 were maintained at week 52, as were improvements in Leeds enthesitis index scores or dactylitis severity [24]. At week 52, enthesitis and dactylitis resolution rates were 58% and ≈ 75% in patients randomized to either guselkumab regimen [24]. Resolution rates were maintained through week 100 of DISCOVER-2 [30]. With respect to axial symptoms in patients who were identified by physicians as having symptoms consistent with spondylitis and had sacroiliitis confirmed via prior radiograph/MRI or screening radiograph, LSM changes in BASDAI, spinal pain and ASDAS were stable from week 24 to week 52 in patients randomized to either guselkumab regimen (pooled DISCOVER-1 and DISCOVER-2 data) [31]. Improvements in physical function and HR-QOL were maintained through one year of treatment with guselkumab in both DISCOVER trials (Table 2) and through week 100 of treatment in DISCOVER-2 [30]. The majority of patients treated in DISCOVER-1 (90%) and DISCOVER-2 (93%) completed one year of treatment [23, 24], while 88% of randomized and treated patients completed week 100 of DISCOVER-2 [30].
What is the tolerability profile of guselkumab?
Guselkumab 100 mg administered subcutaneously 8-weekly or 4-weekly is generally well tolerated in patients with psoriatic arthritis, based on data from the phase 2 and 3 clinical trials [20,21,22]. The overall safety profile of guselkumab was largely consistent with that established in patients with psoriasis [20,21,22].
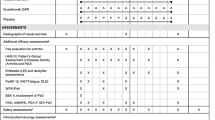
In a pooled analysis of data from the 24-week placebo-controlled periods of the DISCOVER-1 and DISCOVER-2 trials in adults with psoriatic arthritis, the incidence of treatment-emergent adverse events (TEAEs) was similar across treatment arms (48.5% and 48.8% of guselkumab 8-weekly and 4-weekly recipients, compared with 47.3% of placebo recipients) [16, 32]. The most common TEAEs in guselkumab 8-weekly or 4-weekly recipients were nasopharyngitis, increased alanine aminotransferase (ALT), increased aspartate aminotransferase (AST) and upper respiratory tract infection (Fig. 1). ALT and AST elevations were generally mild, transient and not accompanied by clinically significant elevations in bilirubin [16, 32]. Serious TEAEs occurred in 1.9% and 2.1% of guselkumab 8-weekly and 4-weekly recipients compared with 3.2% of placebo recipients [16, 32]. TEAEs of severe intensity were infrequent with guselkumab (occurring in 0.8% and 0.5% of guselkumab 8-weekly and 4-weekly recipients vs 1.6% of placebo recipients) [16]. TEAEs seldom led to discontinuation of the study agent, doing so in 1.3% and 2.1% of guselkumab 8-weekly and 4-weekly recipients versus 1.9% of placebo recipients, and injection-site reaction rates were low (1.3% and 1.1% vs 0.3% of placebo patients) [16, 32].
Most common treatment-emergent adverse events (occurring in ≥ 5% of patients in any treatment arm) with guselkumab in the DISCOVER trials in patients with psoriatic arthritis (through week 24) [16, 32]. ALT alanine aminotransferase, AST aspartate aminotransferase, GUS Q4W guselkumab administered 4-weekly, GUS Q8W guselkumab administered at weeks 0, 4 and 8-weekly thereafter, URTI upper respiratory tract infection
Several warnings and precautions pertain to the use of guselkumab, including a potentially increased risk of infection (Table 3) [13,14,15]. While decreased neutrophil counts were somewhat more common with guselkumab than placebo in the pooled dataset (grade 1: 5.6% and 5.9% of guselkumab 8-weekly and 4-weekly recipients vs 3.2% of placebo recipients; grade 2: 1.6% and 1.6% vs 0.8%; grade 3–4: 0% and 0.3% vs 0.3%), most of these laboratory results were transient and not associated with infection [16, 32]. The guselkumab 8-weekly and 4-weekly groups were comparable to the placebo group with respect to the proportions of recipients reporting ≥ 1 infection (19.5% and 21.4% vs 20.7%) or serious infection (0.3% and 0.8% vs 0.8%) through week 24 [16, 32]. There were no instances of active tuberculosis during DISCOVER-1 or DISCOVER-2, and no opportunistic infections during placebo-controlled treatment [16, 23, 24].
The longer-term tolerability of guselkumab was comparable to that observed during placebo-controlled treatment, with no new safety signals identified through week 60 of DISCOVER-1 (total 365 patient-years of follow-up) [23] or week 112 of DISCOVER-2 (total 1392 patient-years of follow-up) [30]. Guselkumab treatment through week 60 of DISCOVER-1 or week 112 of DISCOVER-2 did not increase the time-adjusted incidences of infections, adverse events leading to treatment discontinuation, or serious adverse events relative to placebo treatment through week 24 of the respective trial [23, 30]. The incidence of serious infections with guselkumab was 1.1 events per 100 patient-years in DISCOVER-1 and 1.9 events per 100 patient-years in DISCOVER-2 (vs 3.5 and 0.9 events per 100 patient-years with placebo through week 24). Opportunistic infections were reported in three guselkumab recipients through week 112 of DISCOVER-2 (fungal esophagitis and disseminated herpes zoster in guselkumab 8-weekly recipients and listeria meningitis in a patient who switched from placebo to guselkumab 4-weekly), while there were no opportunistic infections reported during DISCOVER-1. One patient who switched from placebo to guselkumab 4-weekly in DISCOVER-2 died in a road traffic accident; no other deaths occurred in guselkumab recipients [23, 30].
In the DISCOVER trials, 2% of guselkumab recipients (n = 15) developed anti-drug antibodies during up to 24 weeks of treatment [13]. Of these patients, one had neutralizing antibodies and none developed injection-site reactions [13].
What is the current clinical position of guselkumab in psoriatic arthritis?
The therapeutic landscape for psoriatic arthritis has rapidly evolved over recent years and guselkumab represents an effective and generally well-tolerated treatment option that expands the range of available pharmaceuticals. In adults with active psoriatic arthritis, treatment with subcutaneous guselkumab reduces disease activity [irrespective of dosing interval (8-weekly or 4-weekly), background methotrexate use or previous use of TNF inhibitors] and inhibits the progression of structural joint damage [20, 21]. Psoriatic arthritis is a clinically heterogeneous condition and guselkumab 8-weekly and 4-weekly regimens offer benefits for arthritis symptoms, psoriasis, enthesitis and dactylitis, as well as axial manifestations of the disease. Importantly, guselkumab also improves physical function and physical components of HR-QOL in patients with psoriatic arthritis [20, 21]. Patients with psoriatic arthritis typically report reduced HR-QOL relative to the general population [33], with contributing factors including the psychosocial burden, impaired physical function and comorbidities associated with the condition [34]. Guselkumab provides durable clinical benefits based on results through two years of treatment in clinical trials [23, 30].
Guselkumab is currently the only selective IL-23 inhibitor approved for use in patients with psoriatic arthritis [35]. In patients with psoriasis, the selective blockade of IL-23 appears to be more effective than combined blockade of IL-12/23, with fewer risks [35]. Like that of many other therapies approved for use in psoriatic arthritis, the efficacy of guselkumab in this indication was established in placebo-controlled trials and head-to-head comparisons with active treatments are currently lacking. Systemic reviews and network meta-analyses suggest that guselkumab is generally comparable to most other targeted treatments for psoriatic arthritis with respect to improvements in arthritis, soft tissue damage and physical function, as well as with respect to safety outcomes [36, 37]. Guselkumab may provide greater improvements in psoriasis than some targeted psoriatic arthritis treatments [36, 37], although the results of such indirect comparisons must be interpreted with caution. The 2019 EULAR recommendations for the management of psoriatic arthritis precede the approval of guselkumab, but suggest that a biologic DMARD should be commenced in patients with peripheral arthritis and an inadequate response to ≥ 1 conventional synthetic DMARD (and be considered in certain settings in patients with unequivocal enthesitis or predominantly axial disease) [9]. In patients who respond inadequately to (or are intolerant of) a biologic DMARD, switching to another biologic DMARD or targeted synthetic DMARD should be considered [9]. Well-designed clinical trials directly comparing the efficacy, tolerability and cost-effectiveness of guselkumab with those of other biologic DMARDs are needed to further elucidate the relative position of guselkumab in the treatment of psoriatic arthritis.
Change history
09 July 2021
A Correction to this paper has been published: https://doi.org/10.1007/s40267-021-00851-0
References
Ritchlin CT, Colbert RA, Gladman DD. Psoriatic arthritis. N Engl J Med. 2017;376:957–70.
Coates LC, FitzGerald O, Helliwell PS, et al. Psoriasis, psoriatic arthritis, and rheumatoid arthritis: is all inflammation the same? Semin Arthritis Rheum. 2016;46(3):291–304.
Scotti L, Franchi M, Marchesoni A, et al. Prevalence and incidence of psoriatic arthritis: a systematic review and meta-analysis. Semin Arthritis Rheum. 2018;48(1):28–34.
Alinaghi F, Calov M, Kristensen LE, et al. Prevalence of psoriatic arthritis in patients with psoriasis: a systematic review and meta-analysis of observational and clinical studies. J Am Acad Dermatol. 2019;18(1):251-65.e19.
Feldman SR, Zhao Y, Shi L, et al. Economic and comorbidity burden among moderate-to-severe psoriasis patients with comorbid psoriatic arthritis. Arthritis Care Res. 2015;67(5):708–17.
Lebwohl M, Kavanaugh A, Armstrong AW, et al. US perspectives in the management of psoriasis and psoriatic arthritis: patient and physician results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis (MAPP) survey. Am J Clin Dermatol. 2016;17:87–97.
Sakkas L, Zafiriou E, Bogdanos DP. Mini review: new treatments in psoriatic arthritis. Focus on the IL-23/17 axis. Front Pharmacol. 2019;10:872.
Van den Bosch F, Coates L. Clinical management of psoriatic arthritis. Lancet. 2018;391(10136):2285–94.
Gossec L, Baraliakos X, Kerschbaumer A, et al. EULAR recommendations for the management of psoriatic arthritis with pharmacological therapies: 2019 update. Ann Rheum Dis. 2020;79:700–12.
Kang EJ, Kavanaugh A. Psoriatic arthritis: latest treatments and their place in therapy. Ther Adv Chronic Dis. 2015;6(4):194–203.
Alten R, Conaghan PG, Strand V, et al. Unmet needs in psoriatic arthritis patients receiving immunomodulatory therapy: results from a large multinational real-world study. Clin Rheumatol. 2019;38:1615–26.
Al-Salama ZT, Scott LJ. Guselkumab: a review in moderate to severe plaque psoriasis. Am J Clin Dermatol. 2018;19(6):907–18.
European Medicines Authority. TREMFYA (guselkumab): EU summary of product characteristics. 2020. https://www.ema.europa.eu/. Accessed 6 May 2021.
Janssen Biotech. TREMFYA (guselkumab) injection for subcutaneous use: US prescribing information. 2020. http://dailymed.nlm.nih.gov/. Accessed 6 May 2021.
Janssen Pharma. TREMFYA® subcutaneous injection: Japanese prescribing information. 2020. http://www.pmda.go.jp/. Accessed 6 May 2021.
European Medicines Agency. TREMFYA (guselkumab): extension of indication variation assessment report. 2020. http://www.ema.europa.eu/. Accessed 6 May 2021.
Siebert S, McInnes I, Loza MJ, et al. Guselkumab induces sustained reduction in acute phase proteins and Th17 effector cytokines in active psoriatic arthritis in two phase-3 clinical trials (DISCOVER-1 and DISCOVER-2). Ann Rheum Dis. 2020;79(Suppl. 1):144–5.
Zhuang Y, Calderon C, Marciniak SJ. First-in-human study to assess guselkumab (anti-IL-23 mAb) pharmacokinetics/safety in healthy subjects and patients with moderate-to-severe psoriasis. Eur J Clin Pharmacol. 2016;72:1303–10.
Yao Z, Hu C, Zhu Y. Population pharmacokinetic modeling of guselkumab, a human IgG1λ monoclonal antibody targeting IL-23, in patients with moderate to severe plaque psoriasis. J Clin Pharmacol. 2018;58:613–27.
Mease PJ, Rahman P, Gottlieb AB, et al. Guselkumab in biologic-naive patients with active psoriatic arthritis (DISCOVER-2): a double-blind, randomised, placebo-controlled phase 3 trial. Lancet. 2020;395(10230):1126–36.
Deodhar A, Helliwell PS, Boehncke WH, et al. Guselkumab in patients with active psoriatic arthritis who were biologic-naive or had previously received TNFα inhibitor treatment (DISCOVER-1): a double-blind, randomised, placebo-controlled phase 3 trial. Lancet. 2020;395(10230):1115–25.
Deodhar A, Gottlieb AB, Boehncke WH, et al. Efficacy and safety of guselkumab in patients with active psoriatic arthritis: a randomised, double-blind, placebo-controlled, phase 2 study. Lancet. 2018;391(10136):2213–24.
Ritchlin CT, Helliwell PS, Boehncke WH, et al. Guselkumab, an inhibitor of the IL-23p19 subunit, provides sustained improvement in signs and symptoms of active psoriatic arthritis: 1 year results of a phase III randomised study of patients who were biologic-naïve or TNFα inhibitor-experienced. RMD Open. 2021;7:e001457.
McInnes I, Rahman P, Gottlieb AB, et al. Efficacy and safety of guselkumab, an interleukin-23p19-specific monoclonoal antibody, through 1 year in biologic-naive psoriatic arthritis patients. Arthritis Rheumatol. 2020;73(4):604–16.
Mease PJ, Gladman DD, Deodhar A, et al. Impact of guselkumab, an interleukin-23 p19 subunit inhibitor, on enthesitis and dactylitis in patients with moderate to severe psoriatic arthritis: results from a randomised, placebo-controlled, phase II study. RMD Open. 2020;6(2):1–10.
Gottlieb AB, Mease P, Rahman P, et al. Effects of guselkumab on musculoskeletal features in patients with active psoriatic arthritis by baseline skin disease: results from the phase 3 DISCOVER-1 and DISCOVER-2 studies [abstract]. J Am Acad Dermatol. 2020;83(6 Suppl.):AB36.
Gottlieb AB, Mease PJ, Merola JF, et al. Effects of guselkumab on articular components of American College of Rheumatology score and skin responses in patients with active psoriatic arthritis: results from the phase 3 DISCOVER-2 study. 2020;83(6 Suppl):AB145.
Helliwell P, Gladman DD, Poddubnyy D, et al. Efficacy of guselkumab, a monoclonal antibody that specifically binds to the p19-subunit of Il-23, on endpoints related to axial involvement in patients with active Psa with imaging-confirmed sacroiliitis: week-24 results from two phase 3, randomized, double-blind, placebo-controlled studies [abstract no. OP0054]. Ann Rheum Dis. 2020;79(Suppl. 1):36–7.
Helliwell P, Rahman P, Deodhar A, et al. Guselkumab demonstrated an independent treatment effect on fatigue after adjustment for clinical response (ACR20) in patients with psoriatic arthritis: results from phase-3 trials DISCOVER 1 & 2. Ann Rheum Dis. 2020;79(Suppl. 1):1164.
McInnes IB, Rahman P, Gottlieb AB, et al. Efficacy and safety of guselkumab, a monoclonal antibody specific to the p19-subunit of interleukin-23, through 2 years: results from a phase 3, randomized, double-blind, placebo-controlled study conducted in biologic-naïve patients with active psoriatic arthritis [abstract + poster]. In: Innovations in Dermatology: virtual spring conference; March 16–20. 2021.
Mease P, Helliwell P, Gladman D, et al. Efficacy of guselkumab, a monoclonal antibody that specifically binds to the p19 subunit of IL-23, on axial-related endpoints in patients with active PsA with imaging-confirmed sacroiliitis: week-52 results from two phase 3, randomized, double-blind, placebo-controlled studies [abstract no. 2025]. In: ACR Convergence 2020. 2020.
Rahman P, Ritchlin CT, Helliwell P, et al. Integrated safety results of two phase-3 trials of guselkumab in patients with psoriatic arthritis through the placebo-controlled periods. Ann Rheum Dis. 2020;79(Suppl. 1):776–7.
Wervers K, Luime JJ, Tchetverikov I, et al. Influence of disease manifestations on health-related quality of life in early psoriatic arthritis. J Rheumatol. 2018;14(11):1526–31.
Haugeberg G, Michelsen B, Kavanaugh A. Impact of skin, musculoskeletal and psychosocial aspects on quality of life in psoriatic arthritis patients: a cross-sectional study of outpatient clinic patients in the biologic treatment era. RMD Open. 2020;6(1):e001223.
Hadeler E, Mosca M, Hong J, et al. Advancements in biologic therapy for psoriasis: the IL-23 inhibitors. Curr Dermatol Rep. 2021;10:6–15.
Mease PJ, McInnes I, Tam L-S, et al. Comparative effectiveness of guselkumab in psoriatic arthritis: results from systematic literature review and network meta-analysis. Rheumatology (Oxford). 2021. https://doi.org/10.1093/rheumatology/keab119.
Lu C, Wallace BI, Waljee AK, et al. Comparative efficacy and safety of targeted DMARDs for active psoriatic arthritis during induction therapy: a systematic review and network meta-analysis. Semin Arthritis Rheum. 2019;49(3):381–8.
Acknowledgements
The manuscript was reviewed by: S. Chavez-Alvarez, Dermatology Department, Hospital Universitario Dr. José Eleuterio González, Autonomous University of Nuevo León, Monterrey, Mexico; S. R. Feldman, Department of Dermatology, Wake Forest University School of Medicine, Winston-Salem, NC, USA; A. K. Srivastava, Biotechnology, Indian Institute of Technology, Roorkee, India. During the peer review process, Janssen Biotech, the marketing authorization holder of guselkumab, was offered an opportunity to provide a scientific accuracy review of their data. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Authorship and conflict of interest
Y. N. Lamb is a salaried employee(s) of Adis International Ltd/Springer Nature and declares no relevant conflicts of interest. All authors contributed to the review and are responsible for the article content.
Ethics approval, Consent to participate, Consent for publication, Availability of data and material, Code availability
Not applicable.
Additional information
The original version of this article was revised due to a retrospective Open Access order.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lamb, Y.N. Guselkumab in psoriatic arthritis: a profile of its use. Drugs Ther Perspect 37, 285–293 (2021). https://doi.org/10.1007/s40267-021-00840-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40267-021-00840-3