Abstract
Introduction
Rosuvastatin pharmacokinetics is mainly dependent on the activity of hepatic uptake transporter OATP1B1. In this study, we aimed to investigate and disentangle the effect of Roux-en-Y gastric bypass (RYGB) and weight loss on oral clearance (CL/F) of rosuvastatin as a measure of OATP1B1-activity.
Methods
Patients with severe obesity preparing for RYGB (n = 40) or diet-induced weight loss (n = 40) were included and followed for 2 years, with four 24-hour pharmacokinetic investigations. Both groups underwent a 3-week low-energy diet (LED; < 1200 kcal/day), followed by RYGB or a 6-week very-low-energy diet (VLED; < 800 kcal/day).
Results
A total of 80 patients were included in the RYGB group (40 patients) and diet-group (40 patients). The weight loss was similar between the groups following LED and RYGB. The LED induced a similar (mean [95% CI]) decrease in CL/F in both intervention groups (RYGB: 16% [0, 31], diet: 23% [8, 38]), but neither induced VLED resulted in any further changes in CL/F. At Year 2, CL/F had increased by 21% from baseline in the RYGB group, while it was unaltered in the diet group. Patients expressing the reduced function SLCO1B1 variants (c.521TC/CC) showed similar changes in CL/F over time compared with patients expressing the wild-type variant.
Conclusions
Neither body weight, weight loss nor RYGB per se seem to affect OATP1B1 activity to a clinically relevant degree. Overall, the observed changes in rosuvastatin pharmacokinetics were minor, and unlikely to be of clinical relevance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Both surgery and diet intervention led to a matched weight loss between the study groups. |
Roux-en-Y gastric bypass surgery does not affect OATP1B1 activity in patients with severe obesity. |
No dose adjustments of rosuvastatin appear to be necessary following weight loss induced by bariatric surgery and/or low-calorie diet. |
1 Introduction
Obesity represents a global epidemic [1], and is associated with an increased risk of comorbidities including type 2 diabetes, cardiovascular disease and cancer that often requires pharmacological treatment [2, 3]. Severe obesity is classified as a body mass index (BMI) between 35.0 and 39.9 kg/m2 in combination with comorbidity, or ≥ 40 kg/m2, for which weight loss is the primary treatment [4]. Bariatric surgery has shown superior effects with respect to achieving long-lasting weight loss and improvement of comorbidities compared to non-surgical interventions in patients with severe obesity [5, 6]. The Roux-en-Y gastric bypass (RYGB) procedure reduces the proximal stomach, and the duodenum and proximal intestine are bypassed [7, 8]. Due to this gastrointestinal rearrangement, drug absorption and disposition may be altered. Altered gastric pH, reduced transit-time, and decreased surface area for passive and active absorption, as well as the bypassing of intestinal segments rich in drug-metabolising enzymes and transporters, are among the suggested mechanisms leading to variable drug disposition following RYGB [9].
The 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase inhibitor, rosuvastatin, is a commonly used lipid-lowering agent. Rosuvastatin is more hydrophilic compared with most other statins, and it displays a low degree of passive diffusion into tissues [10]. The hepatic uptake transporters organic-anion transporting polypeptides (OATP) 1B1 (SLCO1B1), OATP1B3 (SLCO1B3), OATP2B1 (SLCO2B1), as well as the sodium taurocholate co-transporting polypeptide (NTCP; SLC10A1) transport rosuvastatin into the hepatocytes. Organic-anion transporting polypeptides 1B1 contributes to 49–86% of rosuvastatin hepatic uptake, and rosuvastatin is thus considered an established and preferred probe drug to study OATP1B1 activity [11,12,13]. Rosuvastatin is sparsely metabolised, and the majority of the absorbed dose is excreted unchanged in faeces (~ 76%). Hepatic elimination accounts for approximately 70% of total clearance of rosuvastatin, with biliary excretion, mediated by canalicular transporters such as breast cancer resistance protein (BCRP; ABCG2) and permeability-glycoprotein (P-gp; ABCB1), as the main clearance mechanism [14, 15]. Genetic polymorphisms of the key hepatic uptake transporter OATP1B1 have been shown to influence rosuvastatin disposition. The single-nucleotide polymorphism (SNP) c.521T>C in SLCO1B1 is associated with decreased membrane expression of OATP1B1 in vivo [16]. Consequently, systemic exposure of rosuvastatin is reported to be 19–68% higher in patients with c.521TC or c.521CC [17].
In patients with a wide range of body weight, using midazolam as a probe drug, both the activity and protein expression of the quantitatively most important drug metabolising enzyme, cytochrome P450 (CYP) 3A, have been shown to be inversely associated with body weight. This was hypothesised to be due to low-grade inflammation and/or non-alcoholic fatty liver disease (NAFLD) [18,19,20]. Inflammatory cytokines such as interleukin (IL) 6 and tumour necrosis factor alpha (TNF-α), as well as NAFLD have been associated with lower expression and activity of several CYP enzymes [18, 21]. However, there are limited data regarding the effect of weight loss, inflammation, and NAFLD on drug transporters. The primary aim of this work was to study the short- (6 weeks) and long-term (2 years) effects of weight loss induced by strict diet or RYGB on OATP1B1 activity by investigating the pharmacokinetics of rosuvastatin, and to secondary compare OATP1B1 activity in a control group of normal-to-overweight individuals with patients with severe obesity.
2 Methods
2.1 Study Design and Patients
The COCKTAIL study, a non-randomised, single-centre, 3-armed study, was carried out at the Morbid Obesity Centre, Vestfold Hospital Trust, Norway [22]. Patients with severe obesity (BMI ≥ 35 kg/m2 in combination with comorbidity or BMI ≥ 40 kg/m2) scheduled for elective weight-reducing intervention by either RYGB or strict diet were eligible for inclusion. The inclusion and exclusion criteria are fully described in the protocol paper [22]. Additionally, normal-to-overweight (BMI 18.5–29.9 kg/m2) individuals scheduled for cholecystectomy were included as a cross-sectional control group. The study was approved by the Regional Committee for Medical and Health Research Ethics (2013/2379/REK) and performed in accordance with Good Clinical Practice and the Declaration of Helsinki (NCT02386917). Written informed consent was obtained prior to study participation.
2.2 Study Visits and Procedures
The patient flow in the study has been described previously [20], and is further detailed in Figure S1. Both the RYGB group and the diet group were prescribed an initial 3-week low-energy diet (LED; < 1200 kcal/day), followed by additional 6 weeks of strict caloric restriction (< 800 kcal/day) induced by surgery or a very-low energy diet (VLED), respectively, in order to obtain a similar weight loss between the two groups [22]. All patients were prospectively followed for 2 years. During the study period, four 24-h pharmacokinetic investigations were performed following single oral administration of 20 mg rosuvastatin. Blood samples were obtained via a peripheral venous catheter before and 0.25, 0.5, 1, 1.5, 2, 3, 4, 4.25, 4.5, 5, 5.5, 6, 8, 10, 12, 23, and 24 h post-dose. The investigations were performed at baseline (Week 0); after the 3-week LED (Week 3); after additional 6-week strict calorie restriction (Week 9), and after 2 years (Year 2). For the RYGB group, the investigation at Week 3 was performed the day before surgery. The cross-sectional control group of normal-to-overweight individuals underwent a single 24-h pharmacokinetic study the day before cholecystectomy (Week 0). Hepatic and jejunal biopsies were obtained at the day of surgery in the RYGB group, and hepatic biopsies were obtained in the normal-to-overweight control group at the day of surgery as previously described [23].
2.3 Outcomes
The primary outcomes were short- (Week 3 to Week 9) and long-term (Week 3 to Year 2) changes in oral clearance of rosuvastatin, as a measure of OATP1B1 activity. Secondary outcomes included changes in rosuvastatin pharmacokinetics over time following RYGB or strict diet, assessed by oral clearance, maximum concentration (Cmax) and time to maximum concentration (Tmax), as well as hepatic concentration of OATP1B1.
2.4 Analytical Assay
Plasma concentrations of rosuvastatin were determined by Covance Laboratories (Madison, Wisconsin, USA), as previously described [24]. In brief, buffered plasma samples were extracted by supported liquid extraction. After evaporation, the residue was reconstituted and analysed with liquid chromatography tandem mass spectrometry (LC-MS/MS). The analyte was separated on a C18-column (Aquasil) with a gradient mobile phase of acetonitrile and 0.1% formic acid, using a LC system from Thermo Electron Corporation. Rosuvastatin was detected by MS/MS using a Sciex API 5500 with positive electrospray ionisation, monitoring the m/z 482.2–258.2 transition. The standard curve ranged from 0.04 to 40 ng/mL, using a human plasma sample volume of 0.1 mL. The assay variation coefficients of the rosuvastatin analysis were 7.1%, 4.4% and 4.5% at 0.12 ng/mL, 2 ng/mL, and 20 ng/mL (n = 130), respectively.
2.5 Clinical Chemistry and Genotyping
Clinical chemistry analyses were performed at the Department of Laboratory Medicine, Vestfold Hospital Trust, Tønsberg, Norway. Plasma concentrations of C-reactive protein (CRP) and high-sensitivity CRP (hsCRP) were measured using immunoturbidimetry (Advia Chemistry XPT systems, Siemens) at Fürst Medical Laboratory, Oslo, Norway. Genotyping of SLCO1B1 and ABCG2 variant alleles were performed using Taqman-based real-time polymerase chain reaction assays at the Center for Psychopharmacology, Diakonhjemmet Hospital, Oslo, Norway. The following variant alleles were assessed for SLCO1B1: c.521T>C (rs4149056); ABCG2: V12M variant (rs2231137) and reduced-function Q141K variant (rs2231142). Homozygote carriers of the V12M C/C and Q141K G/G were considered as the wild-type haplotype. A TaqMan assay for rs2231137 genotyping was not readily available, and as such an assay for rs4148150 was used, which is in complete disequilibrium (R2 = 1 in Europeans) with rs2231137 [25].
2.6 Quantification of Hepatic and Intestinal Protein Concentration
Proteins were extracted from small intestinal and liver biopsies in an SDS-containing (2% w/v) lysis buffer and quantified as previously described [26, 27]. In short, samples were processed with the multi-enzyme digestion filter-aided sample preparation protocol, using LysC and trypsin [28]. Proteomics analysis was performed with Q Exactive HF or Q Exactive HF-X MS in data-dependent mode. Mass spectrometry (MS) data were processed with MaxQuant (version 1.6.10.43) [29] where proteins were identified by searching MS and MS/MS data of peptides against the human UniProtKB (UP000005640). Spectral raw intensities were normalised with variance stabilisation [30] and were subsequently used to calculate the protein concentrations using the Total Protein Approach [31]. Batch effects were removed by geometric mean centring of proteins from samples analysed at different time points.
2.7 Population Pharmacokinetic Modelling
A population pharmacokinetic model was developed to determine individual rosuvastatin pharmacokinetics at the different study visits. The purpose of the model was to provide accurate estimates of AUC, oral clearance, maximum concentration (Cmax) and time to maximum concentration (Tmax) in order to allow for a rational assessment of change over time and between groups. In short, a non-parametric adaptive grid approach implemented in a modified version of Pmetrics 1.9.4 [32] for R 3.6.0 was used. In total, 3630 rosuvastatin concentrations corresponding to 197 18-point and 111 9-point 24-h pharmacokinetic profiles from 98 patients were included. Additional model information and metrics are available in the Supplementary file (Figs S2, S3).
2.8 Pharmacokinetic Calculations
Posterior individual parameter values, as well as posterior individually predicted concentrations obtained from the final population pharmacokinetic model run with the complete dataset were used for all pharmacokinetic calculations. Predictions were made in 12-min intervals, and at each sample point. Area under the concentration-time curve from zero to infinity (AUC0–∞) was calculated with the trapezoidal approximation from individual posterior-predicted concentrations using the ‘makeAUC’-function in the Pmetrics package for R. Cmax and Tmax were obtained directly from the individual predictions, while oral clearance was calculated by dividing the dose by the AUC0–∞.
2.9 Statistical Analyses and Calculations
Linear mixed effects models were used to evaluate changes over time with the parameter of choice as the dependent variable, while visit, intervention group, and their interaction were treated as fixed effects. Variant of OATP1B1 was added as a fixed effect when evaluating differences in change over time between genotypes. The unique patient identifier was used as a random effect. Model residuals were evaluated for normality, and if appropriate, the dependent variable was transformed using the natural logarithm. Models with a logarithmically transformed dependent variable were adjusted for the introduced bias. Estimated marginal means and contrasts were used for factor combinations (of visit and intervention group) for all parameters of interest. The cross-sectional analysis at baseline was performed using Welch’s two-sample t test comparing the control group with patients with severe obesity (RYGB group and diet group combined). Baseline rosuvastatin pharmacokinetics were used to assess differences between genotypes. To explore relationships between variables, Pearson’s product-moment correlation was applied. Variables with non-normal distributions (assessed visually) were logarithmically transformed. Predictions of NAFLD and liver fat were performed using metabolic and genetic factors, with NAFLD Liver Fat Score values greater than − 0.640 as a diagnostic of NAFLD [33]. Data are presented as mean ± standard deviation or mean [95% confidence interval (CI)] unless otherwise stated. With the predetermined α = 0.05, 95% CIs not including zero and p values < 0.05 were considered statistically significant. Confidence intervals from linear mixed effects models were adjusted using Tukey method. All statistical analyses were performed using R 4.0.2 [34].
3 Results
3.1 Patient Characteristics
A total of 108 patients (44, 44 and 20 in the RYGB, diet, and control groups, respectively) were included in the study. In the present analyses, 98 patients (40, 40 and 18 in the RYGB, diet, and control group, respectively) supplied at least one 24-h pharmacokinetic profile during the study period.
Mean total body weight at baseline was 132 ± 24 kg, 124 ± 23 kg, and 71 ± 11 kg in the RYGB, diet, and control groups, respectively (Table 1). There were no differences between the groups with respect to age, sex, or ethnicity. Routine clinical chemistry was similar in the three groups, except for higher value of ALT in the intervention groups compared with the control group (Table 1). At baseline, 71 of 98 patients had a NAFLD-score above − 0.640, indicative of NAFLD, in the RYGB (90%), diet (82%) and control groups (11%).
3.2 Changes in Body Weight
The initial 3-week LED resulted in a mean weight loss of 5 ± 2% and 5 ± 2% in the RYGB and diet group, respectively. Total weight loss after the additional 6 weeks of VLED induced by RYGB or strict diet was 13 ± 3% and 11 ± 4%, respectively (Fig. 1). At Year 2, the RYGB group demonstrated a total weight loss of 29 ± 9% from baseline. In contrast, several patients in the diet group had regained body weight at Year 2, resulting in a mean total weight loss from baseline of 3 ± 6% (Fig. 1). The hsCRP and predicted liver fat were similar between the RYGB and diet groups at Weeks 0, 3, and 9, but lower in the RYGB group at Year 2 (Fig. 1).
Groupwise longitudinal overview of change in a total body weight, b high-sensitive C-reactive protein (hsCRP) and c predicted liver fat percentage. For the Roux-en-Y gastric bypass (RYGB) and diet groups, linear mixed model predicted marginal mean and 95% confidence intervals are presented. For the normal-to-overweight control group, observed mean and 95% confidence interval is presented. Comparisons are made between the RYGB and diet groups at each visit, and significant differences are denoted with asterisks. Non-significant differences are not shown *p < 0.05; **p < 0.01; ***p < 0.001
3.3 Baseline Rosuvastatin Pharmacokinetics, Pharmacogenetics, and Proteomics
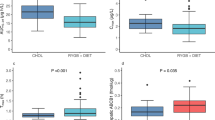
Cross-sectional comparisons of rosuvastatin pharmacokinetics in patients with severe obesity compared with the control group revealed a 0.9 [95% CI 0.4, 1.4] hour shorter Tmax in the normal-to-overweight individuals, with no differences in Cmax or oral clearance (Fig. 2). At baseline, total body weight was not associated with oral clearance (r = 0.17 [95% CI − 0.03, 0.36]). No difference in rosuvastatin oral clearance was observed in patients with NAFLD (n = 69) compared with those without (n = 27), and hsCRP was not associated with oral clearance of rosuvastatin (r = − 0.13 [95% CI − 0.32, 0.07]).
The frequency distribution of SLCO1B1 genetic variants is presented in Table 1, and there were no differences in frequency distribution between the sexes (p = 0.0867). Frequency distribution for the ABCG2 variants are presented in Table S1. Allele frequencies for all sequence variants investigated did not deviate from the Hardy–Weinberg equilibrium. At baseline, patients with SLCO1B1 variant c.521TC (n = 30) or c.521CC (n = 2) demonstrated 30% (p < 0.001) lower oral clearance compared to those with c.521TT. Absolute differences in rosuvastatin oral clearance and systemic exposure within the genetic variants of SLCO1B1 at baseline are presented in Supplementary Tables S2 and S3, respectively.
In the patients undergoing RYGB, hepatic concentration of OATP1B1 was positively associated with oral clearance the day before surgery (r = 0.36 [95% CI 0.04, 0.61]), but this was not the case for the control group (r = − 0.09 [95% CI − 0.54, 0.39]) (Fig. S5). Furthermore, there were no differences in mean hepatic concentration of OATP1B1 between the RYGB (2.7 ± 0.9 fmol/µg) and control groups (2.6 ± 0.9 fmol/µg; p = 0.630), nor were there any differences between individuals in the combined RYGB and control groups with SLCO1B1 variant c.521TT (2.8 ± 0.9 fmol/µg) or c.521TC/CC (2.5 ± 0.7 fmol/µg).
3.4 Short- and Long-Term Changes in Rosuvastatin Pharmacokinetics Following RYGB and Strict Diet
A total of 57 patients (RYGB = 29, diet = 28) participated in all four pharmacokinetic investigations. Mean predicted pharmacokinetic profiles of rosuvastatin are shown in supplementary Figure S6, and an overview of pharmacokinetic parameters for all groups across time is provided in Table 2. There were no differences in pharmacokinetic parameters of rosuvastatin between the two intervention groups at baseline (Table 3).
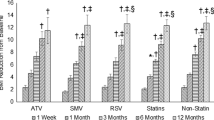
Following the initial 3-week LED, oral clearance decreased by 16% [95% CI 0, 31) and 23% [95% CI 8, 38] in the RYGB and diet groups, respectively (Table 3), and the change was not different between the groups (Fig. 3). Furthermore, no changes in Cmax or Tmax were observed (Table 3). In the RYGB and diet groups combined, the change in oral clearance was positively associated with the weight loss (r = 0.25 [95% CI 0.03, 0.45]) in the same period, but not associated with change in liver fat (r = 0.05 [95% CI − 0.18, 0.27]).
Between-group differences in within-group change for the Roux-en-Y gastric bypass (RYGB) and diet groups for a oral clearance (CL/F), b maximum concentration (Cmax) and c time to maximum concentration (Tmax). Difference between groups are made with the RYGB group as reference (positive values indicate greater change in the RYGB group), and are presented as marginal mean with 95% confidence interval
In the RYGB group, a more rapid rosuvastatin absorption, reflected by a 0.9 [95% CI 0.4, 1.7] hour reduction in Tmax was observed at Week 9, compared with baseline (Table 3). There were no additional changes in oral clearance or Cmax in either the RYGB or diet groups from Week 3 to Week 9. Still, the within group change in oral clearance during this time period was different between the two groups (Fig. 3).
At Year 2, the RYGB group demonstrated a total increase in oral clearance of 21% [95% CI 1, 41] and 57% [95% CI 31, 83] compared to baseline and Week 9, respectively. The change in oral clearance from Week 9 to Year 2 was 8-fold greater in the RYGB- compared with the diet group (Fig. 3). At Year 2, oral clearance of rosuvastatin was 22% (95% CI 0, 43) higher in the RYGB group than in the diet group (Table 3). Long-term change in oral clearance from baseline to Year 2 was not associated with change in hsCRP (RYGB: r = 0.13 [95% CI − 0.24, 0.46]; diet: r = − 0.13 [95% CI − 0.46, 0.25]) or estimated liver fat (RYGB: r = 0.16 [95% CI − 0.21, 0.48]; diet: r = 0.28 [95% CI − 0.09, 0.57]) in either group. The absorption was still faster at Year 2 in the RYGB group; Tmax was reduced by 1.1 [95% CI 0.4, 1.9] hour(s) compared with baseline (Table 3), and was 0.8 [95% CI 0.2, 1.4] hour(s) shorter in the RYGB group compared with the diet group. At Year 2, Cmax in the RYGB group was 27% [95% CI 3, 51] lower compared with Week 9, but not different from Cmax at baseline or when compared with the diet group at Year 2. The diet group showed no difference from baseline in rosuvastatin pharmacokinetics at Year 2.
Neither short- nor long-term change in oral clearance was different in patients with the reduced-function variant (c.521TC or c.521CC) of SLCO1B1 from those with the homozygote wild-type variant (c.521TT) in either group (Fig. 4). While a statistically significant difference in change in oral clearance between individuals with the c.521TT and c.521TT/CC variants were found in the diet group only during LED, no differences were found in the combined RYGB and diet groups in the same time period.
Longitudinal overview of linear mixed effects model predicted oral clearance for individuals expressing the reduced function variant SLCO1B1 c.521CC and TC compared with c.521TT in the a Roux-en-Y gastric bypass (RYGB) and b diet groups, respectively. Data are presented as marginal mean with 95% confidence interval. The between-variant difference in within-variant change for the individuals with SLCO1B1 c.521TT or TC genotype compared with c.521TT are shown for the c RYGB and d diet group, presented as marginal mean with 95% confidence interval, with c.521TT as the reference group (positive values indicate greater change in patients with c.521TT)
4 Discussion
To the best of our knowledge, this is the first longitudinal, prospective pharmacokinetic study in patients with severe obesity, evaluating the effect of RYGB and strict diet on the activity of the hepatic uptake transporter OATP1B1, using rosuvastatin as a probe drug. The main finding was that neither body weight nor weight loss, induced by either RYGB or strict diet, seemed to substantially influence the activity of the hepatic uptake transporter OATP1B1. There were no systematic differences in short- or long-term change in oral clearance between patients with the reduced function variant of SLCO1B1 or wildtype, providing the main evidence for unchanged OATP1B1 activity following RYGB and weight loss observed in the present study. Also, no statistically significant differences in rosuvastatin pharmacokinetics were shown between patients with severe obesity and the normal-to-overweight control group at baseline, suggesting no effect of body weight per se on OATP1B1 activity or rosuvastatin pharmacokinetics. This is supported by similar findings using a semi-mechanistic proteomics-informed model in a subset of the same patients [27].
Given that the changes in rosuvastatin oral clearance were also present in patients with genetically decreased OATP1B1 transport ability, it seems plausible that physiological alterations associated with caloric restriction and/or RYGB induced the observed alterations in oral clearance in the present study. Following the 3-week LED with similar weight loss, oral clearance decreased by approximately 20% in both intervention groups. It is known that caloric restriction may affect both liver size and composition. In a systematic review of LEDs (800–1200 kcal/day) prior to bariatric surgery, liver size was found to be reduced by 12–27%, and approximately 80% of total reduction in liver size was described to occur in the initial two weeks of diet [35]. As rosuvastatin displays a high hepatic extraction ratio (0.63), clearance and bioavailability may be susceptible to changes in both portal and hepatic blood flow [14]. It is possible that hepatic blood flow could be altered following rapid reduction in liver size, as hepatic blood flow has been found to increase following bariatric surgery [36, 37]. A transient increase in portal vein blood flow could thus lead to an increased bioavailability of rosuvastatin, possibly explaining the reduced oral clearance following the initial LED. However, this hypothesis will require further investigation into hepatic haemodynamics following diet-induced weight loss. During the initial LED, change in oral clearance was not associated with change in predicted liver fat content, suggesting that liver composition may be less important with regard to rosuvastatin disposition. Additionally, oral clearance of rosuvastatin was not different in patients with NAFLD-score above the diagnostic cut-off value compared with those with normal scores. This agrees with findings from Tirona and colleagues, who reported no differences in rosuvastatin pharmacokinetics in patients with obesity with magnetic resonance imaging (MRI)-confirmed NAFLD compared to a control group [38]. Furthermore, RYGB or 6 weeks of additional VLED did not induce additional changes in oral clearance despite further reduction in body weight, which indicates that weight loss is not the sole explanation for the observed effects. Nonetheless, a statistically significant between-group difference in the change in oral clearance following RYGB or six weeks of additional VLED was found. However, considering that no significant changes within either group were observed in this period, the observed between-group difference was considered to be less important in the overall interpretation of the results.
At Year 2, no changes in rosuvastatin pharmacokinetics from baseline were observed in the diet group, while the RYGB group demonstrated a net increase in oral clearance of approximately 21%. This increase in oral clearance long term seems to be a surgery-specific effect on rosuvastatin absorption, leading to a net reduced bioavailability that may not have been readily apparent or sufficiently developed six weeks post-surgery. Given the anatomical and physiological changes in the gastrointestinal tract following RYGB, and the fact that rosuvastatin is moderately absorbed (~ 50%) [39] and displays a complex, dissolution rate-limited absorption (BCS class II), a reduction in the absorption and thus oral bioavailability after surgery is not unexpected. Surprisingly, this effect was not observed shortly after surgery. Moreover, it cannot be ruled out that other surgery-specific effects, such as alteration in incretins, expression/activity of other drug transporters such as NTCP or gut microbiota, may have contributed to the observed change in oral clearance in the long term. To date, only one study has evaluated the effect of RYGB on rosuvastatin pharmacokinetics. However, with only one dose- and weight-normalised blood sample, the data were not sufficient to draw conclusions regarding the effect of RYGB on the pharmacokinetics of rosuvastatin [40].
At the time of surgery, hepatic expression of OATP1B1 was positively associated with oral clearance in the RYGB group, but no such associations were shown in the control group, despite similar mean hepatic expression of OATP1B1 in the two groups. In contrast to the controls, the RYGB group was subjected to an initial LED, and thus a subsequent weight loss prior to surgery in the present study. This may potentially explain some of these differences, as rosuvastatin oral clearance was already reduced in the RYGB group when biopsies for protein expression measurement were obtained.
A strength of the present study was that oral clearance of rosuvastatin was calculated using a precise measurement of AUC0–∞, obtained from extensive blood-sampling in combination with an internally validated population pharmacokinetic model. Additionally, by including a dietary control group with matched short-term weight loss, we were able to differentiate the effects of surgery and weight loss on rosuvastatin pharmacokinetics. However, it is also important to recognise the limitations of the presented work. Most importantly, without concomitant intravenous administration it is not possible to determine absolute bioavailability of rosuvastatin, which is likely to change following RYGB. As such, true clearance could provide additional mechanistic understanding of the underlying processes. Another weakness was that NAFLD was not confirmed with biopsy or MRI, but predicted based on metabolic factors. It is also important to recognise that rosuvastatin has a reported half-life of 20 h [14], but sampling was only performed up to 24 h. As such, population pharmacokinetic modelling was used for parameter estimation over non-compartmental methods, as the former is not as reliant on rich sampling in the elimination phase. While additional samples may have improved the accuracy of parameter estimation, we could not justify the added patient inconvenience and logistical challenges for this probe drug.
5 Conclusions
In conclusion, neither body weight, weight loss, nor RYGB per se seem to affect OATP1B1 activity. This is primarily substantiated by the fact that individuals with the reduced function variant of SLCO1B1 showed similar change in oral clearance of rosuvastatin over time. The short-term decrease in oral clearance following LED is reversible, as indicated by the return to baseline values following regained weight in the diet group while the long-term increase in oral clearance observed in the RYGB group appears to be due to a surgery-specific alteration in rosuvastatin disposition leading to an increased oral clearance. Overall, the observed changes in rosuvastatin pharmacokinetics in the present study were small, and dose adjustments of rosuvastatin following RYGB- or diet-induced weight loss appears to be unnecessary.
References
Collaboration NCDRF. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387(10026):1377–96.
Haslam DW, James WP. Obesity. Lancet. 2005;366(9492):1197–209.
Abdelaal M, le Roux CW, Docherty NG. Morbidity and mortality associated with obesity. Ann Transl Med. 2017;5(7):161.
Garvey WT, Mechanick JI, Brett EM, Garber AJ, Hurley DL, Jastreboff AM, et al. American Association of Clinical Endocrinologists and American College of Endocrinology Comprehensive Clinical Practice Guidelines Formedical Care of Patients with Obesity. Endocr Pract. 2016;22:1–203.
Colquitt JL, Pickett K, Loveman E, Frampton GK. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014;8:003641.
Cosentino C, Marchetti C, Monami M, Mannucci E, Cresci B. Efficacy and effects of bariatric surgery in the treatment of obesity: network meta-analysis of randomised controlled trials. Nutr Metab Cardiovasc Dis. 2021;31(10):2815–24.
Padwal R, Klarenbach S, Wiebe N, Hazel M, Birch D, Karmali S, et al. Bariatric surgery: a systematic review of the clinical and economic evidence. J Gen Intern Med. 2011;26(10):1183–94.
Salte OBK, Svanevik M, Risstad H, Hofso D, Blom-Hogestol IK, Johnson LK, et al. Standard versus distal Roux-en-Y gastric bypass in patients with BMI 50-60 kg/m2: 5-year outcomes of a double-blind, randomized clinical trial. BJS Open. 2021;5(6).
Padwal R, Brocks D, Sharma AM. A systematic review of drug absorption following bariatric surgery and its theoretical implications. Obes Rev. 2010;11(1):41–50.
Chapman MJ, McTaggart F. Optimizing the pharmacology of statins: characteristics of rosuvastatin. Atheroscler Suppl. 2002;2(4):33–6 (discussion 6-7).
McFeely SJ, Ritchie TK, Yu J, Nordmark A, Levy RH, Ragueneau-Majlessi I. Identification and evaluation of clinical substrates of organic anion transporting polypeptides 1B1 and 1B3. Clin Transl Sci. 2019;12(4):379–87.
Zhang D, Ding Y, Wang X, Xin W, Du W, Chen W, et al. Effects of ABCG2 and SLCO1B1 gene variants on inflammation markers in patients with hypercholesterolemia and diabetes mellitus treated with rosuvastatin. Eur J Clin Pharmacol. 2020;76(7):939–46.
Shitara Y, Maeda K, Ikejiri K, Yoshida K, Horie T, Sugiyama Y. Clinical significance of organic anion transporting polypeptides (OATPs) in drug disposition: their roles in hepatic clearance and intestinal absorption. Biopharm Drug Dispos. 2013;34(1):45–78.
Martin PD, Warwick MJ, Dane AL, Hill SJ, Giles PB, Phillips PJ, et al. Metabolism, excretion, and pharmacokinetics of rosuvastatin in healthy adult male volunteers. Clin Ther. 2003;25(11):2822–35.
Bergman E, Forsell P, Tevell A, Persson EM, Hedeland M, Bondesson U, et al. Biliary secretion of rosuvastatin and bile acids in humans during the absorption phase. Eur J Pharm Sci. 2006;29(3–4):205–14.
Niemi M, Pasanen MK, Neuvonen PJ. Organic anion transporting polypeptide 1B1: a genetically polymorphic transporter of major importance for hepatic drug uptake. Pharmacol Rev. 2011;63(1):157–81.
Hirota T, Fujita Y, Ieiri I. An updated review of pharmacokinetic drug interactions and pharmacogenetics of statins. Expert Opin Drug Metab Toxicol. 2020;16(9):809–22.
Krogstad V, Peric A, Robertsen I, Kringen MK, Vistnes M, Hjelmesaeth J, et al. Correlation of body weight and composition with hepatic activities of cytochrome P450 enzymes. J Pharm Sci. 2021;110(1):432–7.
Ulvestad M, Skottheim IB, Jakobsen GS, Bremer S, Molden E, Asberg A, et al. Impact of OATP1B1, MDR1, and CYP3A4 expression in liver and intestine on interpatient pharmacokinetic variability of atorvastatin in obese subjects. Clin Pharmacol Ther. 2013;93(3):275–82.
Kvitne KE, Robertsen I, Skovlund E, Christensen H, Krogstad V, Wegler C, et al. Short- and long-term effects of body weight loss following calorie restriction and gastric bypass on CYP3A-activity—a non-randomized three-armed controlled trial. Clin Transl Sci. 2022;15(1):221–33.
Jamwal R, Barlock BJ. Nonalcoholic fatty liver disease (NAFLD) and hepatic cytochrome P450 (CYP) enzymes. Pharmaceuticals (Basel). 2020;13(9):222.
Hjelmesaeth J, Asberg A, Andersson S, Sandbu R, Robertsen I, Johnson LK, et al. Impact of body weight, low energy diet and gastric bypass on drug bioavailability, cardiovascular risk factors and metabolic biomarkers: protocol for an open, non-randomised, three-armed single centre study (COCKTAIL). BMJ Open. 2018;8(5): e021878.
Krogstad V, Peric A, Robertsen I, Kringen MK, Wegler C, Angeles PC, et al. A comparative analysis of cytochrome P450 activities in paired liver and small intestinal samples from patients with obesity. Drug Metab Dispos. 2020;48(1):8–17.
Braamskamp M, Langslet G, McCrindle BW, Cassiman D, Francis GA, Gagne C, et al. Efficacy and safety of rosuvastatin therapy in children and adolescents with familial hypercholesterolemia: results from the CHARON study. J Clin Lipidol. 2015;9(6):741–50.
Machiela MJ, Chanock SJ. LDlink: a web-based application for exploring population-specific haplotype structure and linking correlated alleles of possible functional variants. Bioinformatics. 2015;31(21):3555–7.
Wegler C, Olander M, Wisniewski JR, Lundquist P, Zettl K, Asberg A, et al. Global variability analysis of mRNA and protein concentrations across and within human tissues. NAR Genom Bioinform. 2020;2(1):lqz010.
Wegler C, Prieto Garcia L, Klinting S, Robertsen I, Wisniewski JR, Hjelmesaeth J, et al. Proteomics-informed prediction of rosuvastatin plasma profiles in patients with a wide range of body weight. Clin Pharmacol Ther. 2021;109(3):762–71.
Wisniewski JR, Mann M. Consecutive proteolytic digestion in an enzyme reactor increases depth of proteomic and phosphoproteomic analysis. Anal Chem. 2012;84(6):2631–7.
Tyanova S, Temu T, Cox J. The MaxQuant computational platform for mass spectrometry-based shotgun proteomics. Nat Protoc. 2016;11(12):2301–19.
Huber W, von Heydebreck A, Sultmann H, Poustka A, Vingron M. Variance stabilization applied to microarray data calibration and to the quantification of differential expression. Bioinformatics. 2002;18(suppl_1):S96-104.
Wisniewski JR, Rakus D. Multi-enzyme digestion FASP and the 'Total Protein Approach’-based absolute quantification of the Escherichia coli proteome. J Proteom. 2014;109:322–31.
Neely MN, van Guilder MG, Yamada WM, Schumitzky A, Jelliffe RW. Accurate detection of outliers and subpopulations with Pmetrics, a nonparametric and parametric pharmacometric modeling and simulation package for R. Ther Drug Monit. 2012;34(4):467–76.
Kotronen A, Peltonen M, Hakkarainen A, Sevastianova K, Bergholm R, Johansson LM, et al. Prediction of non-alcoholic fatty liver disease and liver fat using metabolic and genetic factors. Gastroenterology. 2009;137(3):865–72.
R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. 2020.
Romeijn MM, Kolen AM, Holthuijsen DDB, Janssen L, Schep G, Leclercq WKG, et al. Effectiveness of a Low-calorie diet for liver volume reduction prior to bariatric surgery: a systematic review. Obes Surg. 2021;31(1):350–6.
Immonen H, Hannukainen JC, Kudomi N, Pihlajamaki J, Saunavaara V, Laine J, et al. Increased liver fatty acid uptake is partly reversed and liver fat content normalized after bariatric surgery. Diabetes Care. 2018;41(2):368–71.
Honka H, Koffert J, Kauhanen S, Kudomi N, Hurme S, Mari A, et al. Liver blood dynamics after bariatric surgery: the effects of mixed-meal test and incretin infusions. Endocr Connect. 2018;7(7):888–96.
Tirona RG, Kassam Z, Strapp R, Ramu M, Zhu C, Liu M, et al. Apixaban and Rosuvas–tatin pharmacokinetics in nonalcoholic fatty liver disease. Drug Metab Dispos. 2018;46(5):485–92.
Martin PD, Warwick MJ, Dane AL, Brindley C, Short T. Absolute oral bioavailability of rosuvastatin in healthy white adult male volunteers. Clin Ther. 2003;25(10):2553–63.
El-Zailik A, Cheung LK, Wang Y, Sherman V, Chow DS. Longitudinal impacts of gastric bypass surgery on pharmacodynamics and pharmacokinetics of statins. Obes Surg. 2019;29(8):2571–83.
Acknowledgements
The authors would like to express their gratitude to the participants, the surgical staff, and the study personnel working on the COCKTAIL study at Vestfold Hospital Trust. The authors also thank the Swedish Research Council, approval numbers 5715 and 01951, for supporting the proteomics analyses. The computations were performed on resources provided by UNINETT Sigma2—the National Infrastructure for High Performance Computing and Data Storage in Norway, under project NN9736K.
Funding
Open access funding provided by University of Oslo (incl Oslo University Hospital).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Vestfold Hospital Trust, Norway; Department of Pharmacy, University of Oslo, Norway; and AstraZeneca, Sweden.
Conflict of interest
C. Karlsson, S. Andersson and R. Jansson-Löfmark are employees of and own shares in AstraZeneca. C. Wegler is a former employee of AstraZeneca. All other authors have no competing interests to declare. Markus Hovd, Ida Robertsen, Line Kristin Johnson, Veronica Krogstad, Kine E. Kvitne, Marianne K. Kringen, Eva Skovlund, Per Artursson, Rune Sandbu, Jøran Hjelmesæth, Anders Åsberg, Rasmus JL. and Hege Christensen declare that they have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Author contributions
J.H., A.Å., H.C., E.S., C.K., S.A and R.S. designed the study. I.R., V.K., L.K.J., M.K.K., P.A., and C.W. performed the research. M.H., I.R., K.E.K., and E.S. analyzed the data. M.H., I.R., A.Å. and H.C. wrote the manuscript. All authors contributed to critically reviewing the manuscript and gave their final approval for submission.
Data availability statement
Access to data collected from this study, including anonymised individual participant data, may potentially be made available following publication on e-mail request to the corresponding author. After approval of a proposal, data will be shared with investigators whose proposed use of the data has been approved by the COCKTAIL steering committee, according to the consent given by the participants and Norwegian laws and legislations.
Ethics approval
The study was approved by the Regional Committee for Medical and Health Research Ethics (2013/2379/REK).
Consent to participate
Written informed consent was obtained from all patients prior to any study-specific procedures.
Consent for publication
Not applicable.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hovd, M., Robertsen, I., Johnson, L.K. et al. Neither Gastric Bypass Surgery Nor Diet-Induced Weight-Loss Affect OATP1B1 Activity as Measured by Rosuvastatin Oral Clearance. Clin Pharmacokinet 62, 725–735 (2023). https://doi.org/10.1007/s40262-023-01235-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-023-01235-5