Abstract
Background
Recognition and management of adverse events (AEs) associated with immune checkpoint inhibitor (ICI) use by cancer patients requires expertise from multiple disciplines. Greater awareness of potential AEs may result in earlier recognition, appropriate management, and better patient outcomes.
Objective
The primary objective of this overview of systematic reviews was to synthesize and consolidate systematic review evidence describing the incidence proportion and severity of AEs associated with various ICI therapies across different cancers.
Methods
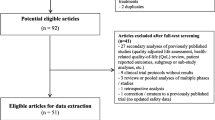
A systematic literature search of four databases was conducted to identify systematic reviews that describe the incidence proportion and severity of AEs related to ICI therapy in cancer patients. A systematic review was eligible if it included adults with cancer; on ICI alone or in combination with another ICI, chemotherapy, or targeted therapy; severity (graded according to the Common Terminology Criteria for Adverse Events) and incidence proportion of AEs and whether it reported its eligibility criteria. AEs of interest were identified through an iterative ranking exercise by key stakeholders and knowledge users. Extraction of PICOTTS elements and quality indicators (AMSTAR-2) were used to manage overlap of primary studies across systematic reviews at the outcome level. Cancer subtypes were mapped to drug class and AE severity.
Results
Overall, 129 systematic reviews met the inclusion criteria for data mapping. Systematic reviews reported incidence proportions for more than 76 AEs, of which 34 were identified as AEs of interest. After overlap assessment, 65 systematic reviews were chosen for data extraction. The three AEs with the highest median incidence were fatigue (18.3%, interquartile range [IQR] 15.0–28.0%), diarrhea (15.3%, IQR 9.7–29.2%) and rash (14.4%, IQR 10.3–19.2%). The three AEs (high-grade) with the highest median incidence were diarrhea (1.5%, IQR 1.2–6.0%), colitis (1.3%, IQR 0.6–6.1%) and neutropenia (1.2%, IQR 0.4–3.3%). Incidence proportions of high-grade AEs were often considerably lower than all-grade AEs and combination therapy (ICI combinations or combinations of ICI with chemotherapy or targeted therapy) was responsible for some of the highest incidence proportions regardless of AE. Rare AEs and certain cancer subtypes were not well reported.
Conclusions
Early recognition of AEs associated with ICIs requires expertise from diverse specialists, not just oncologists. Greater awareness of potential AEs may result in earlier recognition, appropriate management, and better patient outcomes.
PROSPERO Registration
CRD42021231593.


Similar content being viewed by others
References
Schirrmacher V. From chemotherapy to biological therapy: a review of novel concepts to reduce the side effects of systemic cancer treatment. Int J Oncol. 2019;54(2):407–19.
Murciano-Goroff YR, Warner AB, Wolchok JD. The future of cancer immunotherapy: microenvironment-targeting combinations. Cell Res. 2020;30(6):507–19.
Hui E. Immune checkpoint inhibitors. J Cell Biol. 2019;218(3):740–1.
Cancer Care Ontario. Immune Checkpoint Inhibitor Toxicity Management Clinical Practice Guideline. Updated March 2018 [cited 10 Dec 2020]. https://www.cancercareontario.ca/en/guidelines-advice/types-of-cancer/52976. Accessed 10 Dec 2020.
Horrow JC, Digregorio GJ, Barbieri EJ, Rupp E. Intravenous infusions of nitroprusside, dobutamine, and nitroglycerin are compatible. Crit Care Med. 1990;18(8):858–61.
Khoja L, Day D, Wei-Wu Chen T, Siu LL, Hansen AR. Tumour- and class-specific patterns of immune-related adverse events of immune checkpoint inhibitors: a systematic review. Ann Oncol. 2017;28(10):2377–85.
Kirschenbaum HL, Aronoff W, Perentesis GP, Plitz GW, Cutie AJ. Stability and compatibility of lidocaine hydrochloride with selected large-volume parenterals and drug additives. Am J Hosp Pharm. 1982;39(6):1013–5.
Martins F, Sofiya L, Sykiotis GP, Lamine F, Maillard M, Fraga M, et al. Adverse effects of immune-checkpoint inhibitors: epidemiology, management and surveillance. Nat Rev Clin Oncol. 2019;16(9):563–80.
Xing P, Zhang F, Wang G, Xu Y, Li C, Wang S, et al. Incidence rates of immune-related adverse events and their correlation with response in advanced solid tumours treated with NIVO or NIVO+IPI: a systematic review and meta-analysis. J Immunother Cancer. 2019;7(1):341.
Reynolds KL, Cohen JV, Ryan DP, Hochberg EP, Dougan M, Thomas M, et al. Severe immune-related adverse effects (irAE) requring hospital admission in patients treated with immune checkpoint inhibitors for advanced malignancy: Temporal trends and clinical significance. J Clin Oncol. 2018;36(15):3096.
Pollock M FR, Becker LA, Pieper D, Hartling L. Chapter V: Overviews of Reviews: Cochrane; 2020 [updated September 2020. http://www.training.cochrane.org/handbook. Accessed 10 Dec 2020.
Lunny C, Brennan SE, Reid J, McDonald S, McKenzie JE. Overviews of reviews incompletely report methods for handling overlapping, discordant, and problematic data. J Clin Epidemiol. 2020;118:69–85.
Gates M, Gates A, Guitard S, Pollock M, Hartling L. Guidance for overviews of reviews continues to accumulate, but important challenges remain: a scoping review. Syst Rev. 2020;9(1):254.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6.
CADTH. Grey Matters: a practical tool for searching health-related grey literature. 2014. https://www.cadth.ca/resources/finding-evidence/grey-matters. Accessed 10 Dec 2020.
Lunny C, Brennan SE, McDonald S, McKenzie JE. Toward a comprehensive evidence map of overview of systematic review methods: paper 2-risk of bias assessment; synthesis, presentation and summary of the findings; and assessment of the certainty of the evidence. Syst Rev. 2018;7(1):159.
Lunny C, Pieper D, Thabet P, Kanji S. Managing overlap of primary study results across systematic reviews: practical considerations for authors of overviews of reviews. BMC Med Res Methodol. 2021;21(1):140.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. The impact of different inclusion decisions on the comprehensiveness and complexity of overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):18.
Bougioukas KI, Liakos A, Tsapas A, Ntzani E, Haidich AB. Preferred reporting items for overviews of systematic reviews including harms checklist: a pilot tool to be used for balanced reporting of benefits and harms. J Clin Epidemiol. 2018;93:9–24.
Abdel-Rahman O. Toxicity patterns associated with chemotherapy/immune checkpoint inhibitor combinations: a meta-analysis. Immunotherapy. 2019;11(6):543–54.
Almutairi AR, McBride A, Slack M, Erstad BL, Abraham I. Potential immune-related adverse events associated with monotherapy and combination therapy of ipilimumab, nivolumab, and pembrolizumab for advanced melanoma: a systematic review and meta-analysis. Front Oncol. 2020;10:91.
Arnaud-Coffin P, Maillet D, Gan HK, Stelmes J-J, You B, Dalle S, et al. A systematic review of adverse events in randomized trials assessing immune checkpoint inhibitors. Int J Cancer. 2019;145(3):639–48.
Balasubramanian A, Onggo J, Gunjur A, John T, Parakh S. Immune checkpoint inhibition with chemoradiotherapy in stage III non-small-cell lung cancer: a systematic review and meta-analysis of safety results. Clin Lung Cancer. 2021;22(2):74–82.
Barroso-Sousa R, Barry WT, Garrido-Castro AC, Hodi FS, Min L, Krop IE, et al. Incidence of endocrine dysfunction following the use of different immune checkpoint inhibitor regimens: a systematic review and meta-analysis. JAMA Oncol. 2018;4(2):173–82.
Baxi S, Yang A, Gennarelli RL, Khan N, Wang Z, Boyce L, et al. Immune-related adverse events for anti-PD-1 and anti-PD-L1 drugs: systematic review and meta-analysis. BMJ. 2018;360:k793.
Bishay K, Tandon P, Bourassa-Blanchette S, Laurie SA, McCurdy JD. The risk of diarrhea and colitis in patients with lung cancer treated with immune checkpoint inhibitors: a systematic review and meta-analysis. Curr Oncol. 2020;27(5):e486–94.
Chen K, Wang X, Yang L, Chen Z. The anti-PD-1/PD-L1 immunotherapy for gastric esophageal cancer: a systematic review and meta-analysis and literature review. Cancer Control. 2021;28:1073274821997430.
Da L, Teng Y, Wang N, Zaguirre K, Liu Y, Qi Y, et al. Organ-specific immune-related adverse events associated with immune checkpoint inhibitor monotherapy versus combination therapy in cancer: a meta-analysis of randomized controlled trials. Front Pharmacol. 2019;10:1671.
de Filette J, Andreescu CE, Cools F, Bravenboer B, Velkeniers B. A systematic review and meta-analysis of endocrine-related adverse events associated with immune checkpoint inhibitors. Horm Metab Res. 2019;51(3):145–56.
El Osta B, Hu F, Sadek R, Chintalapally R, Tang SC. Not all immune-checkpoint inhibitors are created equal: Meta-analysis and systematic review of immune-related adverse events in cancer trials. Crit Rev Oncol Hematol. 2017;119:1–12.
Facchinetti F, Di Maio M, Tiseo M. Adding PD-1/PD-L1 inhibitors to chemotherapy for the first-line treatment of extensive stage small cell lung cancer (SCLC): a meta-analysis of randomized trials. Cancers. 2020;12(9):2645.
Fu J, Li W-Z, McGrath NA, Lai CW, Brar G, Xiang Y-Q, et al. Immune checkpoint inhibitor associated hepatotoxicity in primary liver cancer versus other cancers: a systematic review and meta-analysis. Front Oncol. 2021;11:650292.
Grunwald V, Voss MH, Rini BI, Powles T, Albiges L, Giles RH, et al. Axitinib plus immune checkpoint inhibitor: evidence- and expert-based consensus recommendation for treatment optimisation and management of related adverse events. Br J Cancer. 2020;123(6):898–904.
Gu Y, Zhang H, Liu Z, Xia Y, Liang B, Liang L. Different patterns of treatment-related adverse events of programmed cell death-1 and its ligand-1 inhibitors in different cancer types: a meta-analysis and systemic review of clinical trials. Asia Pac J Clin Oncol. 2020;16(5):e160–78.
Guo X, Li W, Hu J, Zhu EC, Su Q. Hepatotoxicity in patients with solid tumors treated with PD-1/PD-L1 inhibitors alone, PD-1/PD-L1 inhibitors plus chemotherapy, or chemotherapy alone: systematic review and meta-analysis. Eur J Clin Pharmacol. 2020;76(10):1345–54.
Huang Y-F, Xie W-J, Fan H-Y, Du J. Comparative risks of high-grade adverse events among FDA-approved systemic therapies in advanced melanoma: systematic review and network meta-analysis. Front Oncol. 2020;10:571135.
Khan M, Lin J, Liao G, Tian Y, Liang Y, Li R, et al. Comparative analysis of immune checkpoint inhibitors and chemotherapy in the treatment of advanced non-small cell lung cancer: a meta-analysis of randomized controlled trials. Medicine. 2018;97(33):e11936.
Li H, Xu J, Bai Y, Zhang S, Cheng M, Jin J. Nephrotoxicity in patients with solid tumors treated with anti-PD-1/PD-L1 monoclonal antibodies: a systematic review and meta-analysis. Invest New Drugs. 2021;39(3):860–70.
Li L, Xu F, Chen Y, Ren X, Liu Y, Chen Y, et al. Indirect comparison between immunotherapy alone and immunotherapy plus chemotherapy as first-line treatment for advanced non-small cell lung cancer: a systematic review. BMJ Open. 2020;10(11):e034010.
Li Z-Q, Yan H-C, Gu J-J, Yang Y-L, Zhang M-K, Fang X-J. Comparative efficacy and safety of PD-1/PD-L1 Inhibitors versus platinum-based chemotherapy for the first-line treatment of advanced non-small cell lung cancer: a meta analysis of randomized controlled trials. Pharmacol Res. 2020;160:105194.
Lin L-L, Lin G-F, Yang F, Chen X-Q. A systematic review and meta-analysis of immune-mediated liver dysfunction in non-small cell lung cancer. Int Immunopharmacol. 2020;83:106537.
Liu H, Xu D, Wang W, Sun F, Zhang S, Yang X, et al. Systematic assessment of risk of fever in solid tumor patients treated with PD-1/PD-L1 inhibitors: a systematic review and meta-analysis. Front Oncol. 2020;10:570080.
Liu Q, Fang Z, Liu M, Xu R, Yi F, Wei Y, et al. The benefits and risks of CTLA4 inhibitor plus PD1/PDL1 inhibitor in stage IIIB/IV non-small cell lung cancer: a systematic analysis and meta-analysis based on randomized controlled trials. J Clin Pharm Ther. 2021;46(6):1519–30.
Lu J, Li L, Lan Y, Liang Y, Meng H. Immune checkpoint inhibitor-associated pituitary-adrenal dysfunction: a systematic review and meta-analysis. Cancer Med. 2019;8(18):7503–15.
Lu J, Yang J, Liang Y, Meng H, Zhao J, Zhang X. Incidence of immune checkpoint inhibitor-associated diabetes: a meta-analysis of randomized controlled studies. Front Pharmacol. 2019;10:1453.
Luo W, Wang Z, Tian P, Li W. Safety and tolerability of PD-1/PD-L1 inhibitors in the treatment of non-small cell lung cancer: a meta-analysis of randomized controlled trials. J Cancer Res Clin Oncol. 2018;144(10):1851–9.
Miyashita H, Mikami T, Satoi S, Cruz C, Galsky MD. Incidence and risk of colitis with programmed death 1 versus programmed death ligand 1 inhibitors for the treatment of cancer. J Immunother. 2020;43(9):291–8.
Narayan V, Kahlmeyer A, Dahm P, Skoetz N, Risk MC, Bongiorno C, et al. Pembrolizumab monotherapy versus chemotherapy for treatment of advanced urothelial carcinoma with disease progression during or following platinum-containing chemotherapy. A Cochrane Rapid Review. Cochrane Database Syst Rev. 2018;7(7):CD012838.
Ni X, Xing Y, Sun X, Suo J. The safety and efficacy of anti-PD-1/anti-PD-L1 antibody therapy in the treatment of previously treated, advanced gastric or gastro-oesophageal junction cancer: a meta-analysis of prospective clinical trials. Clin Res Hepatol Gastroenterol. 2020;44(2):211–22.
Ornstein MC, Garcia JA. Toxicity of checkpoint inhibition in advanced RCC: a systematic review. Kidney cancer. 2017;1(2):133–41.
Park R, Lopes L, Cristancho CR, Riano IM, Saeed A. Treatment-related adverse events of combination immune checkpoint inhibitors: systematic review and meta-analysis. Front Oncol. 2020;10:258.
Petrelli F, Ardito R, Borgonovo K, Lonati V, Cabiddu M, Ghilardi M, et al. Haematological toxicities with immunotherapy in patients with cancer: a systematic review and meta-analysis. Eur J Cancer. 2018;103:7–16.
Shi Y, Duan J, Guan Q, Xue P, Zheng Y. Effectivity and safety of PD-1/PD-L1 inhibitors for different level of PD-L1-positive, advanced NSCLC: a meta-analysis of 4939 patients from randomized controlled trials. International immunopharmacology. 2020;84:106452.
Si Z, Zhang S, Yang X, Ding N, Xiang M, Zhu Q, et al. The association between the incidence risk of peripheral neuropathy and PD-1/PD-L1 inhibitors in the treatment for solid tumor patients: a systematic review and meta-analysis. Front Oncol. 2019;9:866.
Sonpavde GP, Grivas P, Lin Y, Hennessy D, Hunt JD. Immune-related adverse events with PD-1 versus PD-L1 inhibitors: a meta-analysis of 8730 patients from clinical trials. Future Oncol. 2021;17(19):2545–58.
Su Q, Sun Z, Zhang C, Hou Y, Cao B. PD-1/PD-L1 antibodies efficacy and safety versus docetaxel monotherapy in advanced NSCLC patients after first-line treatment option: systems assessment. Oncotarget. 2017;8(35):59677–89.
Su Q, Zhu EC, Wu J-B, Li T, Hou Y-L, Wang D-Y, et al. Risk of pneumonitis and pneumonia associated with immune checkpoint inhibitors for solid tumors: a systematic review and meta-analysis. Front Immunol. 2019;10:108.
Tandon P, Bourassa-Blanchette S, Bishay K, Parlow S, Laurie SA, McCurdy JD. The risk of diarrhea and colitis in patients with advanced melanoma undergoing immune checkpoint inhibitor therapy: a systematic review and meta-analysis. J Immunother. 2018;41(3):101–8.
Tian Y, Zhang Z, Yang X, Li D, Zhang L, Li Z, et al. The risk ratio of immune-related colitis, hepatitis, and pancreatitis in patients with solid tumors caused by PD-1/PD-L1 inhibitors: a systematic review and meta-analysis. Front Oncol. 2020;10:261.
Tong Z-Q, Wu D-Y, Liu D, Dong M. Incidence risk of PD-1/PD-L1-related pneumonia and diarrhea in non-small cell lung cancer (NSCLC) patients: a systematic review and meta-analysis of randomized controlled trials. Eur J Clin Pharmacol. 2021;77(8):1079–88.
Tun AM, Thein KZ, Thein WL, Guevara E. Checkpoint inhibitors plus chemotherapy for first-line treatment of advanced non-small cell lung cancer: a systematic review and meta-analysis of randomized controlled trials. Future Sci OA. 2019;5(9):FSO421.
Voutsadakis IA. PD-1 inhibitors monotherapy in hepatocellular carcinoma: meta-analysis and systematic review. Hepatobil Pancreat Dis Int. 2019;18(6):505–10.
Voutsadakis IA. A systematic review and meta-analysis of PD-1 and PD-L1 inhibitors monotherapy in metastatic gastric and gastroesophageal junction adenocarcinoma. Euroasian J Hepato-gastroenterol. 2020;10(2):56–63.
Wang B-C, Cao R-B, Li P-D, Fu C. The effects and safety of PD-1/PD-L1 inhibitors on head and neck cancer: a systematic review and meta-analysis. Cancer Med. 2019;8(13):5969–78.
Wang P-F, Chen Y, Song S-Y, Wang T-J, Ji W-J, Li S-W, et al. Immune-related adverse events associated with anti-PD-1/PD-L1 treatment for malignancies: a meta-analysis. Front Pharmacol. 2017;8:730.
Wang Y, Zhou S, Yang F, Qi X, Wang X, Guan X, et al. Treatment-related adverse events of PD-1 and PD-L1 inhibitors in clinical trials: a systematic review and meta-analysis. JAMA Oncol. 2019;5(7):1008–19.
Xiao BY, Lin GH, Zhao YX, Wang BC. The efficacy and safety of PD-1/PD-L1 inhibitors in breast cancer: a systematic review and meta-analysis. Transl Cancer Res. 2020;9(6):3804–18.
Xu D, Liu H, Xiang M, Feng A, Tian M, Li D, et al. The relationship between pneumonitis and programmed cell death-1/programmed cell death ligand 1 inhibitors among cancer patients: a systematic review and meta-analysis. Medicine. 2020;99(41):e22567.
Xu H, Tan P, Ai J, Zhang S, Zheng X, Liao X, et al. Antitumor activity and treatment-related toxicity associated with nivolumab plus ipilimumab in advanced malignancies: a systematic review and meta-analysis. Front Pharmacol. 2019;10:1300.
Xu H, Tan P, Zheng X, Huang Y, Lin T, Wei Q, et al. Immune-related adverse events following administration of anti-cytotoxic T-lymphocyte-associated protein-4 drugs: a comprehensive systematic review and meta-analysis. Drug Des Dev Ther. 2019;13:2215–34.
Xu M, Nie Y, Yang Y, Lu Y-T, Su Q. Risk of neurological toxicities following the use of different immune checkpoint inhibitor regimens in solid tumors: a systematic review and meta-analysis. Neurologist. 2019;24(3):75–83.
Yang L, Dong X-Z, Xing X-X, Cui X-H, Li L, Zhang L. Efficacy and safety of anti-PD-1/anti-PD-L1 antibody therapy in treatment of advanced gastric cancer or gastroesophageal junction cancer: a meta-analysis. World J Gastrointest Oncol. 2020;12(11):1346–63.
Yang Y, Pang P, Xie Z, Wang N, Liang H, Zhao L. The safety of first and subsequent lines of PD-1/PD-L1 inhibitors monotherapy in non-small cell lung cancer patients: a meta-analysis. Transl Cancer Res. 2020;9(5):3231–41.
Zhang B, Wu Q, Zhou YL, Guo X, Ge J, Fu J. Immune-related adverse events from combination immunotherapy in cancer patients: a comprehensive meta-analysis of randomized controlled trials. Int Immunopharmacol. 2018;63:292–8.
Zhang B, Zhou YL, Chen X, Wang Z, Wang Q, Ju F, et al. Efficacy and safety of CTLA-4 inhibitors combined with PD-1 inhibitors or chemotherapy in patients with advanced melanoma. Int Immunopharmacol. 2019;68:131–6.
Zhang C, Zhang S, Xu D, Liu R, Zhu Q, Zhao Y, et al. Incidence risk of PD-1/PD-L1 related diarrhea in non-small cell lung cancer (NSCLC) patients: a systematic review and meta-analysis. Cancer Manag Res. 2019;11:3957–69.
Zhang H, Shen J, Yi L, Zhang W, Luo P, Zhang J. Efficacy and safety of ipilimumab plus chemotherapy for advanced lung cancer: a systematic review and meta-analysis. J Cancer. 2018;9(23):4556–67.
Zhang Q, Huo G-W, Zhang H-Z, Song Y. Efficacy of pembrolizumab for advanced/metastatic melanoma: a meta-analysis. Open Med. 2020;15(1):447–56.
Zhang S, Zhou Z, Wang L, Li M, Zhang F, Zeng X. Rheumatic immune-related adverse events associated with immune checkpoint inhibitors compared with placebo in oncologic patients: a systemic review and meta-analysis. Therap Adv Chron Dis. 2021;12:2040622320976996.
Zhang X, Chen L, Zhao Y, Yin H, Ma H, He M. Safety and efficacy in relapsed or refractory classic hodgkin’s lymphoma treated with PD-1 inhibitors: a meta-analysis of 9 prospective clinical trials. Biomed Res Int. 2019;2019:9283860.
Zhao L, Yu J, Wang J, Li H, Che J, Cao B. Risk of immune-related diarrhea with PD-1/PD-L1 inhibitors in different cancer types and treatment regimens. J Cancer. 2020;11(1):41–50.
Zhou H, Fu X, Li Q, Niu T. Safety and efficacy of anti-PD-1 monoclonal antibodies in patients with relapsed or refractory lymphoma: a meta-analysis of prospective clinic trails. Front Pharmacol. 2019;10:387.
Ziogas IA, Evangeliou AP, Giannis D, Hayat MH, Mylonas KS, Tohme S, et al. The role of immunotherapy in hepatocellular carcinoma: a systematic review and pooled analysis of 2,402 patients. Oncologist. 2021;26(6):E1036–49.
Xin YuJ, Hubbard-Lucey VM, Tang J. Immuno-oncology drug development goes global. Nat Rev Drug Discov. 2019;18(12):899–900.
Wang DY, Salem JE, Cohen JV, Chandra S, Menzer C, Ye F, et al. Fatal toxic effects associated with immune checkpoint inhibitors: a systematic review and meta-analysis. JAMA Oncol. 2018;4(12):1721–8.
Robert C. A decade of immune-checkpoint inhibitors in cancer therapy. Nat Commun. 2020;11(1):3801.
Raschi E, Mazzarella A, Ippazio CA, Bendinelli N, Forcesi E, Tuccori M, et al. Toxicities with immune checkpoint inhibitors: emerging priorities from disproportionality analysis of the FDA adverse event reporting system. Targ Oncol. 2019;14:205–21.
Raschi E, Gatti M, Gelsomino F, Ardizzoni A, Poluzzi E, De Ponti F. Lessons to be learnt from real-world studies on immune-related adverse events with checkpoint inhibitors: a clinical perspective from pharmacovigilance. Target Oncol. 2020;15:449–66. https://doi.org/10.1007/s11523-020-00738-6.
Brahmer JR, Abu-Sbeih H, Ascierto PA, Brufsky J, Cappelli LC, Cortazar FB, et al. Society for Immunotherapy of Cancer (SITC) clinical practice guideline on immune checkpoint inhibitor-related adverse events. J Immunother Cancer. 2021;9(6): e002435. https://doi.org/10.1136/jitc-2021-002435.
Schneider BJ, Naidoo J, Santomasso BD, Lacchetti C, Adkins S, Anadkat M, et al. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: ASCO guideline update. J Clin Oncol. 2021;39(36):4073–126. https://doi.org/10.1200/JCO.21.01440.
Acknowledgements
The authors would like to acknowledge Risa Shorr, MLS, for her assistance and expertise in developing their search strategy and conducting the literature search.
Author information
Authors and Affiliations
Contributions
Conception and design of the study: SK, PT, BH, CL, DB, XW. Abstract screening: SM, DP, KA, PT and SK. Data collection: SM, DP and KA. Overlap management, data synthesis and interpretation: SK, PT, SM, DP, KA. Drafting the article: SM and SK. Critical revision of the article: All authors. Final approval of the version to be published: All authors.
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this manuscript
Conflicts of interest/competing interests
Brian Hutton has received honoraria from Eversana for the provision of scientific advice on methods for evidence synthesis. Dominick Bosse has received honoraria for consultations or presentations from Pfizer, BMS, AstraZeneca, AMGEN, IPSEN, Bayer, AbbVie, Eisai and Merck. Salmaan Kanji, Sydney Morin, Kyla Agtarap, Debanjali Purkayastha, Pierre Thabet, Xiang Wang and Carole Lunny declare they have no conflicts of interest that might be relevant to the contents of this manuscript.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kanji, S., Morin, S., Agtarap, K. et al. Adverse Events Associated with Immune Checkpoint Inhibitors: Overview of Systematic Reviews. Drugs 82, 793–809 (2022). https://doi.org/10.1007/s40265-022-01707-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-022-01707-1