Abstract
Introduction
Despite the numerous studies investigating drug-induced anaphylaxis (DIA), understanding and quantitative data analysis in developing countries remain limited. The aim of our study is to describe and quantify DIA using the National Pharmacovigilance Database of Vietnam (NPDV).
Methods
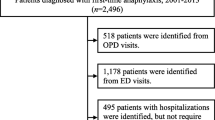
Spontaneous reporting of adverse drug reactions (ADRs) recorded between 2010 and 2016 were retrospectively analysed to identify DIA reports. The trend and characteristics of DIA cases were described. Multivariate disproportionality analysis was used for signal generation.
Results
Overall, 4873 DIA cases (13.2% of total ADRs) were recorded in the NPDV, 111 of which resulted in death (82% of total ADR-induced deaths) over a 7-year period. There was a remarkable increase in DIA reporting over time (p < 0.001). The incidence rates of DIA reporting per total ADRs and per 100,000 inhabitants remained high (mean rates [95% CI] of 12.06 [9.88–14.24] and 0.77 [0.33–1.20], respectively). Concerning suspected drugs, systemic antibiotics (n = 3318, 68%) were mostly reported with a reporting odds ratio (ROR) and 95% CI of 2.35 [2.20–2.51]. In the case of antibiotic-induced anaphylaxis, the third-generation cephalosporins were predominant (n = 1961, 40.2%, ROR 2.39 [2.24–2.55]). We also noted drugs generally associated with DIA such as contrast agents (ROR 2.43 [2.04–2.88]) and anaesthetics (ROR 4.02 [3.30–4.89]). Furthermore, unexpected signals were observed for alpha-chymotrypsin (ROR 1.75 [1.23–2.44]) and amoxicillin/sulbactam (ROR 1.59 [1.18–2.10]), uncommonly reported in western countries.
Conclusion
In recent years, cases of drug-induced DIA have increased in Vietnam, mostly due to antibiotics and third-generation cephalosporins. The inappropriate use of these drugs should be taken into account. Our findings also highlighted typical Vietnamese signals for alpha-chymotrypsin- and amoxicillin/sulbactam-induced anaphylaxis, which may relate to a specific sociological context in resource-limited countries.







Similar content being viewed by others
References
Johansson SGO, Bieber T, Dahl R, Friedmann PS, Lanier BQ, Lockey RF, et al. Revised nomenclature for allergy for global use: Report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J. Allergy Clin. Immunol. 2004;113:832–6.
Sampson HA, Muñoz-Furlong A, Campbell RL, Adkinson NF, Bock SA, Branum A, et al. Second symposium on the definition and management of anaphylaxis: Summary report—Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J. Allergy Clin. Immunol. 2006;117:391–7.
Ribeiro-Vaz I, Marques J, Demoly P, Polónia J, Gomes ER. Drug-induced anaphylaxis: a decade review of reporting to the Portuguese Pharmacovigilance Authority. Eur. J. Clin. Pharmacol. 2013;69:673–81.
Aronson JK, Ferner RE. Joining the DoTS: new approach to classifying adverse drug reactions. BMJ. 2003;327:1222–5.
Tang MLK, Osborne N, Allen K. Epidemiology of anaphylaxis. Curr. Opin. Allergy Clin. Immunol. 2009;9:351–6.
Bochner BS, Lichtenstein LM. Anaphylaxis. N. Engl. J. Med. 1991;324:1785–90.
Mertes PM, Guttormsen AB, Harboe T, Johansson SGO, Florvaag E, Husum B, et al. Can spontaneous adverse event reporting systems really be used to compare rates of adverse events between drugs? Anesth. Analg. 2007;104:471–2.
Ministry of Health. Circular 51/2017/TT-BYT Guidelines on prevention, diagnosis and management of anaphylaxis. 2017. http://canhgiacduoc.org.vn/SiteData/3/UserFiles/Thong%20tu%20Huong%20dan%20phong,%20chan%20doan%20va%20xu%20tri%20soc%20phan%20ve%202017.pdf.
Le TTL. Evaluation of signal detection and management of anaphylactic reactions from spontaneous reporting database in Vietnam [Thesis in Vietnamese]. Hanoi University of Pharmacy. 2015.
Dang BV, Nguyen TB, Nguyen HA, Tran TN, Vo TTT, Pham PL. Analysis of antibiotic-associated anaphylaxis in Vietnam in the period of 2010 – 2015 [in Vietnamese]. Pharmacology Research and Drug Information Journal (ISSN 1859-364X). http://www.hup.edu.vn/cpbdv/pqlkh/noidung/Lists/TapchiNCDTTT/View_Detail.aspx?ItemID=22. Accessed 15 May 2018.
Nguyen K-D, Nguyen P-T, Nguyen H-A, Roussin A, Montastruc J-L, Bagheri H, et al. Overview of pharmacovigilance system in Vietnam: lessons learned in a resource-restricted Country. Drug Saf. 2018;41:151–9.
ICH. Efficacy Guidelines: E2A-E2F Pharmacovigilance. 2018. http://www.ich.org/products/guidelines/efficacy/article/efficacy-guidelines.html. Accessed 29 Jun 2018.
Ministry of Health. National Guideline of Pharmacovigilance. According to Decision 2111/QD-BYT from Ministry of Health (Vietnam). 2015. http://canhgiacduoc.org.vn/SiteData/3/UserFiles/HDQGCGD%20Final%2029_05_2015.pdf. Accessed 24 Dec 2016.
WHO Collaborating Centre for International Drug Monitoring. WHO Adverse Reaction Terminology (WHO-ART). 2012. http://www.umc-products.com/. Accessed 18 Sep 2017.
Olsson S. The role of the WHO programme on international drug monitoring in coordinating worldwide drug safety efforts. Drug Saf. 1998;19:1–10.
Moore N, Kreft-Jais C, Haramburu F, Noblet C, Andrejak M, Ollagnier M, et al. Reports of hypoglycaemia associated with the use of ACE inhibitors and other drugs: a case/non-case study in the French pharmacovigilance system database. Br J Clin Pharmacol. 1997;44:513–8.
van Puijenbroek EP, Bate A, Leufkens HGM, Lindquist M, Orre R, Egberts ACG. A comparison of measures of disproportionality for signal detection in spontaneous reporting systems for adverse drug reactions. Pharmacoepidemiol. Drug Saf. 2002;11:3–10.
Faillie J-L. Case-non case studies: principles, methods, bias and interpretation [Article in French]. Therapie. 2018;73:247–55.
EMA. Screening for adverse reactions in EudraVigilance (EMA/849944/2016). 2016. https://www.ema.europa.eu/documents/other/screening-adverse-reactions-eudravigilance_en.pdf.
General Statistics Office of Vietnam. Population and employment : area, population and population density by province. www.gso.gov.vn2017. https://www.gso.gov.vn/default_en.aspx?tabid=774. Accessed 10 Oct 2017.
CRAN. R: The R Project for Statistical Computing. 2017. https://www.r-project.org/. Accessed 30 Aug 2017.
US Department of Commerce. US Census Bureau: Population. 2017. https://www.census.gov/data-tools/demo/idb/region.php?N=%20Results%20&T=3&A=separate&RT=0&Y=2010,2011,2012,2013,2014,2015,2016&R=-1&C=VM. Accessed 28 Jun 2018.
Decker WW, Campbell RL, Manivannan V, Luke A, St Sauver JL, Weaver A, et al. The etiology and incidence of anaphylaxis in Rochester, Minnesota: a report from the Rochester Epidemiology Project. J. Allergy Clin. Immunol. 2008;122:1161–5.
Thong BY-H, Tan T-C. Epidemiology and risk factors for drug allergy. Br J Clin Pharmacol. 2011;71:684–700.
Hazell L, Shakir SAW. Under-reporting of adverse drug reactions : a systematic review. Drug Saf. 2006;29:385–96.
Leone R, Conforti A, Venegoni M, Motola D, Moretti U, Meneghelli I, et al. Drug-induced anaphylaxis : case/non-case study based on an italian pharmacovigilance database. Drug Saf. 2005;28:547–56.
Zhao Y, Sun S, Li X, Ma X, Tang H, Sun L, et al. Drug-induced anaphylaxis in China: a 10 year retrospective analysis of the Beijing Pharmacovigilance Database. Int J Clin Pharm. 2017. https://doi.org/10.1007/s11096-017-0535-2.
Liew WK, Williamson E, Tang MLK. Anaphylaxis fatalities and admissions in Australia. J Allergy Clin Immunol. 2009;123:434–42.
Park H-K, Kang M-G, Yang M-S, Jung J-W, Cho S-H, Kang H-R. Epidemiology of drug-induced anaphylaxis in a tertiary hospital in Korea. Allergol Int. 2017;66:557–62.
Moore N, Kreft-Jais C, Haramburu F, Noblet C, Andrejak M, Ollagnier M, et al. Reports of hypoglycaemia associated with the use of ACE inhibitors and other drugs: a case/non-case study in the French pharmacovigilance system database. Br J Clin Pharmacol. 1997;44:513–8.
Wang DY, Forslund C, Persson U, Wiholm BE. Drug-attributed anaphylaxis. Pharmacoepidemiol Drug Saf. 1998;7:269–74.
Trinh HT, Nguyen HTL, Pham VTT, Ba HL, Dong PTX, Cao TTB, et al. Hospital clinical pharmacy services in Vietnam. Int J Clin Pharm. 2018;20:33. https://doi.org/10.1007/s11096-018-0633-9.
van Grootheest K, van Puijenbroek EP, de Jong-van den Berg LTW. Do pharmacists’ reports of adverse drug reactions reflect patients’ concerns? Pharm World Sci. 2004;26:155–9.
van Grootheest AC, de Jong-van den Berg LTW. The role of hospital and community pharmacists in pharmacovigilance. Res Social Adm Pharm. 2005;1:126–33.
Montastruc J-L, Lapeyre-Mestre M, Bagheri H, Fooladi A. Gender differences in adverse drug reactions: analysis of spontaneous reports to a Regional Pharmacovigilance Centre in France. Fundam Clin Pharmacol. 2002;16:343–6.
Nguyen KV, Thi Do NT, Chandna A, Nguyen TV, Pham CV, Doan PM, et al. Antibiotic use and resistance in emerging economies: a situation analysis for Viet Nam. BMC Public Health. 2013;13:1158.
Phu VD, Wertheim HFL, Larsson M, Nadjm B, Dinh Q-D, Nilsson LE, et al. Burden of Hospital Acquired Infections and Antimicrobial Use in Vietnamese Adult Intensive Care Units. PLoS One. 2016;11:e0147544.
Thu TA, Rahman M, Coffin S, Harun-Or-Rashid M, Sakamoto J, Hung NV. Antibiotic use in Vietnamese hospitals: a multicenter point-prevalence study. Am J Infect Control. 2012;40:840–4.
Chu QT. Trends on imported medicine and associated factors during 2006–2014 [Doctoral Thesis in Vietnamese Code 62.72.04.12]. 2017.
Salvo F, Polimeni G, Cutroneo P, Leone R, Confortic A, Moretti U, et al. Allergic reactions to oral drugs: a case/non-case study from an Italian spontaneous reporting database (GIF). Pharmacol. Res. 2008;58:202–7.
Minh NT, Tuyến NT, Thắng TN, Hùng DĐ, Nga CT, Phương NT, et al. Survey on the consumption of carbapenem in Bach Mai Hospital in the period 2012–2016 [in Vietnamese]. Vietnam Pharm. J. 2017;57:63–6.
Mao W, Vu H, Xie Z, Chen W, Tang S. Systematic review on irrational use of medicines in China and Vietnam. PLOS One. 2015;10:e0117710.
Johnston A, Holt DW. Substandard drugs: a potential crisis for public health. Br J Clin Pharmacol. 2014;78:218–43.
Trippe ZA, Brendani B, Meier C, Lewis D. Identification of substandard medicines via disproportionality analysis of individual case safety reports. Drug Saf. 2017;40:293–303.
Juhlin K, Karimi G, Andér M, Camilli S, Dheda M, Har TS, et al. Using VigiBase to identify substandard medicines: detection capacity and key prerequisites. Drug Saf. 2015;38:373–82.
Cheema RK. Seven people die after dialysis treatment in Vietnam. 2017. https://today.mims.com/seven-people-die-after-dialysis-treatment-in-vietnam. Accessed 21 May 2018.
Milbert AH. Infusion reactions with special reference to “speed shock”. Am J Surg. 1934;26:479–85.
Hirshfeld S, Hyman HT, Wanger JJ. Influence of velocity on the response to intravenous injections. Arch Intern Med (Chic). 1931;47:259–87.
Van Tuong P, Phuong TTM, Anh BTM, Nguyen THT. Assessment of injection safety in Ha Dong General Hospital, Hanoi, in 2012. F1000Res. 2017 https://doi.org/10.12688/f1000research.11399.4.
Nguyen H-T, Nguyen T-D, van den Heuvel ER, Haaijer-Ruskamp FM, Taxis K. Medication errors in Vietnamese Hospitals: prevalence, potential outcome and associated factors. PLOS One. 2015;10:e0138284.
Fahimi F, Ariapanah P, Faizi M, Shafaghi B, Namdar R, Ardakani MT. Errors in preparation and administration of intravenous medications in the intensive care unit of a teaching hospital: an observational study. Aust Crit Care. 2008;21:110–6.
Ralph Edwards I. Causality assessment in pharmacovigilance: still a challenge. Drug Saf. 2017;40:365–72.
Tomasiak-Łozowska MM, Klimek M, Lis A, Moniuszko M, Bodzenta-Łukaszyk A. Markers of anaphylaxis—a systematic review. Adv Med Sci. 2018;63:265–77.
Grundmark B, Isah AO. Chymotrypsin and anaphylactic shock, a continuing safety issue. Upps. Monit. Cent.—WHO Signal. 2016:5–7.
The Uppsala Monitoring Centre. VigiBase®. 2018. https://www.who-umc.org/vigibase/vigibase/. Accessed 18 Jul 2018.
Rägo L, Santoso B. Drug regulation: history, present and future. In: Drug benefits and risks: international textbook of clinical pharmacology. IOS Press and Uppsala Monitoring Centre. 2008. http://www.who.int/medicines/technical_briefing/tbs/Drug_Regulation_History_Present_Future.pdf. Accessed 18 Sep 2018.
National Assembly of Vietnam. Law on pharmacy revised. 2016. http://vbpl.vn/TW/Pages/vbpqen-toanvan.aspx?ItemID=11099. Accessed 1 Jul 2016.
Caimmi S, Caimmi D, Bernardini R, Caffarelli C, Crisafulli G, Pingitore G, et al. Perioperative anaphylaxis: epidemiology. Int J Immunopathol Pharmacol. 2011;24:S21–6.
Katayama H, Yamaguchi K, Kozuka T, Takashima T, Seez P, Matsuura K. Adverse reactions to ionic and nonionic contrast media. A report from the Japanese Committee on the Safety of Contrast Media. Radiology. 1990;175:621–8.
Maddox TG. Adverse reactions to contrast material: recognition, prevention, and treatment. Am Fam Physician. 2002;66:1229–34.
Mertes PM, Volcheck GW, Garvey LH, Takazawa T, Platt PR, Guttormsen AB, et al. Epidemiology of perioperative anaphylaxis. Presse Méd. 2016;45:758–67.
Montañez MI, Mayorga C, Bogas G, Barrionuevo E, Fernandez-Santamaria R, Martin-Serrano A, et al. Epidemiology, mechanisms, and diagnosis of drug-induced anaphylaxis. Front Immunol. 2017;8:614.
Nghiem TTL. La prophylaxie d’ulcère de stress par les inhibiteurs de la pompe à protons: Étude de bon usage à l’hôpital Thanh Nhan, Hanoi. 2015. http://canhgiacduoc.org.vn/SiteData/3/UserFiles/LV%202015%20Nghien%20Thi%20Thuy%20Linh-%20Mekong.pdf. Accessed 18 July 2018.
Chiem J, Ivanova I, Parker A, Krengel W, Jimenez N. Anaphylactic reaction to tranexamic acid in an adolescent undergoing posterior spinal fusion. Paediatr Anaesth. 2017;27:774–5.
Li PH, Trigg C, Rutkowski R, Rutkowski K. Anaphylaxis to tranexamic acid-a rare reaction to a common drug. J Allergy Clin Immunol Pract. 2017;5:839–41.
Renaudin J-M, Beaudouin E, Ponvert C, Demoly P, Moneret-Vautrin D-A. Severe drug-induced anaphylaxis: analysis of 333 cases recorded by the Allergy Vigilance Network from 2002 to 2010. Allergy. 2013;68:929–37.
González-Pérez A, Aponte Z, Vidaurre CF, Rodríguez LAG. Anaphylaxis epidemiology in patients with and patients without asthma: a United Kingdom database review. J. Allergy Clin. Immunol. 2010;125(1098–1104):e1.
Takazawa T, Oshima K, Saito S. Drug induced anaphylaxis in the emergency room. Acute Med Surg. 2017;4:235–45.
Author information
Authors and Affiliations
Contributions
Study designed by H-AN, D-HN, T-BN. Research carried out by K-DN, TT-LL, H-AN (Jr), B-VD, T-NN. Data analysed by K-DN. New methods or models contributed by K-DN, H-AN, HB, D-HV. Paper written by K-DN, H-AN, D-HV, J-LM, HB.
Corresponding author
Ethics declarations
Funding
The National Centre for Drug Information and Adverse Drug Reaction Monitoring acknowledges support from the National WHO Office in Vietnam (involved in signal detection: WHO Reference 2017/716670-0; PO Number 201735388). Khac-Dung Nguyen acknowledges the French Embassy in Hanoi and the Pierre Fabre Foundation for their financial support of his doctoral studies at the UMR 1027 INSERM–University Toulouse III, France, in close collaboration with the National Centre for Drug Information and Adverse Drug Reaction Monitoring, Hanoi University of Pharmacy, Hanoi, Vietnam. No other sources of funding were used to assist in the preparation of this article.
Conflict of interest
Khac-Dung Nguyen, Hoang-Anh Nguyen, Dang-Hoa Nguyen, Thanh-Binh Nguyen, Dinh-Hoa Vu, Thi Thuy-Linh Le, Hoang-Anh Nguyen (Jr), Bich-Viet Dang, Trung-Nguyen Nguyen, Jean-Louis Montastruc, and Haleh Bagheri have no conflicts of interest that are directly relevant to the content of this manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nguyen, KD., Nguyen, HA., Vu, DH. et al. Drug-Induced Anaphylaxis in a Vietnamese Pharmacovigilance Database: Trends and Specific Signals from a Disproportionality Analysis. Drug Saf 42, 671–682 (2019). https://doi.org/10.1007/s40264-018-0758-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-018-0758-8