Abstract
Acinetobacter baumannii is a leading cause of healthcare-associated infections worldwide. Because of various intrinsic and acquired mechanisms of resistance, most β-lactam agents are not effective against many strains, and carbapenems have played an important role in therapy. Recent trends show many infections are caused by carbapenem-resistant or even extensively drug-resistant (XDR) strains, for which effective therapy is not well established. Evidence to date suggests that colistin constitutes the backbone of therapy, but the unique pharmacokinetic properties of colistin have led many to suggest the use of combination antimicrobial therapy. However, the combination of agents and dosing regimens that delivers the best clinical efficacy while minimizing toxicity is yet to be defined. Carbapenems, sulbactam, rifampin and tigecycline have been the most studied in the context of combination therapy. Most data regarding therapy for invasive, resistant A. baumannii infections come from uncontrolled case series and retrospective analyses, though some clinical trials have been completed and others are underway. Early institution of appropriate antimicrobial therapy is shown to consistently improve survival of patients with carbapenem-resistant and XDR A. baumannii infection, but the choice of empiric therapy in these infections remains an open question. This review summarizes the most current knowledge regarding the epidemiology, mechanisms of resistance, and treatment considerations of carbapenem-resistant and XDR A. baumannii.
Similar content being viewed by others
Acinetobacter baumannii exhibits multiple mechanisms of multi-class resistance and represents a clinical challenge due to extensively-resistant nosocomial infections occurring worldwide. |
Polymyxins, tigecycline and sulbactam are the most commonly used therapies in carbapenem-resistant and extensively drug-resistant A. baumannii infections, with published results varying on efficacy of each. |
Combination therapy for A. baumannii infections with first-line agents and also glycopeptides, rifamycins and fosfomycin has been studied and may be of benefit. |
1 Introduction
Acinetobacter species have been increasingly recognized as major pathogens implicated in hospital-acquired and healthcare-associated infections worldwide. The common presentations of infections include ventilator-associated pneumonia, bloodstream infection, wound infection and urinary tract infection [1]. It is one of the most common etiologic pathogens causing ventilator-associated pneumonia in the USA [2]. The genus Acinetobacter comprises more than 30 genomic species which are aerobic, non-motile, catalase-positive and oxidase-negative coccobacilli. Among these genomic species, the most clinically relevant species is Acinetobacter baumannii, both in terms of relative virulence and the degree of multidrug resistance. In addition, Acinetobacter nosocomialis (genomospecies 13TU) and Acinetobacter pittii (genomospecies 3) are increasingly implicated in hospital-acquired and healthcare-associated infections [3]. However, the standard biochemical identification methods employed in clinical microbiology laboratories do not differentiate A. baumannii from A. nosocomialis, A. pittii or Acinetobacter calcoaceticus, the last of which is considered to be an environmental pathogen of little clinical significance. Identification of A. baumannii requires the use of at least one genetic method, which is usually not available in clinical laboratories. It therefore should be kept in mind when reviewing the literature that A. baumannii, especially in clinical studies, may refer to the actual A. baumannii as the genomic species or, more frequently, A. baumannii complex, which includes all of the four genomic species above.
The most prominent feature of A. baumannii is its ability to develop resistance to multiple classes of antimicrobial agents. While the term multidrug resistance (MDR) is often used to describe this phenomenon, MDR technically refers to non-susceptibility to one or more agents in three or more antimicrobial categories [4], which may apply to even relatively antimicrobial-susceptible isolates in A. baumannii. For example, resistance to ceftriaxone, ciprofloxacin and trimethoprim–sulfamethoxazole is sufficient to define an isolate as MDR, in which case, many treatment options are still available. In contrast, extensive drug resistance refers to non-susceptibility to one or more agents in all but two or fewer antimicrobial categories [4] and is more clinically relevant. For instance, an isolate which is susceptible to colistin and tigecycline but resistant to all other categories tested would be defined as extensively drug resistant (XDR). These XDR isolates are increasingly encountered in clinical practice [5]. Non-susceptibility to all antimicrobial agents tested defines pan-drug resistance. In addition, carbapenem resistance merits special consideration given its otherwise reliable activity against A. baumannii. Resistance to carbapenems poses a major challenge as the second-line treatment options are much less defined in their efficacy and often accompany toxicity. Carbapenem-resistant isolates are often but not always XDR, and vice versa. Therefore, attention should also be paid to the definitions of resistance used when surveying clinical studies addressing treatment of A. baumannii infections. Another key feature of A. baumannii is its ability to survive on dry surfaces for prolonged periods. This unique trait further facilitates its dissemination in the healthcare environment, often leading to outbreaks [6].
This review will describe the current epidemiology of antimicrobial resistance in A. baumannii, mechanisms underlying resistance, and treatment considerations for A. baumannii infections.
2 Epidemiology
Acinetobacter spp. may cause a spectrum of infections, but most commonly affects the lower respiratory tract, followed by blood and wound [1]. Acinetobacter isolates collected randomly from hospitals across the USA in 2010 showed that the majority of the isolates (57.6 %) were from the respiratory tract, followed by bloodstream (23.9 %) and skin or wound (9.1 %) [5]. It was the third most common pathogen causing ventilator-associated pneumonia (8.4 % of cases) and the ninth most common cause of central line-associated bloodstream infection (2.2 %) in US hospitals between 2006 and 2007 [7]. Between 2009 and 2010, it caused 6.6 % of ventilator-associated pneumonia (ranking fifth) and 2.1 % of central line-associated bloodstream infection (ranking thirteenth) [2]. Therefore, most clinical data regarding therapy of Acinetobacter infection have been generated from cases of pneumonia and bloodstream infections. It should be noted, however, that for pneumonia and infections of other non-sterile sites, it is often difficult to distinguish colonization from true Acinetobacter infection and determine whether the affected patients require therapy directed towards this pathogen. Thus, some of the epidemiologic source data may include isolates that were not responsible for infections, but were simply colonizing ill patients, and the estimates of resistance may be biased as a result. In terms of resistance, 34 % of Acinetobacter isolates in the National Healthcare Safety Network were resistant to penicillins, cephalosporins, carbapenems, fluoroquinolones and aminoglycosides [8]. In another nationwide surveillance study conducted in the USA in 2010, 44.7 and 49.0 % were resistant to imipenem and meropenem, respectively [5]. Carbapenem resistance increased with age; it was present in 60–64 % of all isolates in the elderly (age >65 years) and 46–51 % of those in younger adults, while it was only present in 13–17 % of pediatric isolates. Resistance rates to ceftazidime, levofloxacin and tobramycin were at 52.1, 52.3, and 38.9 %, respectively; 53.9 % were MDR. Notably, 5.3 % were also resistant to colistin in vitro in this study. It is clear that over the last decade, Acinetobacter species, in particular A. baumannii, have become increasingly resistant to currently available antimicrobial agents, especially carbapenems [9].
There appears to be a wide geographic and temporal variation in the distribution of genomospecies among clinical isolates of A. baumannii complex. In a study investigating clinical isolates from any site collected from hospitals in Germany between 2005 and 2009, 51 % of A. baumannii complex isolates were identified as A. pittii, followed by A. baumannii (37 %), A. calcoaceticus (3 %) and A. nosocomialis (2 %). Of note, all imipenem-non-susceptible isolates were A. baumannii [10]. On the other hand, in a similarly designed study conducted in Taiwan in 2006, 89 % were A. baumannii, 8 % A. pittii and 3 % A. nosocomialis [11]. In the USA, A. baumannii was the most prevalent species (63 %), followed by A. nosocomialis (21 %) and A. pittii (8 %) among blood isolates collected between 1995 and 2003 [12]. However, when carbapenem-non-susceptible isolates collected more recently (2008–2009) were studied, all were A. baumannii [13]. Furthermore, in a series of A. baumannii complex bloodstream infections, A. baumannii as the genomospecies has been singled out as an independent risk factor for mortality, with attributable mortality of 59, 17, and 33 % for A. baumannii, A. nosocomialis and A. pittii, respectively [3]. Therefore, A. baumannii is the most problematic genomospecies in the A. baumannii complex both in terms of antimicrobial resistance and unfavorable clinical outcome.
3 Clinical Relevance
A. baumannii is primarily a healthcare-associated pathogen, thus the risk factors for colonization and infection by A. baumannii are also healthcare associated. The risk factors for acquisition are best studied for XDR and carbapenem-resistant isolates, and include recent exposure to antimicrobial agents (in particular carbapenems), presence of central venous catheters or urinary catheters, severity of illness, duration of hospital stay, location in an intensive care unit (ICU), larger hospital size, and recent surgery [14–17].
Mortality associated with invasive A. baumannii infection is high, especially for carbapenem-resistant cases. Crude mortality for carbapenem-resistant A. baumannii infections ranges from 16 to 76 %, as opposed to 5 to 53 % for carbapenem-susceptible infections [18]. More recently, attributable mortality of 70 % has been reported for bloodstream infections due to imipenem-resistant A. baumannii, compared with 24.5 % for imipenem-susceptible A. baumannii in Taiwan [19], and 30-day mortality of 79.8 % has been reported for carbapenem-resistant A. baumannii bloodstream infections in Korea [20]. These studies, however, did not report specific causes of death, so determination of the contribution of A. baumannii to the mortality may not be accounted for in these estimates. On the other hand, mortality as low as 2 % has been reported for A. baumannii bloodstream infections among young, previously healthy war-related trauma patients, underscoring the significant contribution of host factors to the clinical outcome of invasive A. baumannii infection [21].
Independent risk factors for mortality among patients with carbapenem-resistant A. baumannii bloodstream infections include the severity of illness, underlying malignancy, history of transplant, higher age, septic shock, concurrent pneumonia, inappropriate antimicrobial therapy, prolonged ICU stay, and renal failure, among others [19, 20, 22–25]. High mortality rates observed in patients with carbapenem-resistant A. baumannii infection are believed to be mostly due to the greater severity of illness and higher risk of receiving early inappropriate antimicrobial therapy (see Sect. 5.9) [18]. For instance, an analysis of 274 patients with A. baumannii bloodstream infection in a US health system revealed significantly higher in-hospital mortality for carbapenem- and ampicillin–sulbactam-resistant infections compared with more susceptible ones (42 vs. 29 %; p < 0.001), but after adjusting for the severity of illness, the odds of dying in the hospital were similar between the two groups. The authors postulated this may be due to the fact that risk factors for carbapenem resistance were similar to risk factors for hospital mortality [26].
4 Mechanisms of Antimicrobial Resistance
A. baumannii has an armamentarium of antimicrobial drug-resistance mechanisms it can utilize or acquire to become XDR. Certain XDR strains are epidemic in hospitals worldwide, likely because of the degree of antimicrobial resistance as well as their ability to survive environmental desiccation for many weeks [27]. Here, we will briefly review the key mechanisms underlying resistance of A. baumannii to relevant classes of antimicrobial drugs.
4.1 Cephalosporins
Most clinical isolates of A. baumannii are resistant to cephalosporins. Acinetobacter spp. intrinsically produces AmpC β-lactamase, called Acinetobacter-derived cephalosporinase (ADC) [28, 29]. Unlike most chromosomally produced AmpC β-lactamases in Gram-negative pathogens, ADC is not believed to be inducible [29]. However, expression of ADC is elevated when insertion sequence ISAba1 or ISAba125 is acquired upstream of the bla ADC gene and provides a stronger promoter activity compared with the native promoter sequence of the bla ADC gene [30, 31]. This results in elevation of cephalosporin minimum inhibitory concentrations (MICs) except cefepime, which is not a substrate of AmpC β-lactamases including ADC. Some A. baumannii isolates have been observed to produce extended-spectrum AmpC β-lactamases which can confer resistance to cefepime along with other cephalosporins [32].
A. baumannii may also become resistant to cephalosporins by producing extended-spectrum β-lactamase (ESBL). PER-type ESBL is the most commonly found ESBL in A. baumannii [33, 34], but production of VEB-type ESBL and CTX-M-type ESBL, which is the most common ESBL in Escherichia coli, has also been reported [35, 36].
4.2 Carbapenems
Several mechanisms are involved in carbapenem resistance. They include production of carbapenem-hydrolyzing β-lactamase (“carbapenemase”), reduced permeability of the outer membrane, and active efflux [37, 38]. Of these, the most significant mechanism is the production of carbapenemases, which can be either intrinsic or acquired.
A. baumannii naturally produces chromosomally encoded OXA-51-group carbapenemase at a low level. While this basal production of the OXA-51 group does not lead to clinically relevant carbapenem resistance, acquisition of a stronger promoter by transposition of ISAba1 or ISAba9 upstream of the OXA-51-group gene may lead to a moderate, clinically significant degree of carbapenem resistance [39, 40].
Among acquired carbapenemases, OXA-group enzymes are the most commonly encountered worldwide. There are five groups of acquired OXA-group carbapenemases in A. baumannii, including OXA-23, -40, -58, -143 and -235 groups [41]. Of these, the OXA-23 group is especially widely disseminated and is the most frequent cause of clinically relevant carbapenem resistance in A. baumannii [42]. Of note, OXA-group carbapenemases confer resistance to oxacillins and carbapenems, but not cephalosporins. However, isolates that acquire OXA-group carbapenemase are usually already resistant to cephalosporins because of the aforementioned mechanisms.
Non-OXA carbapenemases that have spread in Enterobacteriaceae are also being acquired by A. baumannii. The most significant metallo-β-lactamase found in this species is NDM group. Carbapenem-resistant A. baumannii producing NDM-1 has been identified worldwide since 2011 [43, 44]. Production of IMP-, VIM- and SIM-group metallo-β-lactamases has also been reported on rare occasions in this species [45–47]. Finally, A. baumannii producing KPC- and GES-group carbapenemases have been reported, but they appear to remain sporadic events at this point [48, 49].
4.3 Sulbactam
Sulbactam exerts its anti-Acinetobacter activity by binding to the penicillin-binding protein PBP2 of A. baumannii [50]. Reduced expression of PBP2 has been associated with resistance to sulbactam [51]. In addition, the role of production of non-ESBL β-lactamase TEM-1 has been suggested to contribute to sulbactam resistance of A. baumannii [52].
4.4 Rifampin
Rifampin binds to the active center of bacterial ribonucleic acid (RNA) polymerase and inhibits transcription initiation. The major mechanism underlying rifampin resistance is amino acid substitutions in the β-subunit of this target protein [53]. In addition, enzymatic modification by rifampin adenosine diphosphate (ADP) ribosyltransferase (e.g., Arr-2) and active efflux have been implicated in rifampin resistance of A. baumannii clinical isolates [53, 54].
4.5 Aminoglycosides
Aminoglycosides bind to the 16S ribosomal RNA of the 30S ribosomal subunit and inhibit protein synthesis. The most ubiquitous mechanism underlying aminoglycoside resistance in A. baumannii is production of various aminoglycoside-modifying enzymes. There are three functional groups of modifying enzymes, which include aminoglycoside acetyltransferases [e.g., AAC(6′)-Ib], aminoglycoside phosphotransferases [e.g., APH(3′)-Ia] and aminoglycoside adenylyltransferases [e.g., ANT(2″)-Ia] [55]. Commonly found aminoglycoside-modifying enzymes in A. baumannii are AAC(6′)-Ib, AAC(6′)-Ih (conferring tobramycin and amikacin resistance), AAC(3)-Ia, ANT(2″)-Ia and APH(3′)-Ia (conferring gentamicin resistance) [56, 57]. Another aminoglycoside resistance mechanism that appears to be emerging is production of 16S ribosomal RNA methyltransferase, especially ArmA. ArmA methylates a guanine residue in the aminoglycoside-binding site (A-site) of 16S ribosomal RNA (rRNA) [58]. ArmA-producing A. baumannii are highly and uniformly resistant to the aminoglycosides that are commonly used systemically (e.g., gentamicin, tobramycin and amikacin) [59, 60].
4.6 Fluoroquinolones
The primary mechanism of resistance to fluoroquinolones in A. baumannii is, as with any bacteria, amino acid substitutions in the quinolone resistance determining region (QRDR) of the DNA gyrase and topoisomerase IV, which interfere with binding of fluoroquinolones to these target proteins [36]. Overexpression of active efflux pumps may also cause moderate fluoroquinolone resistance and augment the level of resistance in strains with QRDR substitutions [61].
4.7 Colistin
Colistin targets lipid A of lipopolysaccharide for its activity, and resistance to colistin arises because of modifications of this target. The most commonly reported pathway in A. baumannii is the addition of a phosphoethanolamine moiety to the hepta-acylated lipid A, which reduces the negative charge of lipid A and lowers the affinity of colistin [62–64]. Another proposed mechanism is the loss of lipopolysaccharide, which deprives A. baumannii of the target [65].
4.8 Tetracyclines
Resistance to the tetracycline group of agents is mediated primarily by active efflux or target protection by production of Tet proteins that bind to the 70S ribosome [66]. Tigecycline, which was designed to resist the majority of these mechanisms, is still prone to efflux by Ade-type efflux pumps, which are produced by the majority of A. baumannii clinical isolates. Their overexpression therefore leads to resistance to tigecycline [67].
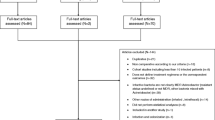
5 Treatment of Acinetobacter baumannii Infections
For infections caused by relatively antimicrobial-susceptible A. baumannii strains, there usually remain a sufficient number of safe and effective antimicrobial agents that can be used for treatment. Research has thus primarily focused on how to effectively treat XDR and carbapenem-resistant A. baumannii infections (Tables 1, 2). While various treatment approaches have been proposed through in vitro, in vivo and clinical studies, there is a hesitant consensus that a polymyxin (colistin [polymyxin E] or polymyxin B) should be included in any regimen as the backbone for treatment of infections caused by colistin-susceptible isolates and likely colistin-resistant isolates as well [68, 69]. Despite the recent trend toward polymyxins, there is some hesitancy to their use. For most other infections, polymyxins were abandoned because of their toxicity profile in the 1980s. Thus many centers and clinicians favor therapy based on other agents, including sulbactam and tigecycline, both as monotherapy and in combination, for carbapenem-resistant isolates. The variation in practice has driven some of the heterogeneous studies included here.
Of note, colistin is given as its less active prodrug colistimethate (colistin methanesulfonate) intravenously, which is then converted over time to the active drug colistin in the blood. However, most scientific papers refer to colistimethate as colistin. In this review, colistin, when appearing as part of treatment regimens, refers to colistimethate. On the other hand, the active drug colistin is used for in vitro testing of susceptibility and synergy.
5.1 Colistin
Colistin (polymyxin E) is one of the two polymyxin class agents that are approved for clinical use, the other one being polymyxin B. Polymyxins are cationic polypeptides which exert their bactericidal activity through interactions with the lipid A component of lipopolysaccharide constituting the bacterial outer membrane. For intravenous use, colistin is administered as its inactive prodrug colistin methanesulfonate, or colistimethate. Colistin is much more widely available than polymyxin B worldwide, and as a result most data in the literature regarding treatment of A. baumannii are provided for colistin rather than polymyxin B. It is worth noting that a recent retrospective study from a single center showed higher risk of nephrotoxicity with colistin compared with polymyxin B (60.4 vs. 41.8 %), though more patients in the colistin arm were on vasopressors [70]. Also worth mentioning is the confusing terminology used to describe the amount of colistimethate, with international units (IUs) used in Europe and elsewhere and milligrams of colistin base activity (CBA) used in the Americas and elsewhere. One million IU is equivalent to approximately 30 mg of CBA, which in turn corresponds to approximately 80 mg of chemical colistimethate [71]. We will use CBA throughout this review unless otherwise specified.
Colistin is active against Gram-negative bacteria, and most A. baumannii isolates remain susceptible to this agent. Among Acinetobacter clinical isolates collected from US hospitals in 2010, 94.7 % were susceptible to colistin when using the susceptibility breakpoint of ≤2 μg/mL currently endorsed by both the Clinical and Laboratory Standards Institute (CLSI) and the European Committee on Antimicrobial Susceptibility Testing (EUCAST) [5]. The antibacterial activity of colistin is best predicted by free area under the curve (AUC)/MIC (fAUC/MIC) [72]. In time-kill studies, colistin exerts a rapid bactericidal effect, but regrowth is commonly observed even at colistin concentrations exceeding the MICs [73]. In addition, subpopulations with increased tolerance to colistin concentrations higher than the MICs can be observed when high inoculums are used for testing [74]. This hetero-resistance phenomenon raises concerns about subpopulations not adequately targeted by colistin in an apparently colistin-susceptible isolate. Emergence of resistance on therapy with colistin may be related to selection for these hetero-resistant subpopulations.
Colistin and its prodrug colistimethate have unique pharmacokinetic properties [72]. Colistimethate has a relatively short terminal half-life under normal physiology because of high renal clearance, and slowly converts to colistin in the blood. Some references estimated the colistimethate half-life at 2.2 h, whereas others give a higher estimate, closer to 4.9 h. Colistin, on the other hand, undergoes tubular reabsorption and has a longer terminal half-life (14.4–18.5 h) [75]. Of note, in patients with decreased clearance, the half-life of colistimethate was prolonged proportionally more than the colistin half-life [76]. As a result, the predicted maximum plasma concentration of colistin after a 90-mg CBA-equivalent dose is only 0.6 mg/L, and only reaches 2.3 mg/L after repeated administration every 8 h in critically ill patients [77]. The colistin MICs for the majority of A. baumannii clinical isolates cluster between 0.25 and 2 μg/mL (http://mic.eucast.org), implying that patients may be exposed to subtherapeutic concentrations of colistin for a prolonged period. These data suggest that a loading dose may provide clinical benefit to patients receiving colistin. When a loading dose of 180 mg (CBA equivalent) was administered, colistin concentrations averaged 1.34 mg/L, with a wide range [75]. In another study, which included 105 critically ill patients with variable renal function, the average steady-state plasma concentration of colistin ranged from 0.48 to 9.38 mg/L, with a median of 2.36 mg/L [76]. These studies highlighted the pharmacokinetic caveats of treating patients with colistin alone, where an adequate plasma level of the active form of colistin may not be achieved for the first 1 or 2 days of therapy in the absence of a loading dose, and the therapeutic window between the colistin MICs of the infecting organisms and the plasma colistin concentration remains low even at the steady state. However, nephrotoxicity of colistin limits the potential for increasing the doses at the same time. Because of these limitations of colistin monotherapy, it is increasingly proposed that colistin should be used as part of combination regimens for clinical efficacy and prevention of resistance (see also Sect. 5.8).
Given that colistin is usually used for therapy when there are no good alternatives, clinical data on the efficacy of colistin in the treatment of XDR A. baumannii infections are scarce. Furthermore, studies suffer from inherent limitations, including the lack of suitable comparators, heterogeneity and complexity of the patients’ medical conditions, and also inconsistent dosing approaches. In a retrospective study of 35 patients with ventilator-associated pneumonia due to A. baumannii who were treated according to colistin or imipenem susceptibility, 21 received colistin (2.5–5 mg/kg/day) and 14 received imipenem (2–3 g/day) [78]. Clinical cure and in-hospital mortality rates were comparable at 57 % each and 61.9 vs. 64.2 %, respectively. Though a small study, the findings suggested that colistin might be a reasonable alternative for imipenem when A. baumannii is resistant to imipenem. On the other hand, in another study of 167 patients with invasive infections caused by carbapenem-resistant A. baumannii and treated with a polymyxin or ampicillin–sulbactam, therapy with a polymyxin was an independent risk factor for in-hospital mortality (odds ratio 2.07; p = 0.041; see also Sect. 5.2 below) [79]. There is only one prospective, randomized study that compared the efficacy of colistin and ampicillin–sulbactam among A. baumannii ventilator-associated pneumonia patients [80]. This small study of 28 patients used a dose of colistin (270 mg CBA/day, without loading dose) that was acceptable, but on the low end of the current recommended dosing [76], and high-dose ampicillin–sulbactam (27 g/day). The clinical efficacy was comparable in both groups (60.0 vs. 61.5 %). Overall, there does appear to be some efficacy of colistin when used against A. baumannii infection, which nonetheless is difficult to quantify. Given the pharmacokinetic limitations of colistin as described above and concerns over development of resistance during treatment, it is increasingly used as part of combination therapy, and, consequently, most of the efficacy data on colistin are expected to be derived in this context in the future. Efficacy data regarding colistin-containing combination therapy that are currently available are reviewed in the sections for each companion agent below.
Nebulized colistin (as its prodrug colistimethate) is often used in clinical practice, in conjunction with intravenous colistin or other regimens for the treatment of ventilator-associated pneumonia due to XDR A. baumannii. A pharmacokinetic study conducted in cystic fibrosis patients confirmed the higher and likely therapeutic colistin concentrations present in sputum following administration of nebulized colistin compared with intravenous colistin [81]. There were minimal systemic levels noted in the six patients tested, all of whom had normal renal function, suggesting a possible way to limit toxicity. However, it should be noted that bronchospasm is a known adverse event of this off-label use [82]. A recently conducted retrospective study on ventilator-associated pneumonia patients with Gram-negative isolates susceptible only to colistin reported increased clinical cure rates (69.2 vs. 54.8 %; p = 0.03) when nebulized colistin was added to the intravenous form, as compared with intravenous colistin monotherapy. The study included Klebsiella pneumoniae and Pseudomonas aeruginosa as well as A. baumannii, but A. baumannii was the predominate pathogen in both groups. There was no observed difference in ICU death between the groups [83]. In a case-control study conducted in Taiwan, patients with respiratory secretions growing MDR A. baumannii eradicated the organism sooner when they were given nebulized colistin for a median of 10.9 days, with or without intravenous colistin, compared with no nebulized colistin therapy (8.2 vs. 21.5 days; p < 0.001) [84]. There were no differences in the rates of adverse events or in-hospital mortality. A randomized, open-label trial comparing the efficacy of nebulized colistin for 100 patients with Gram-negative ventilator-associated pneumonia was conducted in Thailand [85]. In this study, A. baumannii accounted for over 60 % of the causative organisms. Favorable microbiologic outcome was noted in 60.9 % of the nebulized plus intravenous colistin group and 38.2 % of the intravenous colistin only group (p = 0.03). However, there was no difference in the rates of favorable clinical outcome (51.0 vs. 53.1 %; p = 0.84). Of note, there were numerically more bronchospasm events in the nebulized colistin group (7.8 vs. 2.0 %; p = 0.36). These data suggest that nebulized colistin expedites eradication of A. baumannii from the airway, but the true benefit to the clinical outcome of the patients, and to overall mortality, along with the risks of bronchospasm and development of resistance remain unclear.
Central nervous system (CNS) infections with A. baumannii are uncommon and are associated with neurosurgical procedures and devices. While carbapenems penetrate the CNS relatively well, colistin has been shown to have low CNS penetration [86]. Patients with severe and/or resistant A. baumannii CNS infections have been treated with intrathecal or intraventricular colistin [87]. A recent review of cases and case series showed that 72 of 81 patients treated with colistin by intrathecal/intraventricular route (in most cases with concomitant intravenous colistin) had a clinical and microbiologic cure [88]. Most of the isolates were XDR, MDR or carbapenem resistant, which explains why patients may not have been given carbapenems.
5.2 Sulbactam
Sulbactam is a synthetic β-lactamase inhibitor which has been co-formulated with ampicillin or cefoperazone to overcome β-lactamase-mediated resistance and restore the activity of the co-formulated β-lactams. In addition, sulbactam itself has affinity for penicillin-binding proteins, in particular, types 1a and 2. As a result, it possesses intrinsic activity against Acinetobacter species [89, 90]. After a 1-g intravenous dose (the standard dose in the ampicillin–sulbactam 3-g formulation), a peak serum concentration of 40–60 mg/L is achieved, with an approximate half-life of 1 h [91]. Susceptibility data are somewhat limited. An ampicillin–sulbactam susceptibility of 63.6 % was reported for Acinetobacter spp. isolates collected from US hospitals in the early 2000s [92]. However, a steady decline in the susceptibility rate of A. baumannii from 89 % in 2003 to 40 % in 2008 has also been reported from a US hospital system [93].
In mouse pneumonia models of A. baumannii, treatment with sulbactam achieved survival and clearance of the bacteria from the lungs that was comparable to imipenem, and better than colistin in one study, when the strains were not resistant to these agents [94, 95].
The only prospective, randomized study on this topic to date was conducted in Greece, where 28 patients with ventilator-associated pneumonia from XDR A. baumannii were randomized to receive ampicillin–sulbactam (9 g of sulbactam/day) or colistin (270 mg CBA/day) [80]. In this trial, the clinical response rates were comparable, with 76.8 % for ampicillin–sulbactam versus 73.3 % for colistin. Bacteriologic success rates, 14- and 28-day mortality rates and the rates of adverse events were also comparable between the two groups. Of note, all isolates were resistant to ampicillin–sulbactam and susceptible to colistin in vitro and the dose of the former was more than twice higher than the standard dose of 4 g/day. This suggests that the in vitro testing against sulbactam may not reflect clinical response and may need to be studied further to reflect the pharmacodynamics and pharmacokinetics of this higher dose.
Several observational studies have attempted to explore the efficacy of sulbactam. In a study of Acinetobacter bloodstream infections from Korea, 35 patients received cefoperazone–sulbactam and 12 received imipenem [96]. All isolates were susceptible in vitro to the agents given. The clinical response rates were comparable (77 vs. 75 %), though there was a trend towards lower 30-day mortality among those who received cefoperazone–sulbactam (20 vs. 50 %; p = 0.065). However, while pneumonia was the most common source of bacteremia in both arms, 26 % of patients in the cefoperazone–sulbactam arm had a vascular catheter-related infection. No infections in the imipenem group were catheter-related, and thus the trend toward lower mortality might be explained by a more easily removable focus of infection. In another series of A. baumannii ventilator-associated pneumonia from the USA, 14 patients were treated with ampicillin–sulbactam and 63 with imipenem [97]. The percentages of successfully treated episodes were similar in the two groups (93 vs. 83 %). There were no differences in the rates of microbiologic clearance and mortality either. Dosing information was not provided in either of these studies. Finally, a study from Brazil examined the efficacy of ampicillin–sulbactam and polymyxins (colistin or polymyxin B) against invasive carbapenem-resistant A. baumannii infections [79]. Here, 85 patients received ampicillin–sulbactam and 82 received polymyxins. Almost 30 % also received a carbapenem in both groups, despite all isolates demonstrating carbapenem resistance in vitro. Clinical response was observed in 60 % of the ampicillin–sulbactam group and 39 % of the polymyxin group, and treatment with polymyxins was an independent risk factor for in-hospital mortality (odds ratio 2.07; p = 0.04). However, the median daily dose of colistin was 5.1 million IU, corresponding to approximately 150 mg CBA, which is substantially lower than the currently recommended dose [76]. The median daily dose of ampicillin–sulbactam was 9 g.
These data suggest that the use of sulbactam-containing regimens may have a role in the treatment of infections caused by carbapenem-resistant A. baumannii that remain susceptible to sulbactam. However, a recent report suggests an apparent lack of correlation between the level of sulbactam MICs and clinical response after treatment with this agent [98]. Furthermore, the declining in vitro activity of sulbactam may limit the utility of this agent in the long term.
5.3 Tigecycline
Tigecycline is the first agent in the glycylcycline class that has been approved and marketed for clinical use. It is a derivative of minocycline and exerts its activity through inhibition of protein synthesis by binding to the 30S ribosomal subunit. Tigecycline is approved for use in complicated intra-abdominal, complicated skin and skin structure infections, and also community-acquired bacterial pneumonia in the USA. It is capable of circumventing many of the efflux and ribosomal protection mechanisms underlying tetracycline resistance, and thus has a broader spectrum of activity compared with the earlier tetracyclines [99]. A. baumannii is broadly susceptible to tigecycline as a species [100]. Resistance to tigecycline is relatively rare but may develop through overexpression of efflux pumps, especially upon exposure to this agent [37, 101, 102].
Tigecycline has unique pharmacokinetics where the large volume of distribution results in extensive tissue distribution but also a low serum peak concentration of 0.7 to 0.8 mg/L after the standard loading dose of 100 mg [103]. The use of this agent for bloodstream infection is controversial because of the low serum concentrations, and breakthrough bacteremia during therapy has been reported [102]. Suboptimal clinical outcome (56 % infection-related mortality) has been reported for patients with carbapenem-resistant A. baumannii bloodstream infection who were treated with tigecycline despite in vitro susceptibility [104]. In addition, it is generally not recommended for use in urinary tract infection since only 15–22 % is excreted unchanged in the urine [105].
Tigecycline is not approved for use in hospital-acquired pneumonia because of a phase III approval study which resulted in inferior clinical outcome in those who received tigecycline-based regimens compared with those who received imipenem-based regimens [106]. The inferiority was driven by the lower clinical response rates among those with ventilator-associated pneumonia. Among the small subset of patients who had ventilator-associated pneumonia from A. baumannii, the clinical response rates for the tigecycline group and the imipenem group were 57.1 and 94.7 %, respectively. These clinical outcome data are consistent with findings in a mouse pneumonia model comparing imipenem and tigecycline, where only imipenem reduced mortality when infection was caused by either imipenem-susceptible or intermediate A. baumannii strains. Clearance of the bacteria from the lungs was also superior with imipenem compared with tigecycline [107]. However, recent data have suggested that clinical failure in pneumonia with tigecycline may be related to poor lung penetration and decreased AUC/MIC ratios. Given this hypothesis, a phase II trial was conducted for hospital-acquired pneumonia with doses of 75 and 100 mg of tigecycline every 12 h (standard dosing is 50 mg every 12 h), compared with imipenem. The overall cure rate in this small study was 85 % for the 100-mg dose of tigecycline, 75 % for imipenem and 70 % for the 75-mg dose of tigecycline [108]. Thus prior studies with standard-dose tigecycline in pneumonia may not have used the ideal dosing for this drug.
Observational clinical studies that compare the efficacy of tigecycline with comparators for XDR A. baumannii infections are scarce. The largest case series on the use of tigecycline for XDR A. baumannii infections comes from Taiwan, where 266 patients were treated with tigecycline alone or in combination with another agent (a carbapenem, expanded-spectrum cephalosporin or piperacillin–tazobactam), and 120 were treated with imipenem and sulbactam [109]. In both arms, the isolates were resistant to all antibiotics tested except tigecycline and colistin. The patients who received tigecycline were significantly less likely to be in an ICU, were less likely to be febrile, had lower serum creatinine, and were less likely to have sepsis, all pointing to the lower severity of illness as well as infection in the tigecycline group. Also, the tigecycline group was more likely to have pneumonia (64.7 vs. 31.7 %) and less likely to have bacteremia (18.0 vs. 43.3 %) compared with the non-tigecycline group. With these caveats in mind, there was no difference in 30-day mortality between the two groups, and there was a lower percentage of patients with unfavorable clinical outcome in the tigecycline group (30.8 vs. 50.0 %; p < 0.001). Since the isolates were resistant to the agents used in the non-tigecycline group, the results suggest that there may be some efficacy of tigecycline in the treatment of XDR A. baumannii infections.
Tigecycline, despite all its limitations, may be effective when given early. Four of five patients (80.0 %) treated with tigecycline for imipenem-resistant A. baumannii bloodstream infection survived when therapy was started within 2 days, as opposed to only one of nine patients (11.1 %) when therapy was started late [19]. In this study, the combination of tigecycline and colistin had a similar trend, where four of five patients (80.0 %) survived when treated early but none of five patients survived when treated late.
There remains significant concern about emergence of resistance on tigecycline monotherapy. Two clear instances of this have been reported in the literature, both with monotherapy. One was a ventilator-associated pneumonia treated with tigecycline monotherapy for an initially susceptible isolate, with subsequent resistant isolate in the lungs (greater than threefold increase in MIC) [110]. The other was a patient with a susceptible urinary isolate treated with tigecycline monotherapy, who had subsequent infection (pneumonia and epidural abscess) with a tigecycline-resistant isolate [111]. Given the pharmacokinetics of tigecycline in relation to both urinary excretion and pulmonary concentrations, it is conceivable that subtherapeutic site concentrations contributed to resistance in these cases. Given these concerns, the role of tigecycline in pathogen-specific therapy of A. baumannii infections may be limited, at least in the context of monotherapy and at the currently approved dose.
5.4 Minocycline
Minocycline is a derivative of tetracycline. Like tigecycline, its mode of action is inhibition of the 30S ribosomal subunits. It maintains better activity against A. baumannii compared with tetracycline or doxycycline since it is generally less prone to efflux-mediated resistance, though it does not overcome resistance due to ribosomal protection, whereas tigecycline does [112]. It is almost completely absorbed when taken orally, and achieves a peak serum concentration of approximately 3 mg/L after a 200-mg dose, with a prolonged serum half-life of 12–18 h [113].
Minocycline maintains good in vitro activity against contemporary isolates of A. baumannii. In a surveillance study of MDR A. baumannii isolates collected in the USA between 2005 and 2011, 72.1 % were susceptible to minocycline, whereas only 8.7 % were susceptible to carbapenems [100]. In addition, a high rate of in vitro synergy has been observed between minocycline and colistin, meropenem or sulbactam for carbapenem-resistant A. baumannii [114, 115]. However, reports of clinical experience remain extremely limited. In a series of eight patients treated with oral minocycline for traumatic wound infections due to MDR A. baumannii (six of which were resistant to carbapenems), minocycline therapy resulted in clinical cure in seven of the patients [116]. These patients were young, otherwise healthy military service personnel. In another small series, four patients with ventilator-associated pneumonia due to XDR A. baumannii were treated with intravenous minocycline [117]. One also received imipenem, though the isolate was resistant to this agent. All four patients had clinical improvement, and three of them had microbiologic clearance as well. A retrospective single-center study on carbapenem-resistant A. baumannii ventilator-associated pneumonia found a good rate of clinical response in 36 patients treated with doxycycline or minocycline in monotherapy or combination therapy (81.8 and 80 %, respectively) [118]. Of note, 76 % of the isolates were susceptible to aminoglycosides, and these were the most common drugs used in combination.
Despite the well-maintained in vitro activity, the bacteriostatic action of minocycline and the availability of tigecycline, to which a higher proportion of carbapenem-resistant and XDR A. baumannii are susceptible, limit the clinical use of minocycline for A. baumannii infections. However, it may have roles in the context of combination therapy or as step-down therapy given the availability of both intravenous and oral formulations. Clearly, more clinical data are needed on the use of this agent to make a better assessment of its role in the therapy of A. baumannii infections.
5.5 Rifampin
Rifampin often retains low MICs for XDR A. baumannii. While rifampin cannot be used for treatment alone because of rapid emergence of resistance, its potential role in combinations with other agents, in particular, colistin, has been explored (for further discussion of combination therapy, see Sect. 5.8). In vitro synergy between colistin and rifampin has been demonstrated for MDR and carbapenem-resistant A. baumannii at their MICs [119, 120]. Efficacy of rifampin alone or in combination with colistin, imipenem or sulbactam was also shown in pneumonia and meningitis models [121], and rifampin alone or with colistin prolonged survival of neutropenic rats in a thigh infection model [122], both models using carbapenem-resistant A. baumannii. Clinical case series have also shown low infection-related mortality (21 %) among patients with XDR A. baumannii nosocomial pneumonia or bloodstream infection treated with this combination [123].
Two prospective clinical trials have been conducted on this topic. In an open-label, randomized trial comparing the efficacy of colistin alone and colistin plus rifampin conducted in Turkey, 43 patients with ventilator-associated pneumonia due to carbapenem-resistant A. baumannii were enrolled [124]. Twenty-two patients were treated with colistin alone, and 21 were treated with the combination. The dose of colistin was 300 mg CBA/day. The two groups were comparable with the exception of the mean Sequential Organ Failure Assessment (SOFA) score, which was higher for the combination group. The crude in-hospital mortality was nominally higher for the colistin group (72.7 %) compared with the combination group (61.9 %), and so was the pneumonia-related mortality (63.6 vs. 38.1 %). Synergy was observed between colistin and rifampin for all isolates in vitro. Twenty-three percent developed nephrotoxicity, but none had hepatotoxicity from rifampin. Overall this study was underpowered to detect relevant differences in mortality and other key outcomes.
The other, larger study was conducted in Italy [125]. This was a multicenter, open-label, randomized trial comparing the efficacy of colistin alone and colistin plus rifampin. Patients with life-threatening infection due to XDR A. baumannii which remained susceptible to colistin were enrolled. The study was powered to detect a 20 % absolute difference in 30-day mortality between the two groups. A total of 210 patients were enrolled, and 209 received at least one dose of the study drug(s). The baseline characteristics were comparable, with most patients located in ICUs. There was no mortality difference between the two groups (43.4 % for the combination group, 42.9 % for the colistin group). This was the case even when patients who had rifampin-resistant isolates were excluded. However, the microbiologic eradication rate was significantly higher in the combination group (60.6 vs. 44.8 %; p = 0.034). In terms of adverse events, renal impairment occurred evenly (26.2 % overall), but hepatic dysfunction was nominally more common in the combination group, presumably due to rifampin use (20.8 vs. 11.9 %; p = 0.13). Several aspects of this study are worth a mention. The dose of colistin was approximately 180 mg CBA/day, which is lower than the dosing recommended currently based on contemporary pharmacokinetic assessments [76], though this would have affected both groups equally if anything. In addition, meropenem was added in the colistin group more frequently than in the combination group (15.9 vs. 3.9 %), which may have improved the outcome in the colistin group compared with what might have been achieved with colistin alone.
Taken together, the beneficial effect of adding rifampin in the treatment of XDR A. baumannii infection, which had been suggested repeatedly by in vitro and animal studies, has not been demonstrated in two randomized, controlled trials. Also, given the potential for hepatotoxicity and significant drug interactions due to the induction of cytochrome P450 3A4, the use of rifampin is currently not recommend in the treatment of A. baumannii infection.
5.6 Fosfomycin
Fosfomycin is an inhibitor of peptidoclycan biosynthesis which has a broad spectrum of activity across Gram-positive and Gram-negative pathogens, but not A. baumannii [126]. However, in vitro synergy has been reported between fosfomycin and colistin or sulbactam among carbapenem-resistant A. baumannii [127].
The results of a randomized controlled trial of colistin versus colistin plus fosfomycin for infections caused by carbapenem-resistant A. baumannii were presented recently from Thailand [128]. In this study, 99 patients were enrolled and 94 were included in the analysis, 47 in each group. Fosfomycin was given at 4 g every 12 h intravenously to patients in the combination arm, and colistin was given at 5 mg CBA/kg/day to both groups for 7–14 days. The two groups did not differ in favorable clinical outcomes (59.6 vs. 55.3 %; p = 0.835) nor mortality at 28 days (46.8 vs. 57.4 %; p = 0.409). However, microbiologic eradication rates at the end of treatment were significantly higher in the combination group (100 vs. 81.2 %; p = 0.01). Of concern, the dose of fosfomycin was lower than has been used in other infections. In addition, this study was grossly underpowered to detect a relevant difference in mortality, but, like with rifampin, microbiologic clearance was significantly improved when combination therapy was used. Therefore, the combination of colistin and fosfomycin appears to merit further investigation.
5.7 Glycopeptides
Glycopeptides, including vancomycin, teicoplanin and telavancin, exert their activity by inhibiting peptidoglycan synthesis, but they do not penetrate the Gram-negative bacterial outer membrane and are considered inactive against Gram-negative pathogens. However, disruption of the outer membrane may allow them to reach their targets in Gram-negative bacteria. This phenomenon was initially suggested in colistin-resistant A. baumannii [129]. Subsequently, a series of investigations, both in vitro and using waxworm infection models, have reported potent synergy between glycopeptides and colistin [130–132]. A recent study evaluating A. baumannii clinical isolates from a Greek hospital found that seven of the ten colistin-susceptible isolates had synergy with daptomycin via time-kill methodology. This suggests that daptomycin, similarly to vancomycin, may be useful when combined with colistin [133].
An observational study conducted in Spain compared the outcome of patients who had carbapenem-resistant A. baumannii ventilator-associated pneumonia or bacteremia, 29 of them treated with colistin and vancomycin and 28 of them treated with colistin without vancomycin [134]. The clinical cure rate was similar in both treatment groups (55.2 vs. 67.9 %; p = 0.32), and microbiologic eradication was documented in 65.2 % of patients treated with colistin and in 54.2 % of patients treated with combined therapy (p = 0.44). However, the rate of renal failure was significantly higher in the combination therapy group (55.2 vs. 28.6 %; p = 0.04).
A similar study from Italy, where 166 patients who were given colistin for any Gram-negative infections were surveyed, showed somewhat opposing results [135]. Approximately 60 % of the infections were due to carbapenem-resistant A. baumannii. Sixty-eight received a colistin–glycopeptide combination, and 98 received colistin without a glycopeptide. The combination group had more bloodstream infections and less ventilator-associated pneumonia. The 30-day mortality for patients with carbapenem-resistant A. baumannii infection was comparable (41.7 vs. 35.3 %; p = 0.54) and so was the rate of nephrotoxicity (10.4 vs. 15.7 %; p = 0.55). Of note, colistin–glycopeptide combination therapy given for 5 days or longer was an independent protective factor for survival (hazard ratio 0.41; p = 0.04).
Given these inconclusive data, more clinical studies are needed on this topic, ideally as a prospective controlled study, especially given the difficulty in controlling for the differences in Gram-positive co-infections.
5.8 Role of Combination Therapy
While colistin is a key drug in the therapy of XDR A. baumannii infections, there are concerns regarding its unpredictable and suboptimal pharmacokinetics [76, 77] and documentation of emergence of colistin resistance during therapy [136, 137]. Similar concerns about suboptimal pharmacokinetics and resistance emerging on therapy exist for tigecycline [108, 110, 111]. Regarding sulbactam, optimal dosing is unclear and there is concern about in vitro efficacy not necessarily predicting clinical outcomes [98]. Given these concerns, various combination regimens have been studied mostly with colistin serving as one of the agents. The studies which have focused on comparing combination and monotherapy are listed in Table 2.
In a large retrospective study from 27 Turkish hospitals, the clinical outcome of patients with XDR A. baumannii bloodstream infections was investigated [23]. Thirty-six of them received colistin monotherapy, whereas 214 received colistin-based combination therapy (102 with a carbapenem, 69 with ampicillin–sulbactam or sulbactam, and 43 with other agents). The baseline characteristics were comparable among the groups, and all isolates were susceptible to colistin and not more than one additional class, but no specific microbiologic breakdown was reported. None received a loading dose of colistin, and the standard dose of colistin was 5 mg CBA/kg/day. The in-hospital mortality rate was significantly lower in the combination group compared with the monotherapy group (52.3 vs. 72.2 %; p = 0.03), and the rate of microbiologic eradication was also significantly higher in the combination group than the monotherapy group (79.9 vs. 55.6 %; p = 0.001). When the combination group was broken down by the agent that accompanied colistin, no difference in mortality was observed.
In another observational study, including 69 patients with solid organ transplantation who developed XDR A. baumannii infection, where most developed ventilator-associated pneumonia, treatment with a combination of colistin and a carbapenem was an independent predictor of survival, whereas none of four patients who received any monotherapy survived; however, none in the monotherapy group received colistin [138]. In yet another single-center study, in which all patients on colistin were evaluated for clinical cure versus deterioration, 87 % of patients on colistin monotherapy and 84 % of those on colistin and meropenem combination had a clinical cure, whereas the rate of cure with colistin and piperacillin–tazobactam combination was 68 % and the rate of cure with colistin and sulbactam was 73 % for A. baumannii infection. Of note, in this study, lower dose colistin was associated with poor outcomes compared with higher doses [139]. The inadequacy of monotherapy for resistant A. baumannii infections may be due to a lack of highly effective drugs and/or the lack of adequate site concentrations of drugs. The possibility of synergy with, for example, glycopeptides, may mitigate the first consideration. In addition, combination therapy for drugs with pharmacokinetic challenges may help mitigate the concern for resistance on therapy with colistin and tigecycline. These concerns, together with the unique pharmacokinetic properties of colistin (which is administered as a prodrug), support the use of combination regimens for the treatment of invasive XDR A. baumannii infections.
Many questions remain unanswered, however. Is combination therapy still beneficial when dosing of colistin is optimized? Are patients at a higher risk for adverse events, especially nephrotoxicity, when multiple agents are used together? How can we best prevent the emergence of colistin resistance? The results from the ongoing randomized trials comparing colistin monotherapy and colistin–carbapenem combination therapy for the treatment of XDR Gram-negative pathogens, including XDR A. baumannii, should help address these questions.
5.9 Importance of Early Appropriate Therapy
Early appropriate antimicrobial therapy [i.e., therapy including agent(s) that have in vitro activity] is crucial in reducing mortality due to severe sepsis and septic shock, in particular, for cases caused by resistant Gram-negative pathogens, including A. baumannii [140, 141]. Furthermore, the risk of inappropriate early antimicrobial therapy increases substantially when the infecting strain is carbapenem resistant [24]. Evidence is accumulating that this is also the case for A. baumannii, in that higher mortality for XDR and carbapenem-resistant infections is strongly correlated with delay in the institution of appropriate therapy.
For imipenem-resistant A. baumannii bloodstream infection studied in Taiwan, patients given early appropriate therapy with colistin alone, tigecycline alone, or a combination of colistin and tigecycline had lower mortality (37.5, 20, 20 %) than those not given early appropriate therapy with the same agents (88.2, 88.9, 100 %) (p = 0.017, 0.023, 0.048) [12]. Another study from Taiwan investigated the appropriateness of therapy and clinical outcome among 252 cases of A. baumannii bloodstream infection [142]. Here, administration of appropriate therapy within 48 h of the onset of bloodstream infection was an independent predictor of survival at 14 days (odds ratio 0.22; p < 0.001). When adjusted for the severity of illness, early appropriate therapy predicted survival among patients with an Acute Physiology and Chronic Health Evaluation (APACHE) II score of 25 or greater. The protective effect of early appropriate therapy has also been demonstrated in a study of A. baumannii bloodstream infections conducted in Turkey (30-day mortality of 39.5 % for appropriate therapy vs. 65.0 % for inappropriate therapy; p = 0.011) [143] and a Brazilian study describing A. baumannii infections among solid organ transplant recipients, where early appropriate therapy was associated with significantly lower A. baumannii-related mortality (odds ratio = 0.04; p = 0.03) [144].
Early administration of an agent which has activity against the offending strain of A. baumannii is therefore critical in improving survival of patients, especially for those who are critically ill. Rapid identification of A. baumannii, and possibly XDR or carbapenem resistance, would be crucial in shortening the time until appropriate therapy is instituted, at least presumptively. At this point, it is not clear whether adequate therapy means one or multiple agents with activity. If, as some data suggest, combination therapy for A. baumannii is superior to monotherapy, it may be that multiple active agents, at optimal dosing, early in the course of infection, will be the most effective way to treat these infections. Advances in diagnostics, such as direct species identification from clinical samples using matrix-assisted laser desorption ionization–time of flight (MALDI–TOF), can be leveraged to achieve this goal.
6 Concluding Remarks
A. baumannii is a significant healthcare-associated pathogen, causing invasive infections in patients with co-morbid conditions and pre-existing illnesses. The current data suggest that carbapenem-resistant strains are likely to respond better to colistin-based combination therapy compared with monotherapy. At this point, it remains unclear what the optimal companion agent is in the setting of carbapenem resistance. There are at least two advantages of combination therapy. The first involves decreasing time to effective therapy, especially given the time it takes for colistin to achieve therapeutic levels in the blood. The second relates to targeting multiple cellular mechanisms to enhance the overall antibacterial activity when the activities of single agents are no longer considered reliable.
Given the increase in carbapenem resistance in the last decade, this once-reliable drug class now offers only slightly better than 50 % coverage of this pathogen. A priori prediction of resistance is difficult as A. baumannii has multiple related mechanisms of resistance. If carbapenem resistance continues to increase in A. baumannii, empiric coverage for carbapenem-resistant and XDR strains will likely require colistin-based combination therapy even prior to determination of antimicrobial susceptibilities in critically ill patients. This would represent a major shift from current practice where the use of colistin is usually considered only in the context of definitive, salvage therapy, rather than empiric therapy. The ongoing clinical trials may indicate which specific colistin-containing regimens are most effective while minimizing toxicity in this population and give some guidance in these situations.
References
Peleg AY, Seifert H, Paterson DL. Acinetobacter baumannii: emergence of a successful pathogen. Clin Microbiol Rev. 2008;21(3):538–82.
Sievert DM, Ricks P, Edwards JR, Schneider A, Patel J, Srinivasan A, et al. Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2009–2010. Infect Control Hosp Epidemiol. 2013;34(1):1–14.
Chuang YC, Sheng WH, Li SY, Lin YC, Wang JT, Chen YC, et al. Influence of genospecies of Acinetobacter baumannii complex on clinical outcomes of patients with Acinetobacter bacteremia. Clin Infect Dis. 2011;52(3):352–60.
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–81.
Queenan AM, Pillar CM, Deane J, Sahm DF, Lynch AS, Flamm RK, et al. Multidrug resistance among Acinetobacter spp. in the USA and activity profile of key agents: results from CAPITAL Surveillance 2010. Diagn Microbiol Infect Dis. 2012;73(3):267–70.
Pogue JM, Mann T, Barber KE, Kaye KS. Carbapenem-resistant Acinetobacter baumannii: epidemiology, surveillance and management. Expert Rev Anti Infect Ther. 2013;11(4):383–93.
Hidron AI, Edwards JR, Patel J, Horan TC, Sievert DM, Pollock DA, et al. NHSN annual update: antimicrobial-resistant pathogens associated with healthcare-associated infections: annual summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2006–2007. Infect Control Hosp Epidemiol. 2008;29(11):996–1011.
Kallen AJ, Hidron AI, Patel J, Srinivasan A. Multidrug resistance among gram-negative pathogens that caused healthcare-associated infections reported to the National Healthcare Safety Network, 2006-2008. Infect Control Hosp Epidemiol. 2010;31(5):528–31.
Mera RM, Miller LA, Amrine-Madsen H, Sahm DF. Acinetobacter baumannii 2002–2008: increase of carbapenem-associated multiclass resistance in the United States. Microb Drug Resist. 2010;16(3):209–15.
Schleicher X, Higgins PG, Wisplinghoff H, Korber-Irrgang B, Kresken M, Seifert H. Molecular epidemiology of Acinetobacter baumannii and Acinetobacter nosocomialis in Germany over a 5-year period (2005–2009). Clin Microbiol Infect. 2013;19(8):737–42.
Chuang YC, Sheng WH, Lauderdale TL, Li SY, Wang JT, Chen YC, et al. Molecular epidemiology, antimicrobial susceptibility and carbapenemase resistance determinants among Acinetobacter baumannii clinical isolates in Taiwan. J Microbiol Immunol Infect. 2013; in press.
Wisplinghoff H, Paulus T, Lugenheim M, Stefanik D, Higgins PG, Edmond MB, et al. Nosocomial bloodstream infections due to Acinetobacter baumannii, Acinetobacter pittii and Acinetobacter nosocomialis in the United States. J Infect. 2012;64(3):282–90.
Adams-Haduch JM, Onuoha EO, Bogdanovich T, Tian GB, Marschall J, Urban CM, et al. Molecular epidemiology of carbapenem-nonsusceptible Acinetobacter baumannii in the United States. J Clin Microbiol. 2011;49(11):3849–54.
Ng TM, Teng CB, Lye DC, Apisarnthanarak A. A multicenter case–case control study for risk factors and outcomes of extensively drug-resistant Acinetobacter baumannii bacteremia. Infect Control Hosp Epidemiol. 2014;35(1):49–55.
Sheng WH, Liao CH, Lauderdale TL, Ko WC, Chen YS, Liu JW, et al. A multicenter study of risk factors and outcome of hospitalized patients with infections due to carbapenem-resistant Acinetobacter baumannii. Int J Infect Dis. 2010;14(9):e764–9.
Cisneros JM, Rodriguez-Bano J, Fernandez-Cuenca F, Ribera A, Vila J, Pascual A, et al. Risk-factors for the acquisition of imipenem-resistant Acinetobacter baumannii in Spain: a nationwide study. Clin Microbiol Infect. 2005;11(11):874–9.
Lee SO, Kim NJ, Choi SH, Hyong Kim T, Chung JW, Woo JH, et al. Risk factors for acquisition of imipenem-resistant Acinetobacter baumannii: a case–control study. Antimicrob Agents Chemother. 2004;48(1):224–8.
Lemos EV, de la Hoz FP, Einarson TR, McGhan WF, Quevedo E, Castaneda C, et al. Carbapenem resistance and mortality in patients with Acinetobacter baumannii infection: systematic review and meta-analysis. Clin Microbiol Infect. 2014;20(5):416–23.
Lee HY, Chen CL, Wu SR, Huang CW, Chiu CH. Risk factors and outcome analysis of Acinetobacter baumannii complex bacteremia in critical patients. Crit Care Med. 2014;42(5):1081–8.
Kim SY, Jung JY, Kang YA, Lim JE, Kim EY, Lee SK, et al. Risk factors for occurrence and 30-day mortality for carbapenem-resistant Acinetobacter baumannii bacteremia in an intensive care unit. J Korean Med Sci. 2012;27(8):939–47.
Kang G, Hartzell JD, Howard R, Wood-Morris RN, Johnson MD, Fraser S, et al. Mortality associated with Acinetobacter baumannii complex bacteremia among patients with war-related trauma. Infect Control Hosp Epidemiol. 2010;31(1):92–4.
Kim YJ, Kim SI, Hong KW, Kim YR, Park YJ, Kang MW. Risk factors for mortality in patients with carbapenem-resistant Acinetobacter baumannii bacteremia: impact of appropriate antimicrobial therapy. J Korean Med Sci. 2012;27(5):471–5.
Batirel A, Balkan, II, Karabay O, Agalar C, Akalin S, Alici O, et al. Comparison of colistin–carbapenem, colistin–sulbactam, and colistin plus other antibacterial agents for the treatment of extremely drug-resistant Acinetobacter baumannii bloodstream infections. Eur J Clin Microbiol Infect Dis. 2014;33(8):1311–22.
Esterly JS, Griffith M, Qi C, Malczynski M, Postelnick MJ, Scheetz MH. Impact of carbapenem resistance and receipt of active antimicrobial therapy on clinical outcomes of Acinetobacter baumannii bloodstream infections. Antimicrob Agents Chemother. 2011;55(10):4844–9.
Munoz-Price LS, Zembower T, Penugonda S, Schreckenberger P, Lavin MA, Welbel S, et al. Clinical outcomes of carbapenem-resistant Acinetobacter baumannii bloodstream infections: study of a 2-state monoclonal outbreak. Infect Control Hosp Epidemiol. 2010;31(10):1057–62.
Chopra T, Marchaim D, Awali RA, Krishna A, Johnson P, Tansek R, et al. Epidemiology of bloodstream infections caused by Acinetobacter baumannii and impact of drug resistance to both carbapenems and ampicillin–sulbactam on clinical outcomes. Antimicrob Agents Chemother. 2013;57(12):6270–5.
Woodford N, Turton JF, Livermore DM. Multiresistant Gram-negative bacteria: the role of high-risk clones in the dissemination of antibiotic resistance. FEMS Microbiol Rev. 2011;35(5):736–55.
Hujer KM, Hamza NS, Hujer AM, Perez F, Helfand MS, Bethel CR, et al. Identification of a new allelic variant of the Acinetobacter baumannii cephalosporinase, ADC-7 β-lactamase: defining a unique family of class C enzymes. Antimicrob Agents Chemother. 2005;49(7):2941–8.
Bou G, Martinez-Beltran J. Cloning, nucleotide sequencing, and analysis of the gene encoding an AmpC β-lactamase in Acinetobacter baumannii. Antimicrob Agents Chemother. 2000;44(2):428–32.
Heritier C, Poirel L, Nordmann P. Cephalosporinase over-expression resulting from insertion of ISAba1 in Acinetobacter baumannii. Clin Microbiol Infect. 2006;12(2):123–30.
Lopes BS, Amyes SG. Role of ISAba1 and ISAba125 in governing the expression of bla ADC in clinically relevant Acinetobacter baumannii strains resistant to cephalosporins. J Med Microbiol. 2012;61(Pt 8):1103–8.
Tian GB, Adams-Haduch JM, Taracila M, Bonomo RA, Wang HN, Doi Y. Extended-spectrum AmpC cephalosporinase in Acinetobacter baumannii: ADC-56 confers resistance to cefepime. Antimicrob Agents Chemother. 2011;55(10):4922–5.
Vahaboglu H, Ozturk R, Aygun G, Coskunkan F, Yaman A, Kaygusuz A, et al. Widespread detection of PER-1-type extended-spectrum β-lactamases among nosocomial Acinetobacter and Pseudomonas aeruginosa isolates in Turkey: a nationwide multicenter study. Antimicrob Agents Chemother. 1997;41(10):2265–9.
Lee Y, Bae IK, Kim J, Jeong SH, Lee K. Dissemination of ceftazidime-resistant Acinetobacter baumannii clonal complex 92 in Korea. J Appl Microbiol. 2012;112(6):1207–11.
Naas T, Coignard B, Carbonne A, Blanckaert K, Bajolet O, Bernet C, et al. VEB-1 extended-spectrum β-lactamase-producing Acinetobacter baumannii, France. Emerg Infect Dis. 2006;12(8):1214–22.
Adams-Haduch JM, Paterson DL, Sidjabat HE, Pasculle AW, Potoski BA, Muto CA, et al. Genetic basis of multidrug resistance in Acinetobacter baumannii clinical isolates at a tertiary medical center in Pennsylvania. Antimicrob Agents Chemother. 2008;52(11):3837–43.
Rumbo C, Gato E, Lopez M, Ruiz de Alegria C, Fernandez-Cuenca F, Martinez-Martinez L, et al. Contribution of efflux pumps, porins, and β-lactamases to multidrug resistance in clinical isolates of Acinetobacter baumannii. Antimicrob Agents Chemother. 2013;57(11):5247–57.
Heritier C, Poirel L, Lambert T, Nordmann P. Contribution of acquired carbapenem-hydrolyzing oxacillinases to carbapenem resistance in Acinetobacter baumannii. Antimicrob Agents Chemother. 2005;49(8):3198–202.
Turton JF, Ward ME, Woodford N, Kaufmann ME, Pike R, Livermore DM, et al. The role of ISAba1 in expression of OXA carbapenemase genes in Acinetobacter baumannii. FEMS Microbiol Lett. 2006;258(1):72–7.
Figueiredo S, Poirel L, Papa A, Koulourida V, Nordmann P. Overexpression of the naturally occurring bla OXA-51 gene in Acinetobacter baumannii mediated by novel insertion sequence ISAba9. Antimicrob Agents Chemother. 2009;53(9):4045–7.
Higgins PG, Perez-Llarena FJ, Zander E, Fernandez A, Bou G, Seifert H. OXA-235, a novel class D β-lactamase involved in resistance to carbapenems in Acinetobacter baumannii. Antimicrob Agents Chemother. 2013;57(5):2121–6.
Mugnier PD, Poirel L, Naas T, Nordmann P. Worldwide dissemination of the bla OXA-23 carbapenemase gene of Acinetobacter baumannii. Emerg Infect Dis. 2010;16(1):35–40.
Chen Y, Zhou Z, Jiang Y, Yu Y. Emergence of NDM-1-producing Acinetobacter baumannii in China. J Antimicrob Chemother. 2011;66(6):1255–9.
Decousser JW, Jansen C, Nordmann P, Emirian A, Bonnin RA, Anais L, et al. Outbreak of NDM-1-producing Acinetobacter baumannii in France, January to May 2013. Euro Surveill. 2013;18(31):1–4.
Tsakris A, Ikonomidis A, Pournaras S, Tzouvelekis LS, Sofianou D, Legakis NJ, et al. VIM-1 metallo-β-lactamase in Acinetobacter baumannii. Emerg Infect Dis. 2006;12(6):981–3.
Kouyama Y, Harada S, Ishii Y, Saga T, Yoshizumi A, Tateda K, et al. Molecular characterization of carbapenem-non-susceptible Acinetobacter spp. in Japan: predominance of multidrug-resistant Acinetobacter baumannii clonal complex 92 and IMP-type metallo-β-lactamase-producing non-baumannii Acinetobacter species. J Infect Chemother. 2012;18(4):522–8.
Lee K, Yum JH, Yong D, Lee HM, Kim HD, Docquier JD, et al. Novel acquired metallo-β-lactamase gene, bla SIM-1, in a class 1 integron from Acinetobacter baumannii clinical isolates from Korea. Antimicrob Agents Chemother. 2005;49(11):4485–91.
Robledo IE, Aquino EE, Sante MI, Santana JL, Otero DM, Leon CF, et al. Detection of KPC in Acinetobacter spp. in Puerto Rico. Antimicrob Agents Chemother. 2010;54(3):1354–7.
Moubareck C, Bremont S, Conroy MC, Courvalin P, Lambert T. GES-11, a novel integron-associated GES variant in Acinetobacter baumannii. Antimicrob Agents Chemother. 2009;53(8):3579–81.
Urban C, Go E, Mariano N, Rahal JJ. Interaction of sulbactam, clavulanic acid and tazobactam with penicillin-binding proteins of imipenem-resistant and -susceptible Acinetobacter baumannii. FEMS Microbiol Lett. 1995;125:193–7.
Fernandez-Cuenca F, Martinez-Martinez L, Conejo MC, Ayala JA, Perea EJ, Pascual A. Relationship between β-lactamase production, outer membrane protein and penicillin-binding protein profiles on the activity of carbapenems against clinical isolates of Acinetobacter baumannii. J Antimicrob Chemother. 2003;51(3):565–74.
Krizova L, Poirel L, Nordmann P, Nemec A. TEM-1 β-lactamase as a source of resistance to sulbactam in clinical strains of Acinetobacter baumannii. J Antimicrob Chemother. 2013;68(12):2786–91.
Giannouli M, Di Popolo A, Durante-Mangoni E, Bernardo M, Cuccurullo S, Amato G, et al. Molecular epidemiology and mechanisms of rifampicin resistance in Acinetobacter baumannii isolates from Italy. Int J Antimicrob Agents. 2012;39(1):58–63.
Houang ET, Chu YW, Lo WS, Chu KY, Cheng AF. Epidemiology of rifampin ADP-ribosyltransferase (arr-2) and metallo-β-lactamase (bla IMP-4) gene cassettes in class 1 integrons in Acinetobacter strains isolated from blood cultures in 1997 to 2000. Antimicrob Agents Chemother. 2003;47(4):1382–90.
Shaw KJ, Rather PN, Hare RS, Miller GH. Molecular genetics of aminoglycoside resistance genes and familial relationships of the aminoglycoside-modifying enzymes. Microbiol Rev. 1993;57(1):138–63.
Landman D, Kelly P, Backer M, Babu E, Shah N, Bratu S, et al. Antimicrobial activity of a novel aminoglycoside, ACHN-490, against Acinetobacter baumannii and Pseudomonas aeruginosa from New York City. J Antimicrob Chemother. 2011;66(2):332–4.
Akers KS, Chaney C, Barsoumian A, Beckius M, Zera W, Yu X, et al. Aminoglycoside resistance and susceptibility testing errors in Acinetobacter baumannii–calcoaceticus complex. J Clin Microbiol. 2010;48(4):1132–8.
Liou GF, Yoshizawa S, Courvalin P, Galimand M. Aminoglycoside resistance by ArmA-mediated ribosomal 16S methylation in human bacterial pathogens. J Mol Biol. 2006;359(2):358–64.
Yu YS, Zhou H, Yang Q, Chen YG, Li LJ. Widespread occurrence of aminoglycoside resistance due to ArmA methylase in imipenem-resistant Acinetobacter baumannii isolates in China. J Antimicrob Chemother. 2007;60(2):454–5.
Doi Y, Adams JM, Yamane K, Paterson DL. Identification of 16S rRNA methylase-producing Acinetobacter baumannii clinical strains in North America. Antimicrob Agents Chemother. 2007;51(11):4209–10.
Coyne S, Rosenfeld N, Lambert T, Courvalin P, Perichon B. Overexpression of resistance-nodulation-cell division pump AdeFGH confers multidrug resistance in Acinetobacter baumannii. Antimicrob Agents Chemother. 2010;54(10):4389–93.
Beceiro A, Llobet E, Aranda J, Bengoechea JA, Doumith M, Hornsey M, et al. Phosphoethanolamine modification of lipid A in colistin-resistant variants of Acinetobacter baumannii mediated by the pmrAB two-component regulatory system. Antimicrob Agents Chemother. 2011;55(7):3370–9.
Pelletier MR, Casella LG, Jones JW, Adams MD, Zurawski DV, Hazlett KR, et al. Unique structural modifications are present in the lipopolysaccharide from colistin-resistant strains of Acinetobacter baumannii. Antimicrob Agents Chemother. 2013;57(10):4831–40.
Arroyo LA, Herrera CM, Fernandez L, Hankins JV, Trent MS, Hancock RE. The pmrCAB operon mediates polymyxin resistance in Acinetobacter baumannii ATCC 17978 and clinical isolates through phosphoethanolamine modification of lipid A. Antimicrob Agents Chemother. 2011;55(8):3743–51.
Moffatt JH, Harper M, Harrison P, Hale JD, Vinogradov E, Seemann T, et al. Colistin resistance in Acinetobacter baumannii is mediated by complete loss of lipopolysaccharide production. Antimicrob Agents Chemother. 2010;54(12):4971–7.
Chopra I, Hawkey PM, Hinton M. Tetracyclines, molecular and clinical aspects. J Antimicrob Chemother. 1992;29(3):245–77.
Coyne S, Courvalin P, Perichon B. Efflux-mediated antibiotic resistance in Acinetobacter spp. Antimicrob Agents Chemother. 2011;55(3):947–53.
Abbott I, Cerqueira GM, Bhuiyan S, Peleg AY. Carbapenem resistance in Acinetobacter baumannii: laboratory challenges, mechanistic insights and therapeutic strategies. Expert Rev Anti Infect Ther. 2013;11(4):395–409.
Cai Y, Chai D, Wang R, Liang B, Bai N. Colistin resistance of Acinetobacter baumannii: clinical reports, mechanisms and antimicrobial strategies. J Antimicrob Chemother. 2012;67(7):1607–15.
Akajagbor DS, Wilson SL, Shere-Wolfe KD, Dakum P, Charurat ME, Gilliam BL. Higher incidence of acute kidney injury with intravenous colistimethate sodium compared with polymyxin B in critically ill patients at a tertiary care medical center. Clin Infect Dis. 2013;57(9):1300–3.
Nation RL, Li J, Cars O, Couet W, Dudley MN, Kaye KS, et al. Consistent global approach on reporting of colistin doses to promote safe and effective use. Clin Infect Dis. 2014;58(1):139–41.
Bergen PJ, Landersdorfer CB, Zhang J, Zhao M, Lee HJ, Nation RL, et al. Pharmacokinetics and pharmacodynamics of ‘old’ polymyxins: what is new? Diagn Microbiol Infect Dis. 2012;74(3):213–23.
Owen RJ, Li J, Nation RL, Spelman D. In vitro pharmacodynamics of colistin against Acinetobacter baumannii clinical isolates. J Antimicrob Chemother. 2007;59(3):473–7.
Li J, Rayner CR, Nation RL, Owen RJ, Spelman D, Tan KE, et al. Heteroresistance to colistin in multidrug-resistant Acinetobacter baumannii. Antimicrob Agents Chemother. 2006;50(9):2946–50.
Mohamed AF, Karaiskos I, Plachouras D, Karvanen M, Pontikis K, Jansson B, et al. Application of a loading dose of colistin methanesulfonate in critically ill patients: population pharmacokinetics, protein binding, and prediction of bacterial kill. Antimicrob Agents Chemother. 2012;56(8):4241–9.
Garonzik SM, Li J, Thamlikitkul V, Paterson DL, Shoham S, Jacob J, et al. Population pharmacokinetics of colistin methanesulfonate and formed colistin in critically ill patients from a multicenter study provide dosing suggestions for various categories of patients. Antimicrob Agents Chemother. 2011;55(7):3284–94.
Plachouras D, Karvanen M, Friberg LE, Papadomichelakis E, Antoniadou A, Tsangaris I, et al. Population pharmacokinetic analysis of colistin methanesulfonate and colistin after intravenous administration in critically ill patients with infections caused by gram-negative bacteria. Antimicrob Agents Chemother. 2009;53(8):3430–6.
Garnacho-Montero J, Ortiz-Leyba C, Jimenez-Jimenez FJ, Barrero-Almodovar AE, Garcia-Garmendia JL, Bernabeu-Wittel IM, et al. Treatment of multidrug-resistant Acinetobacter baumannii ventilator-associated pneumonia (VAP) with intravenous colistin: a comparison with imipenem-susceptible VAP. Clin Infect Dis. 2003;36(9):1111–8.
Oliveira MS, Prado GV, Costa SF, Grinbaum RS, Levin AS. Ampicillin/sulbactam compared with polymyxins for the treatment of infections caused by carbapenem-resistant Acinetobacter spp. J Antimicrob Chemother. 2008;61(6):1369–75.
Betrosian AP, Frantzeskaki F, Xanthaki A, Douzinas EE. Efficacy and safety of high-dose ampicillin/sulbactam vs. colistin as monotherapy for the treatment of multidrug resistant Acinetobacter baumannii ventilator-associated pneumonia. J Infect. 2008;56(6):432–6.
Yapa SW, Li J, Patel K, Wilson JW, Dooley MJ, George J, et al. Pulmonary and systemic pharmacokinetics of inhaled and intravenous colistin methanesulfonate in cystic fibrosis patients: targeting advantage of inhalational administration. Antimicrob Agents Chemother. 2014;58(5):2570–9.
Conway SP. Nebulized antibiotic therapy: the evidence. Chron Respir Dis. 2005;2(1):35–41.
Tumbarello M, De Pascale G, Trecarichi EM, De Martino S, Bello G, Maviglia R, et al. Effect of aerosolized colistin as adjunctive treatment on the outcomes of microbiologically documented ventilator-associated pneumonia caused by colistin-only susceptible gram-negative bacteria. Chest. 2013;144(6):1768–75.
Kuo SC, Lee YT, Yang SP, Chen CP, Chen TL, Hsieh SL, et al. Eradication of multidrug-resistant Acinetobacter baumannii from the respiratory tract with inhaled colistin methanesulfonate: a matched case–control study. Clin Microbiol Infect. 2012;18(9):870–6.
Rattanaumpawan P, Lorsutthitham J, Ungprasert P, Angkasekwinai N, Thamlikitkul V. Randomized controlled trial of nebulized colistimethate sodium as adjunctive therapy of ventilator-associated pneumonia caused by Gram-negative bacteria. J Antimicrob Chemother. 2010;65(12):2645–9.
Markantonis SL, Markou N, Fousteri M, Sakellaridis N, Karatzas S, Alamanos I, et al. Penetration of colistin into cerebrospinal fluid. Antimicrob Agents Chemother. 2009;53(11):4907–10.
Imberti R, Cusato M, Accetta G, Marino V, Procaccio F, Del Gaudio A, et al. Pharmacokinetics of colistin in cerebrospinal fluid after intraventricular administration of colistin methanesulfonate. Antimicrob Agents Chemother. 2012;56(8):4416–21.
Karaiskos I, Galani L, Baziaka F, Giamarellou H. Intraventricular and intrathecal colistin as the last therapeutic resort for the treatment of multidrug-resistant and extensively drug-resistant Acinetobacter baumannii ventriculitis and meningitis: a literature review. Int J Antimicrob Agents. 2013;41(6):499–508.
Noguchi JK, Gill MA. Sulbactam: a β-lactamase inhibitor. Clin Pharm. 1988;7(1):37–51.
Rafailidis PI, Ioannidou EN, Falagas ME. Ampicillin/sulbactam: current status in severe bacterial infections. Drugs. 2007;67(13):1829–49.
Meyers BR, Wilkinson P, Mendelson MH, Walsh S, Bournazos C, Hirschman SZ. Pharmacokinetics of ampicillin–sulbactam in healthy elderly and young volunteers. Antimicrob Agents Chemother. 1991;35(10):2098–101.
Swenson JM, Killgore GE, Tenover FC. Antimicrobial susceptibility testing of Acinetobacter spp. by NCCLS broth microdilution and disk diffusion methods. J Clin Microbiol. 2004;42(11):5102–8.
Reddy T, Chopra T, Marchaim D, Pogue JM, Alangaden G, Salimnia H, et al. Trends in antimicrobial resistance of Acinetobacter baumannii isolates from a metropolitan Detroit health system. Antimicrob Agents Chemother. 2010;54(5):2235–8.
Montero A, Ariza J, Corbella X, Domenech A, Cabellos C, Ayats J, et al. Efficacy of colistin versus β-lactams, aminoglycosides, and rifampin as monotherapy in a mouse model of pneumonia caused by multiresistant Acinetobacter baumannii. Antimicrob Agents Chemother. 2002;46(6):1946–52.
Rodriguez-Hernandez MJ, Cuberos L, Pichardo C, Caballero FJ, Moreno I, Jimenez-Mejias ME, et al. Sulbactam efficacy in experimental models caused by susceptible and intermediate Acinetobacter baumannii strains. J Antimicrob Chemother. 2001;47(4):479–82.
Choi JY, Kim CO, Park YS, Yoon HJ, Shin SY, Kim YK, et al. Comparison of efficacy of cefoperazone/sulbactam and imipenem/cilastatin for treatment of Acinetobacter bacteremia. Yonsei Med J. 2006;47(1):63–9.
Wood GC, Hanes SD, Croce MA, Fabian TC, Boucher BA. Comparison of ampicillin-sulbactam and imipenem-cilastatin for the treatment of Acinetobacter ventilator-associated pneumonia. Clin Infect Dis. 2002;34(11):1425–30.
Oliveira MS, Costa SF, Pedri E, van der Heijden I, Levin AS. The minimal inhibitory concentration for sulbactam was not associated with the outcome of infections caused by carbapenem-resistant Acinetobacter sp. treated with ampicillin/sulbactam. Clinics (Sao Paulo). 2013;68(4):569–73.
Livermore DM. Tigecycline: what is it, and where should it be used? J Antimicrob Chemother. 2005;56(4):611–4.
Denys GA, Callister SM, Dowzicky MJ. Antimicrobial susceptibility among gram-negative isolates collected in the USA between 2005 and 2011 as part of the Tigecycline Evaluation and Surveillance Trial (T.E.S.T.). Ann Clin Microbiol Antimicrob. 2013;12:24.
Ruzin A, Keeney D, Bradford PA. AdeABC multidrug efflux pump is associated with decreased susceptibility to tigecycline in Acinetobacter calcoaceticus-Acinetobacter baumannii complex. J Antimicrob Chemother. 2007;59(5):1001–4.
Peleg AY, Potoski BA, Rea R, Adams J, Sethi J, Capitano B, et al. Acinetobacter baumannii bloodstream infection while receiving tigecycline: a cautionary report. J Antimicrob Chemother. 2007;59(1):128–31.
Muralidharan G, Micalizzi M, Speth J, Raible D, Troy S. Pharmacokinetics of tigecycline after single and multiple doses in healthy subjects. Antimicrob Agents Chemother. 2005;49(1):220–9.
Kim NH, Hwang JH, Song KH, Choe PG, Kim ES, Park SW, et al. Tigecycline in carbapenem-resistant Acinetobacter baumannii bacteraemia: susceptibility and clinical outcome. Scand J Infect Dis. 2013;45(4):315–9.
Nix DE, Matthias KR. Should tigecycline be considered for urinary tract infections? A pharmacokinetic re-evaluation. J Antimicrob Chemother. 2010;65(6):1311–2.
Freire AT, Melnyk V, Kim MJ, Datsenko O, Dzyublik O, Glumcher F, et al. Comparison of tigecycline with imipenem/cilastatin for the treatment of hospital-acquired pneumonia. Diagn Microbiol Infect Dis. 2010;68(2):140–51.
Pichardo C, Pachon-Ibanez ME, Docobo-Perez F, Lopez-Rojas R, Jimenez-Mejias ME, Garcia-Curiel A, et al. Efficacy of tigecycline vs. imipenem in the treatment of experimental Acinetobacter baumannii murine pneumonia. Eur J Clin Microbiol Infect Dis. 2010;29(5):527–31.
Ramirez J, Dartois N, Gandjini H, Yan JL, Korth-Bradley J, McGovern PC. Randomized phase 2 trial to evaluate the clinical efficacy of two high-dosage tigecycline regimens versus imipenem-cilastatin for treatment of hospital-acquired pneumonia. Antimicrob Agents Chemother. 2013;57(4):1756–62.
Lee YT, Tsao SM, Hsueh PR. Clinical outcomes of tigecycline alone or in combination with other antimicrobial agents for the treatment of patients with healthcare-associated multidrug-resistant Acinetobacter baumannii infections. Eur J Clin Microbiol Infect Dis. 2013;32(9):1211–20.
Anthony KB, Fishman NO, Linkin DR, Gasink LB, Edelstein PH, Lautenbach E. Clinical and microbiological outcomes of serious infections with multidrug-resistant gram-negative organisms treated with tigecycline. Clin Infect Dis. 2008;46(4):567–70.
Reid GE, Grim SA, Aldeza CA, Janda WM, Clark NM. Rapid development of Acinetobacter baumannii resistance to tigecycline. Pharmacotherapy. 2007;27(8):1198–201.
Testa RT, Petersen PJ, Jacobus NV, Sum PE, Lee VJ, Tally FP. In vitro and in vivo antibacterial activities of the glycylcyclines, a new class of semisynthetic tetracyclines. Antimicrob Agents Chemother. 1993;37(11):2270–7.
Agwuh KN, MacGowan A. Pharmacokinetics and pharmacodynamics of the tetracyclines including glycylcyclines. J Antimicrob Chemother. 2006;58(2):256–65.
Pei G, Mao Y, Sun Y. In vitro activity of minocycline alone and in combination with cefoperazone-sulbactam against carbapenem-resistant Acinetobacter baumannii. Microb Drug Resist. 2012;18(6):574–7.
Liang W, Liu XF, Huang J, Zhu DM, Li J, Zhang J. Activities of colistin- and minocycline-based combinations against extensive drug resistant Acinetobacter baumannii isolates from intensive care unit patients. BMC Infect Dis. 2011;11:109.
Griffith ME, Yun HC, Horvath LL, Murray CK. Minocycline therapy for traumatic wound infections caused by the multidrug-resistant Acinetobacter baumannii–Acinetobacter calcoaceticus complex. Infect Dis Clin Pract. 2008;16:16–9.
Wood GC, Hanes SD, Boucher BA, Croce MA, Fabian TC. Tetracyclines for treating multidrug-resistant Acinetobacter baumannii ventilator-associated pneumonia. Intensive Care Med. 2003;29(11):2072–6.
Chan JD, Graves JA, Dellit TH. Antimicrobial treatment and clinical outcomes of carbapenem-resistant Acinetobacter baumannii ventilator-associated pneumonia. J Intensive Care Med. 2010;25(6):343–8.
Song JY, Kee SY, Hwang IS, Seo YB, Jeong HW, Kim WJ, et al. In vitro activities of carbapenem/sulbactam combination, colistin, colistin/rifampicin combination and tigecycline against carbapenem-resistant Acinetobacter baumannii. J Antimicrob Chemother. 2007;60(2):317–22.
Giamarellos-Bourboulis EJ, Xirouchaki E, Giamarellou H. Interactions of colistin and rifampin on multidrug-resistant Acinetobacter baumannii. Diagn Microbiol Infect Dis. 2001;40(3):117–20.
Pachon-Ibanez ME, Docobo-Perez F, Lopez-Rojas R, Dominguez-Herrera J, Jimenez-Mejias ME, Garcia-Curiel A, et al. Efficacy of rifampin and its combinations with imipenem, sulbactam, and colistin in experimental models of infection caused by imipenem-resistant Acinetobacter baumannii. Antimicrob Agents Chemother. 2010;54(3):1165–72.
Pantopoulou A, Giamarellos-Bourboulis EJ, Raftogannis M, Tsaganos T, Dontas I, Koutoukas P, et al. Colistin offers prolonged survival in experimental infection by multidrug-resistant Acinetobacter baumannii: the significance of co-administration of rifampicin. Int J Antimicrob Agents. 2007;29(1):51–5.
Bassetti M, Repetto E, Righi E, Boni S, Diverio M, Molinari MP, et al. Colistin and rifampicin in the treatment of multidrug-resistant Acinetobacter baumannii infections. J Antimicrob Chemother. 2008;61(2):417–20.
Aydemir H, Akduman D, Piskin N, Comert F, Horuz E, Terzi A, et al. Colistin vs. the combination of colistin and rifampicin for the treatment of carbapenem-resistant Acinetobacter baumannii ventilator-associated pneumonia. Epidemiol Infect. 2013;141(6):1214–22.
Durante-Mangoni E, Signoriello G, Andini R, Mattei A, De Cristoforo M, Murino P, et al. Colistin and rifampicin compared with colistin alone for the treatment of serious infections due to extensively drug-resistant Acinetobacter baumannii: a multicenter, randomized clinical trial. Clin Infect Dis. 2013;57(3):349–58.
Falagas ME, Kanellopoulou MD, Karageorgopoulos DE, Dimopoulos G, Rafailidis PI, Skarmoutsou ND, et al. Antimicrobial susceptibility of multidrug-resistant Gram negative bacteria to fosfomycin. Eur J Clin Microbiol Infect Dis. 2008;27(6):439–43.
Santimaleeworagun W, Wongpoowarak P, Chayakul P, Pattharachayakul S, Tansakul P, Garey KW. In vitro activity of colistin or sulbactam in combination with fosfomycin or imipenem against clinical isolates of carbapenem-resistant Acinetobacter baumannii producing OXA-23 carbapenemases. Southeast Asian J Trop Med Public Health. 2011;42(4):890–900.
Sirijatuphat R, Thamlikitkul V. Colistin versus colistin plus fosfomycin for treatment of carbapenem-resistant Acinetobacter baumannii infections: a preliminary study. Antimicrob Agents Chemother. 2014; in press.
Li J, Nation RL, Owen RJ, Wong S, Spelman D, Franklin C. Antibiograms of multidrug-resistant clinical Acinetobacter baumannii: promising therapeutic options for treatment of infection with colistin-resistant strains. Clin Infect Dis. 2007;45(5):594–8.
Hornsey M, Wareham DW. In vivo efficacy of glycopeptide-colistin combination therapies in a Galleria mellonella model of Acinetobacter baumannii infection. Antimicrob Agents Chemother. 2011;55(7):3534–7.
Hornsey M, Phee L, Longshaw C, Wareham DW. In vivo efficacy of telavancin/colistin combination therapy in a Galleria mellonella model of Acinetobacter baumannii infection. Int J Antimicrob Agents. 2013;41(3):285–7.
O’Hara JA, Ambe LA, Casella LG, Townsend BM, Pelletier MR, Ernst RK, et al. Activities of vancomycin-containing regimens against colistin-resistant Acinetobacter baumannii clinical strains. Antimicrob Agents Chemother. 2013;57(5):2103–8.
Galani I, Orlandou K, Moraitou H, Petrikkos G, Souli M. Colistin/daptomycin: an unconventional antimicrobial combination synergistic in vitro against multidrug-resistant Acinetobacter baumannii. Int J Antimicrob Agents. 2014;43(4):370–4.
Garnacho-Montero J, Amaya-Villar R, Gutierrez-Pizarraya A, Espejo-Gutierrez de Tena E, Artero-Gonzalez ML, Corcia-Palomo Y, et al. Clinical efficacy and safety of the combination of colistin plus vancomycin for the treatment of severe infections caused by carbapenem-resistant Acinetobacter baumannii. Chemotherapy. 2013;59(3):225–31.
Petrosillo N, Giannella M, Antonelli M, Antonini M, Barsic B, Belancic L, et al. Clinical experience of colistin–glycopeptide combination in critically ill patients infected with gram-negative bacteria. Antimicrob Agents Chemother. 2014;58(2):851–8.
Lesho E, Yoon EJ, McGann P, Snesrud E, Kwak Y, Milillo M, et al. Emergence of colistin-resistance in extremely drug-resistant Acinetobacter baumannii containing a novel pmrCAB operon during colistin therapy of wound infections. J Infect Dis. 2013;208(7):1142–51.
Snitkin ES, Zelazny AM, Gupta J, Program NCS, Palmore TN, Murray PR, et al. Genomic insights into the fate of colistin resistance and Acinetobacter baumannii during patient treatment. Genome Res. 2013;23(7):1155–62.
Shields RK, Clancy CJ, Gillis LM, Kwak EJ, Silveira FP, Massih RC, et al. Epidemiology, clinical characteristics and outcomes of extensively drug-resistant Acinetobacter baumannii infections among solid organ transplant recipients. PLoS One. 2012;7(12):e52349.
Falagas ME, Rafailidis PI, Ioannidou E, Alexiou VG, Matthaiou DK, Karageorgopoulos DE, et al. Colistin therapy for microbiologically documented multidrug-resistant Gram-negative bacterial infections: a retrospective cohort study of 258 patients. Int J Antimicrob Agents. 2010;35(2):194–9.
Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34(6):1589–96.
Micek ST, Welch EC, Khan J, Pervez M, Doherty JA, Reichley RM, et al. Empiric combination antibiotic therapy is associated with improved outcome against sepsis due to Gram-negative bacteria: a retrospective analysis. Antimicrob Agents Chemother. 2010;54(5):1742–8.
Lee YT, Kuo SC, Yang SP, Lin YT, Tseng FC, Chen TL, et al. Impact of appropriate antimicrobial therapy on mortality associated with Acinetobacter baumannii bacteremia: relation to severity of infection. Clin Infect Dis. 2012;55(2):209–15.
Erbay A, Idil A, Gozel MG, Mumcuoglu I, Balaban N. Impact of early appropriate antimicrobial therapy on survival in Acinetobacter baumannii bloodstream infections. Int J Antimicrob Agents. 2009;34(6):575–9.
de Gouvea EF, Martins IS, Halpern M, Ferreira AL, Basto ST, Goncalves RT, et al. The influence of carbapenem resistance on mortality in solid organ transplant recipients with Acinetobacter baumannii infection. BMC Infect Dis. 2012;12:351.
Acknowledgments
This work was supported in part by a research grant from the National Institutes of Health to Y.D. (R01AI104895). Y.D. has received a research grant from Merck and has served on an advisory board for Shionogi. J.A.V. has no potential conflicts of interest. M.H.N. has no potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Viehman, J.A., Nguyen, M.H. & Doi, Y. Treatment Options for Carbapenem-Resistant and Extensively Drug-Resistant Acinetobacter baumannii Infections. Drugs 74, 1315–1333 (2014). https://doi.org/10.1007/s40265-014-0267-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-014-0267-8