Abstract
Eltrombopag is an orally available thrombopoietin receptor agonist indicated for the treatment of immune thrombocytopenia (ITP). Beyond the effect on megakaryopoiesis, the drug also showed a stimulating effect on the hematopoietic stem cell with consistent clinical efficacy in aplastic anemia (AA) and myelodysplastic syndromes (MDS). Eltrombopag is highly effective in ITP and less so in AA and MDS. This observation underlines the importance of residual normal hematopoiesis, which is maximal in ITP, minimal/absent in AA, and dysregulated in MDS. In ITP, the drug at 50–75 mg daily induced up to 85% responses both in clinical trials and real-life studies, with the possibility of tapering and discontinuation. In AA, eltrombopag at 150 mg daily was effective in about 40% of cases relapsed/refractory to standard immunosuppression or ineligible for bone marrow transplant. In MDS, the drug seems less effective, with responses in about a quarter of patients at various schedules. The efficacy of eltrombopag in ITP, AA, and MDS suggests the existence of common immune-pathological mechanisms in these diseases, including autoimmunity against peripheral blood cells and bone marrow precursors, as well as a possible evolution of one condition into the other. Additional mechanisms of action emerging from the clinical use of eltrombopag include modulation of T-regulatory cells, restoration of Fc-γ receptor balance in phagocytes, and an iron-mobilizing effect. In this review, we analyzed the most recent literature on eltrombopag use and efficacy in patients with ITP, AA, and MDS, exploring the basis for different dosing, combined treatments, and discontinuation in each context.

Similar content being viewed by others
References
Gonzalez-Porras JR, Bastida JM, et al. Eltrombopag in immune thrombocytopenia: efficacy review and update on drug safety. Ther Adv Drug Saf. 2018;9:263–85.
Gill H, Wong RSM, et al. From chronic immune thrombocytopenia to severe aplastic anemia: recent insights into the evolution of eltrombopag. Ther Adv Hematol. 2017;8:159–74.
Svensson T, Chowdhury O, et al. A pilot phase I dose finding safety study of the thrombopoietin-receptor agonist, eltrombopag, in patients with myelodysplastic syndrome treated with azacitidine. Eur J Haematol. 2014;93:439–45.
Swaminathan M, Borthakur G, et al. A phase 2 clinical trial of eltrombopag for treatment of patients with myelodysplastic syndromes after hypomethylating-agent failure. Leuk Lymphoma. 2019;18:1–7.
Erickson-Miller CL, DeLorme E, Tian SS, et al. Discovery and characterization of a selective, nonpeptidyl thrombopoietin receptor agonist. Exp Hematol. 2005;33:85–93.
Barcellini W. The relationship between idiopathic cytopenias/dysplasias of uncertain significance (ICUS/IDUS) and autoimmunity. Expert Rev Hematol. 2017;10:649–57.
Barcellini W, Fattizzo B, et al. Clinical evolution of autoimmune cytopenias to idiopathic cytopenias/ dysplasias of uncertain significance (ICUS/IDUS) and bone marrow failure syndromes. Am J Hematol. 2017;92:E26–9.
Olnes MJ, Scheinberg P, Calvo KR, et al. Eltrombopag and improved hematopoiesis in refractory aplastic anemia. N Engl J Med. 2012;367:11–9.
US FDA. Promacta (eltrombopag) tablets: US prescribing information. 2014. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/022291s012lbl.pdf. Accessed Jan 2019.
Wire MB, Bruce J, Gauvin J, et al. A randomized, open-label, 5-period, balanced crossover study to evaluate the relative bioavailability of eltrombopag powder for oral suspension (PfOS) and tablet formulations and the effect of a high-calcium meal on eltrombopag pharmacokinetics when administered with or 2 hours before or after PfOS. Clin Ther. 2012;34:699–709.
Deng Y, Madatian A, Wire MB, et al. Metabolism and disposition of eltrombopag, an oral, nonpeptide thrombopoietin receptor agonist, in healthy human subjects. Drug Metab Dispos. 2011;39:1734–46.
Allred AJ, Bowen CJ, Park JW, et al. Eltrombopag increases plasma rosuvastatin exposure in healthy volunteers. Br J Clin Pharmacol. 2011;72:321–9.
Lambert MP, Gernsheimer TB. Clinical updates in adult immune thrombocytopenia. Blood. 2017;129:2829–35.
Nieswandt B, Bergmeier W, Rackebrandt K, et al. Identification of critical antigen-specific mechanisms in the development of immune thrombocytopenic purpura in mice. Blood. 2000;96:2520–7.
Chang M, Nakagawa PA, Williams SA, et al. Immune thrombocytopenic purpura (ITP) plasma and purified ITP monoclonal autoantibodies inhibit megakaryocytopoiesis in vitro. Blood. 2003;102:887–95.
Leytin V, Mykhaylov S, Starkey AF, et al. Intravenous immunoglobulin inhibits antiglycoprotein IIb-induced platelet apoptosis in a murine model of immune thrombocytopenia. Br J Haematol. 2006;133:78–82.
Sandler SG. Review: immune thrombocytopenic purpura: an update for immunohematologists. Immunohematology. 2004;20:112–7.
Kuwana M, Okazaki Y, Ikeda Y. Splenic macrophages maintain the anti- platelet autoimmune response via uptake of opsonized platelets in patients with immune thrombocytopenic purpura. J Thromb Haemost. 2009;7:322–9.
Qiu J, Liu X, Li X, et al. CD8(+) T cells induce platelet clearance in the liver via platelet desialylation in immune thrombocytopenia. Sci Rep. 2016;6:27445.
Mithoowani S, Gregory-Miller K, Goy J, et al. High-dose dexamethasone compared with prednisone for previously untreated primary immune thrombocytopenia: a systematic review and meta-analysis. Lancet Haematol. 2016;3:e489–96.
Wei Y, Ji XB, Wang YW, et al. High-dose dexamethasone vs prednisone for treatment of adult immune thrombocytopenia: a prospective multicenter randomized trial. Blood. 2016;127:296–302.
Bae SH, Ryoo H, Lee WS, Joo YD, Lee KH, Lee J, et al. High dose dexamethasone vs. conventional dose prednisolone for adults with immune thrombocytopenia: a prospective multicenter phase III trial. Blood. 2010;116:3687.
Godeau B, Caulier MT, Decuypere L, et al. Intravenous immunoglobulin for adults with autoimmune thrombocytopenic purpura: results of a randomized trial comparing 0.5 and 1 g/kg b.w. Br J Haematol. 1999;107:716–9.
Zaja F, Baccarani M, Mazza P, et al. Dexamethasone plus rituximab yields higher sustained response rates than dexamethasone monotherapy in adults with primary immune thrombocytopenia. Blood. 2010;115:2755–62.
Mikhael J, Northridge K, Lindquist K, et al. Short-term and long-term failure of laparoscopic splenectomy in adult immune thrombocytopenic purpura patients: a systematic review. Am J Hematol. 2009;84:743–8.
Steurer M, Quittet P, Papadaki HA, et al. A large observational study of patients with primary immune thrombocytopenia receiving romiplostim in European clinical practice. Eur J Haematol. 2017;98:112–20.
Gonzalez-Porras JR, Mingot-Castellano ME, Andrade MM, et al. Use of eltrombopag after romiplostim in primary immune thrombocytopenia. Br J Haematol. 2015;169:111–6.
George JN, Mathias SD, Go RS, et al. Improved quality of life for romiplostim-treated patients with chronic immune thrombocytopenic purpura: results from two randomized, placebo-controlled trials. Br J Haematol. 2009;144:409–15.
Bussel JB, Cheng G, Saleh MN, et al. Eltrombopag for the treatment of chronic idiopathic thrombocytopenic purpura. N Engl J Med. 2007;357:2237–47.
Bussel J, Provan D, Shamsi T, et al. Effect of eltrombopag on platelet counts and bleeding during treatment of chronic idiopathic thrombocytopenic purpura: a randomised, double-blind, placebo-controlled trial. Lancet. 2009;373:641–8.
Cheng G, Saleh MN, Marcher C, et al. Eltrombopag for management of chronic immune thrombocytopenia (RAISE): a 6-month, randomised, phase 3 study. Lancet. 2011;377:393–402.
Bussel JB, Saleh MN, Vasey SY, et al. Repeated short-term use of eltrombopag in patients with chronic immune thrombocytopenia (ITP). Br J Haematol. 2013;160:538–46.
Saleh MN, Bussel JB, Cheng G, EXTEND Study Group, et al. Safety and efficacy of eltrombopag for treatment of chronic immune thrombocytopenia: results of the long-term, open-label EXTEND study. Blood. 2013;121:537–45.
Ghanima W, Cooper N, Rodeghiero F, Godeau B, Bussel JB. Thrombopoietin receptor agonists: ten years later. Haematologica. 2019;104:1112–23.
Wong RSM, Saleh MN, Khelif A, et al. Safety and efficacy of long-term treatment of chronic/persistent ITP with eltrombopag: final results of the EXTEND study. Blood. 2017;130:2527–36.
Saleh MN, Bussel JB, Khelif A, et al. Improvements in patient health-related quality of life (HRQoL) with clinical efficacy in patients treated with eltrombopag: final results from the long-term, open-label extend study. Blood. 2016;128:3742.
Khelif A, Saleh MN, Salama A, et al. Changes in health-related quality of life with long-term eltrombopag treatment in adults with persistent/chronic immune thrombocytopenia: findings from the EXTEND study. Am J Hematol. 2019;94:200–8.
Tripathi AK, Shukla A, Mishra S, et al. Eltrombopag therapy in newly diagnosed steroid non-responsive ITP patients. Int J Hematol. 2014;99:413–7.
Gómez-Almaguer D, Herrera-Rojas MA, Jaime-Pérez JC, et al. Eltrombopag and high-dose dexamethasone as frontline treatment of newly diagnosed immune thrombocytopenia in adults. Blood. 2014;123:3906–8.
Bussel J, De Miguel P, Despotovic J, et al. Eltrombopag for the treatment of children with Persistent and Chronic Immune Thrombocytopenia (PETIT): a randomised, multicentre, placebo-controlled study. Lancet Haematol. 2015;2:e315–25.
Grainger JD, Locatelli F, Chotsampancharoen T, et al. Eltrombopag for children with chronic immune thrombocytopenia (PETIT2): a randomised, multicentre, placebo-controlled trial. Lancet. 2015;386:1649–58.
Kim TO, Despotovic J, Lambert MP. Eltrombopag for use in children with immune thrombocytopenia. Blood Adv. 2018;2:454–61.
Tumaini Massaro J, Chen Y, Ke Z. Efficacy and safety of thrombopoietin receptor agonists in children with chronic immune thrombocytopenic purpura: meta-analysis. Platelets. 2019;27:1–8.
González-López TJ, Alvarez-Román MT, Pascual C, et al. Eltrombopag safety and efficacy for primary chronic immune thrombocytopenia in clinical practice. Eur J Haematol. 2016;97:297–302.
Depre F, Aboud N, Mayer B, et al. Efficacy and tolerability of old and new drugs used in the treatment of immune thrombocytopenia: results from a long-term observation in clinical practice. PLoS One. 2018;13:e0198184.
Mazza P, Minoia C, Melpignano A, et al. The use of thrombopoietin-receptor agonists (TPO-RAs) in immune thrombocytopenia (ITP): a “real life” retrospective multicenter experience of the Rete Ematologica Pugliese (REP). Ann Hematol. 2016;95:239–44.
Eser A, Toptas T, Kara O, et al. Efficacy and safety of eltrombopag in treatment-refractory primary immune thrombocytopenia: a retrospective study. Blood Coagul Fibrinolysis. 2016;27:47–52.
Mingot-Castellano ME, Caparrós IS, Fernández F, et al. Treatment characteristics, efficacy and safety of thrombopoietin analogues in routine management of primary immune thrombocytopenia. Blood Coagul Fibrinolysis. 2018;29:374–80.
Arai Y, Matsui H, Jo T, et al. Comparison of treatments for persistent/chronic immune thrombocytopenia: a systematic review and network meta-analysis. Platelets. 2018;3:1–11.
González-López TJ, Pascual C, Álvarez-Román MT, et al. Successful discontinuation of eltrombopag after complete remission in patients with primary immune thrombocytopenia. Am J Hematol. 2015;90:E40–3.
Mahévas M, Fain O, Ebbo M, et al. The temporary use of thrombopoietin-receptor agonists may induce a prolonged remission in adult chronic immune thrombocytopenia. Results of a French observational study. Br J Haematol. 2014;165:865–9.
Al-Samkari H, Kuter DJ. An alternative intermittent eltrombopag dosing protocol for the treatment of chronic immune thrombocytopenia. Br J Clin Pharmacol. 2018;84:2673–7.
González-López TJ, Fernández-Fuertes F, Hernández-Rivas JA, et al. Efficacy and safety of eltrombopag in persistent and newly diagnosed ITP in clinical practice. Int J Hematol. 2017;106:508–16.
Uto Y, Fujiwara S, Arai N, et al. Age and bone marrow cellularity are associated with response to eltrombopag in Japanese Adult Immune Thrombocytopenia patients: a retrospective single-center study. Rinsho Byori. 2015;63:548–56.
Al-Samkari H, Kuter DJ, et al. Thrombopoietin level predicts response to treatment with eltrombopag and romiplostim in immune thrombocytopenia. Am J Hematol. 2018;93:1501–8.
Fattizzo B, Pasquale R, Carpenedo M, et al. Bone marrow characteristics predict outcome in a multicenter cohort of primary immune thrombocytopenia patients treated with thrombopoietin analogues. Haematologica. 2019. https://doi.org/10.3324/haematol.2019.216804.
Bacigalupo A. How I treat acquired aplastic anemia. Blood. 2017;129:1428–36.
Camitta BM, Rappeport JM, Parkman R, et al. Selection of patients for bone marrow transplantation in severe aplastic anemia. Blood. 1975;45:355–63.
Wang Y. Telomere length, expression of MRE11 and Ku80 in patients with aplastic anemia and their correlation with pathogenesis. Zhongguo Shi Yan Xue Ye Xue Za Zhi. 2017;25:503–9.
Killick SB, Bown N, Cavenagh J, et al. British Society for Standards in Haematology. Guidelines for the diagnosis and management of adult aplastic anaemia. Br J Haematol. 2016;172:187–207.
Scheinberg P, Nunez O, Weinstein B, et al. Horse versus rabbit antithymocyte globulin in acquired aplastic anemia. N Engl J Med. 2011;365:430–8.
Calado RT, Yewdell WT, Wilkerson KL, et al. Sex hormones, acting on the TERT gene, increase telomerase activity in human primary hematopoietic cells. Blood. 2009;114:2236–43.
Townsley DM, Dumitriu B, Liu D, et al. Danazol treatment for telomere diseases. N Engl J Med. 2016;374:1922–31.
Bacigalupo A, Chaple M, Hows J, et al. Treatment of aplastic anemia (AA) with antilymphocyte globulin (ALG) and methylprednisolone (MPred) with or without androgens: a randomized trial from the EBMT SAA working party. Br J Haematol. 1993;83:145–51.
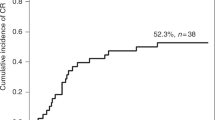
Desmond R, Townsley DM, Dumitriu B, et al. Eltrombopag restores trilineage hematopoiesis in refractory severe aplastic anemia that can be sustained on discontinuation of drug. Blood. 2014;123:1818–25.
Townsley DM, Scheinberg P, Winkler T, et al. Eltrombopag added to standard immunosuppression for aplastic anemia. N Engl J Med. 2017;376:1540–50.
Winkler T, Fan X, Cooper J, et al. Treatment optimization and genomic outcomes in refractory severe aplastic anemia treated with eltrombopag. Blood. 2019;133(24):2575–85.
Ecsedi M, Lengline É, Knol-Bout C, et al. Use of eltrombopag in aplastic anemia in Europe. Ann Hematol. 2019;98:1341–50.
Hwang YY, Gill H, Chan TSY, et al. Eltrombopag in the management of aplastic anaemia: real-world experience in a non-trial setting. Hematology. 2018;23:399–404.
Lengline E, Drenou B, Peterlin P, et al. Nationwide survey on the use of eltrombopag in patients with severe aplastic anemia: a report on behalf of the French Reference Center for Aplastic Anemia. Haematologica. 2018;103:212–20.
Fattizzo B, Kulasekararaj AG, et al. Clinical and morphologic predictors of outcome in older aplastic anemia patients treated with eltrombopag. Haematologica. 2019. https://doi.org/10.3324/haematol.2019.216374.
Mc Cormack PL. Eltrombopag: a review of its use in patients with severe aplastic anaemia. Drugs. 2015;75:525–31.
Vaht K, Göransson M, Carlson K, et al. Incidence and outcome of acquired aplastic anemia: real-world data from patients diagnosed in Sweden from 2000–2011. Haematologica. 2017;102:1683–90.
De Planque MM, Bacigalupo A, Wursch A, et al. Long term follow-up of severe aplastic anaemia patients treated with antithymocyte globulin. Br J Haematol. 1989;73:121–6.
Townsley DM, Dumitriu B, Young NS. Bone marrow failure and the telomeropathies. Blood. 2014;124:2775–83.
Lane AA, Odejide O, Kopp N, et al. Low frequency clonal mutations recoverable by deep sequencing in patients with aplastic anemia. Leukemia. 2013;27:968–71.
Yoshizato T, Dumitriu B, Hosokawa K, et al. Somatic mutations and clonal hematopoiesis in aplastic anemia. N Engl J Med. 2015;373:35–47.
Kulasekararaj AG, Jiang J, Smith AE, et al. Somatic mutations identify a subgroup of aplastic anemia patients who progress to myelodysplastic syndrome. Blood. 2014;124:2698–704.
Young NS, Abkowitz JL, Luzzatto L. New insights into the pathophysiology of acquired cytopenias. Hematol Am Soc Hematol Educ Progr 2000;18–38.
Fattizzo B, Dunlop A, Ireland R, et al. Clinical significance of PNH clones in 3085 patients with cytopenia: a large single-center experience. Hematologica. 2018. Abstract PF304–215846.
Greenberg PL, Tuechler H, Schanz J, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120:2454–65.
Sekeres MA. The epidemiology of myelodysplastic syndromes. Hematol Oncol Clin N Am. 2010;24:287–94.
Parmentier S, Schetelig J, Lorenz K, et al. Assessment of dysplastic hematopoiesis: lessons from healthy bone marrow donors. Haematologica. 2012;97:723–30.
Matsuda A, Germing U, Jinnai I, et al. Improvement of criteria for refractory cytopenia with multilineage dysplasia according to the WHO classification based on prognostic significance of morphological features in patients with refractory anemia according to the FAB classification. Leukemia. 2007;21:6782686.
Bennett JM, Orazi A, et al. Diagnostic criteria to distinguish hypocellular acute myeloid leukemia from hypocellular myelodysplastic sindrome and aplastic anemia: recommendations for a standardized approach. Haematologica. 2009;94:2642268.
Della Porta MG, Gallì A, Bacigalupo A, et al. Clinical effects of driver somatic mutations on the outcomes of patients with myelodysplastic syndromes treated with allogeneic hematopoietic stem-cell transplantation. J Clin Oncol. 2016;34:3627–37.
Santini V, Schemenau J, Levis A, et al. Can the revised IPSS predict response to erythropoietic-stimulating agents in patients with classical IPSS low or intermediate-1 MDS? Blood. 2013;122:2286–8.
Alessandrino EP, Amadori S, Barosi G, et al. Evidence- and consensus-based practice guidelines for the therapy of primary myelodysplastic syndromes. A statement from the Italian Society of Hematology. Haematologica. 2002;87:1286–306.
Li W, Morrone K, Kambhampati S, et al. Thrombocytopenia in MDS: epidemiology, mechanisms, clinical consequences and novel therapeutic strategies. Leukemia. 2016;30:536–44.
Sekeres MA, Kantarjian H, Fenaux P, et al. Subcutaneous or intravenous administration of romiplostim in thrombocytopenic patients with lower risk myelodysplastic syndromes. Cancer. 2011;117:992–1000.
Oliva EN, Santini V, Alati C, et al. Quality of life in patients with lower risk myelodysplastic syndromes with severe thrombocytopenia treated with eltrombopag: interim results of a randomized, placebo-controlled prospective trial [abstract]. Haematologica. 2015;100:575.
Kantarjian HM, Giles FJ, Greenberg PL, et al. Phase 2 study of romiplostim in patients with low- or intermediate-risk myelodys-plastic syndrome receiving azacitidine therapy. Blood. 2010;116:3163–70.
Greenberg PL, Garcia-Manero G, Moore M, et al. A randomized controlled trial of romiplostim in patients with low- or intermediate-risk myelodysplastic syndrome receiving decitabine. Leuk Lymphoma. 2013;54:321–8.
Wang ES, Lyons RM, Larson RA, et al. A randomized, double-blind, placebo-controlled phase 2 study evaluating the efficacy and safety of romiplostim treatment of patients with low or intermediate-1 risk myelodysplastic syndrome receiving lenalidomide. J Hematol Oncol. 2012;5:71.
Mavroudi I, Pyrovolaki K, Pavlaki K, et al. Effect of the nonpeptide thrombopoietin receptor agonist eltrombopag on megakaryopoiesis of patients with lower risk myelodysplastic syndrome. Leuk Res. 2011;35:323–8.
Oliva EN, Alati C, Santini V, et al. Eltrombopag versus placebo for low-risk myelodysplastic syndromes with thrombocytopenia (EQoL-MDS): phase 1 results of a single-blind, randomised, controlled, phase 2 superiority trial. Lancet Haematol. 2017;4:e127–36.
Mittelman M, Platzbecker U, Afanasyev B, et al. Eltrombopag for advanced myelodysplastic syndromes or acute myeloid leukaemia and severe thrombocytopenia (ASPIRE): a randomised, placebo-controlled, phase 2 trial. Lancet Haematol. 2018;5:e34–43.
Platzbecker U, Wong RS, Verma A, et al. Safety and tolerability of eltrombopag versus placebo for treatment of thrombocytopenia in patients with advanced myelodysplastic syndromes or acute myeloid leukaemia: a multicentre, randomised, placebo-controlled, double-blind, phase 1/2 trial. Lancet Haematol. 2015;2:e417–26.
Dickinson M, Cherif H, et al. Azacitidine with or without eltrombopag for first-line treatment of intermediate- or high-risk MDS with thrombocytopenia. Blood. 2018;132:2629–38.
Sekeres MA, Giagounidis A, Kantarjian H, et al. Development and validation of a model to predict platelet response to romiplostim in patients with lower-risk myelodysplastic syndromes. Br J Haematol. 2014;167:337–45.
Bao W, Bussel JB, Heck S, et al. Improved regulatory T-cell activity in patients with chronic immune thrombocytopenia treated with thrombopoietic agents. Blood. 2010;116:4639–45.
Liu XG, Liu S, Feng Q, et al. Thrombopoietin receptor agonists shift the balance of Fcγ receptors toward inhibitory receptor IIb on monocytes in ITP. Blood. 2016;128:852–61.
Roth M, Will B, Simkin G, et al. Eltrombopag inhibits the proliferation of leukemia cells via reduction of intracellular iron and induction of differentiation. Blood. 2012;120:386–94.
Lambert MP, Witmer CM, Kwiatkowski JL, et al. Therapy induced iron deficiency in children treated with eltrombopag for immune thrombocytopenia. Am J Hematol. 2017;92:E88–91.
Bastian TW, Duck KA, Michalopoulos GC, et al. Eltrombopag, a thrombopoietin mimetic, crosses the blood–brain barrier and impairs iron-dependent hippocampal neuron dendrite development. J Thromb Haemost. 2017;15:565–74.
Pecci A, Gresele P, Klersy C, et al. Eltrombopag for the treatment of the inherited thrombocytopenia deriving from MYH9 mutations. Blood. 2010;116:5832–7.
Fiore M, Saut N, Alessi MC, et al. Successful use of eltrombopag for surgical preparation in a patient with ANKRD26-related thrombocytopenia. Platelets. 2016;27:828–9.
Gerrits AJ, Leven EA, Frelinger AL 3rd, et al. Effects of eltrombopag on platelet count and platelet activation in Wiskott–Aldrich syndrome/X-linked thrombocytopenia. Blood. 2015;126:1367–78.
Vlachodimitropoulou E, Chen YL, Garbowski M, et al. Eltrombopag: a powerful chelator of cellular or extracellular iron(III) alone or combined with a second chelator. Blood. 2017;130:1923–33.
Punzo F, Tortora C, Argenziano M, et al. Iron chelating properties of Eltrombopag: investigating its role in thalassemia-induced osteoporosis. PLoS One. 2018;13:e0208102.
Zhao Z, Sun Q, Sokoll LJ, et al. Eltrombopag mobilizes iron in patients with aplastic anemia. Blood. 2018;131:2399–402.
Fattizzo B, Cavallaro F, Milesi G, Barcellini W. Iron mobilization in a real life cohort of aplastic anemia patients treated with eltrombopag. Am J Hematol. 2019. https://doi.org/10.1002/ajh.25550[Epub ahead of print].
Caillon H, Peterlin P, Chevallier P, et al. Eltrombopag induces major non-toxic hypersiderraemia. Br J Haematol. 2019. https://doi.org/10.1111/bjh.15863[Epub ahead of print].
Kao JK, Wang SC, Ho LW, et al. Chronic iron overload results in impaired bacterial killing of THP-1 derived macrophage through the inhibition of lysosomal acidification. PLoS One. 2016;31(11):e0156713.
Weiss G. Iron and immunity: a double-edged sword. Eur J Clin Investig. 2002;32(Suppl 1):70–8.
Arber DA, Orazi A, Hasserjian R, et al. The 2016 revision to the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia. Blood. 2016;127:2391–405.
Malcovati L, Cazzola M. The shadowlands of MDS: idiopathic cytopenias of undetermined significance (ICUS) and clonal hematopoiesis of indeterminate potential (CHIP). Hematol Am Soc Hematol Educ Progr. 2015;2015:299–307.
Rafferty M, Leach M. Hypomegakaryocytic thrombocytopenia and increased number of PNH-phenotype cells—an emerging subgroup of myelodysplastic syndrome showing frequent response to immunosuppression. Br J Haematol. 2018;182:152–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this manuscript.
Conflict of interest
Bruno Fattizzo has received consulting honoraria from Apellis. Giorgia Levati and Ramona Cassin declare that they have no conflict of interest that might be relevant to the contents of this manuscript. Wilma Barcellini has received consulting fee or honoraria from Bioverativ, Apellis, Agios, Alexion, and Novartis, and has received speaker honoraria from Novartis.
Rights and permissions
About this article
Cite this article
Fattizzo, B., Levati, G., Cassin, R. et al. Eltrombopag in Immune Thrombocytopenia, Aplastic Anemia, and Myelodysplastic Syndrome: From Megakaryopoiesis to Immunomodulation. Drugs 79, 1305–1319 (2019). https://doi.org/10.1007/s40265-019-01159-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-019-01159-0