Abstract
Background and Objective
Ultra rapid lispro (URLi) is a novel insulin lispro formulation developed to more closely match physiological insulin secretion and improve postprandial glucose control. This pooled analysis compared the pharmacokinetics and glucodynamics between URLi and Humalog® in healthy subjects and patients with type 1 or type 2 diabetes mellitus.
Methods
The analysis included four randomized, double-blind, crossover, single-dose studies (healthy subjects [n = 74], patients with type 1 diabetes [n = 78], and type 2 diabetes [n = 38]) evaluating subcutaneous doses of 7, 15, or 30 U of URLi and Humalog during an 8- to 10-h euglycemic clamp procedure.
Results
The pooled analysis showed an ~ 5-min faster onset of appearance, an ~8-fold greater exposure in the first 15 min, a 43% reduction in exposure beyond 3 h, and a 68-min shorter exposure duration with URLi vs Humalog across all study populations and dose range. Compared with Humalog, URLi had a 10-min faster onset of action, a 3-fold greater insulin action in the first 30 min, a 35% reduction in insulin action beyond 4 h, and a 44-min shorter duration of action across all populations and dose range. Overall exposure and insulin action were similar between URLi and Humalog for each dose level and study population.
Conclusions
Across the studied populations and dose range, URLi consistently demonstrated a faster absorption, reduced late exposure, and overall shorter exposure duration compared with Humalog. Similarly, URLi demonstrated earlier insulin action while reducing late insulin action and shorter insulin action compared with Humalog across the study populations and dose range.
Clinical Trial Registration
NCT02942654 (registered: 21 October, 2016), NCT03286751 (registered: 15 September, 2017), NCT03166124 (registered: 23 May, 2017), and NCT03305822 (registered: 5 October, 2017).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Across the studied populations and dose range, insulin appeared in the blood five times faster, and early insulin exposure increased up to eight-fold, resulting in a greater early glucose-lowering effect with ultra rapid lispro compared with Humalog® |
Insulin also left the blood sooner, reducing the late glucose-lowering effect with ultra rapid lispro compared with Humalog; potentially reducing the occurrence of late hypoglycemia observed with a rapid-acting insulin analogs |
The ultra-rapid pharmacokinetic and glucodynamic profile of ultra rapid lispro has the potential to improve post-meal glucose control over current rapid-acting insulin analogs |
1 Introduction
In patients with diabetes, glycemic variability may contribute to increased morbidity and mortality, as well as reduced quality of life [1,2,3]. Control of postprandial glucose (PPG) remains a challenge in patients with type 1 diabetes (T1D) or type 2 diabetes (T2D) because of absent or reduced physiological secretion of prandial insulin or insulin resistance [4]. Therefore, optimum PPG control is crucial for achieving recommended glycated hemoglobin targets and preventing or delaying long-term complications [5,6,7]. Intensive insulin therapy in patients with T1D and T2D with basal and bolus (prandial) insulin aims to mimic physiological insulin secretion to control basal and prandial blood glucose [8,9,10]. Rapid-acting insulin analogs (e.g., insulin lispro, insulin aspart, and insulin glulisine) have a faster onset and a shorter duration of action than regular human insulin [11]. Although rapid-acting insulins have shown superiority over regular insulin at reducing postprandial glycemic excursions [12], they cannot always match carbohydrate absorption profiles [13, 14], limiting their efficacy in PPG control. Thus, there is a need to develop faster, ultra-rapid-acting insulins that more closely match the endogenous response to food intake and minimize PPG excursions.
Insulin lispro (Humalog®) is a commercially available, rapid-acting human insulin analog indicated for glycemic control in adults and children with diabetes mellitus [15]. Ultra rapid lispro (URLi) is a novel insulin lispro formulation containing two locally acting excipients, treprostinil to induce local vasodilation [16] and citrate to increase vascular permeability [17], thereby accelerating insulin lispro absoprtion at the injection site. URLi was formulated to more closely match physiological prandial insulin secretion and improve PPG control. In a recent publication comparing the pharmacokinetics and glucodynamics of URLi with Humalog, Fiasp®, and NovoRapid®, URLi showed greater numeric glucose lowering during a mixed meal tolerance test in patients with T1D and more closely matched the early glucose lowering of endogenous insulin secretion in healthy subjects [18]. Phase III clinical studies of URLi have demonstrated superiority of URLi to Humalog in controlling PPG excursions, with a similar overall safety profile in patients with T1D [19] and T2D [20].
Several factors, including insulin dose, insulin formulation, and patient physiology, can impact the pharmacokinetic (PK) and glucodynamic (GD) profiles. Therefore, this pooled analysis was conducted to compare and assess the consistency of pharmacokinetics and glucodynamics between URLi and Humalog in healthy subjects and patients with T1D or T2D.
2 Methods
2.1 Study Selection
Study inclusion criteria were: completed phase I studies with a crossover design, conducted in adults who received the final commercial formulation of URLi, used Humalog as the comparator, and had similar time points for the data collection during a euglycemic clamp procedure.
2.2 Study Design
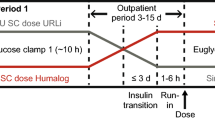
The pooled analysis included four randomized, double-blind, crossover, single-dose studies that evaluated insulin lispro PK and GD responses of URLi compared with Humalog following administration of a 7-U, 15-U, or 30-U dose. The pharmacokinetics and glucodynamics were assessed up to 8–10 h. Two trials in healthy subjects (trials 1 and 2 [21]), one trial in patients with T1D (trial 3 [22]), and one trial in patients with T2D (trial 4 [23]) met the inclusion criteria. Information on trial design, population characteristics, sample size, and treatment arms is presented in Table 1. Two trials were conducted at a single center (Profil, Nuess, Germany), one trial (trial 3 [patients with T1D]) was conducted at two centers (Profil, Nuess, Germany and Profil, Mainz, Germany), and one trial (trial 1 [healthy subjects]) was conducted in Singapore (Lilly Centre for Clinical Pharmacology Pte Ltd, Singapore). All trials were conducted in accordance with the principles of the Declaration of Helsinki (2000), International Council for Harmonisation, and the E6 Guideline for Good Clinical Practice. Institutional review board approval and written informed consent from all subjects were obtained before conducting any evaluations or study procedures. The trials were registered at ClinicalTrials.gov (identifiers: NCT02942654, NCT03286751, NCT03166124, and NCT03305822).
2.3 Study Procedures and Treatments
Participants of trials 1, 3, and 4 were randomized to single subcutaneous 15-U doses of URLi and Humalog U100 formulations (Eli Lilly, Indianapolis, IN, USA). Trial 2 healthy subjects were randomized to single subcutaneous doses of 7, 15, and 30 U of URLi and Humalog. Both Humalog and URLi were administered to the abdominal wall using a 6-mm or 8-mm, 31-gauge needle to ensure that injections were delivered to a consistent depth. For patients with T1D and T2D on multiple daily insulin injections, the washout period prior to each dosing visit was ≥ 72 h for insulin glargine U300, ≥ 48 h for insulin detemir or glargine, and ≥ 24 h for neutral protamine Hagedorn insulin, insulin mixtures, or other intermediate-acting insulin. Patients receiving continuous subcutaneous insulin infusion therapy were switched to insulin glulisine (Apidra®; Sanofi, Paris, France) ≥ 8 h before dosing and discontinued basal insulin delivery ≥ 3 h before dosing. For patients with T2D receiving oral antidiabetic medications, patients discontinued dipeptidyl peptidase-IV inhibitors, sulfonylureas, and sodium glucose co-transporter 2 inhibitors 2 weeks prior to the first dosing. Additionally, studies conducted in patients with T1D and T2D required that any bolus injection of short-acting insulin should occur at least 6 h prior to study drug dosing. However, patients were allowed to continue metformin throughout the study.
2.4 Bioanalysis
Serum-free insulin lispro was analyzed using a validated enzyme-linked immunosorbent assay specific to insulin lispro without cross-reactivity to endogenous insulin or insulin glulisine (600 pmol/L) at Charles River Laboratories Montreal in Senneville, QC, Canada. Blood samples for the PK analysis were collected at time 0; every 5 min for the first 60 min; at 70, 90, 120, 150, and 180 min; and hourly thereafter up to 8 h post-administration in trial 1 and up to 10 h post-administration for all other studies. The lower limit of quantification (LLOQ) was 8.6 pmol/L. The inter-assay accuracy (percent relative error) and inter-assay precision (percent relative standard deviation) during validation were ≤ 16%.
2.5 Glucodynamics
Glucodynamic assessments were determined from a euglycemic glucose clamp procedure using the automated ClampArt® device in trials 2, 3, and 4, and a manual clamp in trial 1. During the euglycemic clamp procedure, target blood glucose levels were kept constant while glucose infusion rate (GIR) varied over time, reflecting the GD activity of exogenous insulin. In healthy subjects, baseline fasting glucose level (calculated as the mean of blood glucose levels at 6, 4, and 2 min before study drug administration) was set as the target blood glucose level. In patients with T1D or T2D, a run-in period was conducted prior to dosing to achieve the target blood glucose level (defined as 100 mg/dL ± 10% for T1D and 100 mg/dL ± 20% for T2D) using a variable intravenous infusion of either glucose (20% dextrose solution) or insulin (insulin glulisine). The run-in was stopped at least 30 min prior to dosing in patients with T2D and at least 10 min prior to dosing in patients with T1D. With this approach, GIR reflected only the pharmacology of the study treatments by removing any confounding effect of the glucose or insulin during the run-in on the determination of the onset of insulin action or early GIR. Once the target blood glucose level stabilized, patients or subjects received either URLi or Humalog. Following drug administration, time to onset of insulin action (Tonset) was defined as when blood glucose dropped by 5 mg/dL (0.3 mmol/L) below the baseline. Following onset of action, the GIR was recorded every minute (trials 2, 3, 4) or every 2.5 min (trial 1) throughout the clamp procedure. For trials using an automated clamp, manual blood samples were collected and measured (SuperGL glucose analyzer; Dr. Müller/Hitado, Möhnesee, Germany) for blood glucose at least every 30 min during the clamp procedure to validate clamp glucose sensor measurements. For the trial, using a manual clamp, blood samples were collected at least every 5 min during the clamp procedure and were measured using glucose analyzers (YSI STAT Plus Glucose and Lactate Analyzer; YSI Inc., Yellow Springs, OH, USA).
Blood samples were collected and measured using the YSI STAT Plus Glucose and Lactate Analyzer (YSI Incorporated, Yellow Springs, OH, USA) for trial 1 and the SuperGL glucose analyser (Dr. Müller/Hitado, Möhnesee, Germany) for trials 2, 3, and 4. The euglycemic clamp procedure, where the time–concentration and time–action profiles of the study treatment were evaluated simultaneously, was conducted for up to 10 h in trials 2, 3, and 4, and up to 8 h in trial 1.
2.6 Study Endpoints
2.6.1 Pharmacokinetic Parameters
Free serum insulin lispro PK parameters were calculated by non-compartmental methods using Phoenix® Version 7.0 and S-PLUS® Version 8.2. Early insulin exposure was characterized by time to early half-maximal drug concentration (early 50% tmax), area under the concentration vs time curve (AUC) from time 0 to 15 min (AUC0–15 min), AUC from time 0 to 30 min (AUC0–30 min), AUC from time 0 to 1 h (AUC0–1h), and onset of appearance, defined as the time that serum insulin lispro reached the LLOQ. Determination of onset of appearance used a linear interpolation between the time of dosing (zero serum insulin lispro concentration) and the time of the first quantifiable serum insulin lispro concentration. Late insulin exposure was characterized by time to late half-maximal drug concentration (late 50% tmax), AUC from time 2 to X h (AUC2–Xh), and AUC from time 3 to X h (AUC3–Xh), where X is the last sample collection in the study (either 8 or 10 h post-injection), and duration of exposure, defined as the time from dosing until serum insulin lispro reached the LLOQ. Overall insulin exposure was determined by maximum observed drug concentration (Cmax), time to Cmax (tmax), and AUC from time 0 to infinity (AUC0–∞).
2.6.2 Glucodynamic Parameters
Glucodynamic analyses were conducted using Phoenix Version 6.4 or higher and S-PLUS Version 8.2. Glucodynamic assessments were determined from the glucose clamp procedure, where GIR over time was used as a measure of insulin effect. A locally weighted scatterplot smoothing function was applied to all individual GIR-vs-time profiles in each treatment group and/or dose. Fitted data for each patient were used to calculate GD parameters, except Tonset, which was based on raw GIR data. Early insulin action was characterized by Tonset, time to half-maximal GIR before maximum GIR (early 50% tRmax), total amount of glucose infused over the first 30 min (Gtot,0–30min), and total amount of glucose infused over the first hour (Gtot,0–1h). Late insulin action was characterized by time to half-maximal GIR occurring after maximum GIR (late 50% tRmax), total amount of glucose infused from 2 h to the end of the clamp (Gtot,2h–End), total amount of glucose infused from 3 h to the end of the clamp (Gtot,3h–End), total amount of glucose infused from 4 h to the end of the clamp (Gtot,4h–End), and duration of insulin action. Total insulin action was characterized by total amount of glucose infused over the duration of the clamp (Gtot) and maximum GIR (Rmax).
2.7 Statistical Analyses
The PK and GD results from the individual studies were obtained from the analysis of each individual study, and the pooled PK and GD analyses included the individual subject data from these four studies. The PK and GD parameters were compared between URLi and Humalog using a mixed-effects model, with treatment and study as fixed effects and subject as a random effect. For log-transformed parameters, least-squares (LS) geometric means, ratios of LS geometric means between URLi and Humalog, and their corresponding 95% confidence intervals (CIs) were estimated using the mixed-effects model. For parameters analyzed using original scale data (time parameters and GD parameters with values of 0), LS means, differences in LS means between URLi and Humalog, and 95% CIs for each dose level were estimated from the mixed-effects models. For GD parameters with values of 0, treatment ratios and 95% CIs were calculated using Fieller’s method. Forest plots were created that included the individual study level and pooled analysis difference or ratio between URLi and Humalog, and the 95% CIs for the PK and GD parameters. Statistical analyses were conducted using SAS® Version 9.4 (SAS Institute, Cary, NC, USA) at a 5% significance level.
3 Results
3.1 Trial and Patient Characteristics
Of the four trials, two were conducted in healthy subjects, one in patients with T1D (both younger adults and elderly patients), and one in patients with T2D (Table 1). A total of 191 subjects were included in the PK and GD analyses. The sample size in the trials ranged from 32 to 80 adult participants. A total of 74 healthy subjects, 78 patients with T1D, and 38 patients with T2D were included in the pooled analysis (Table 1). The average age in the study populations ranged from 32.0 to 68.5 years. The average duration of diabetes was approximately 18 years in younger adult patients with T1D, approximately 38 years in elderly patients with T1D, and approximately 17 years in patients with T2D (Table 1).
3.2 Pharmacokinetic Endpoints
3.2.1 Insulin Lispro Concentration Profiles
Mean serum insulin lispro concentration–time profiles were shifted to the left following dosing with URLi compared with Humalog in healthy subjects (Fig. 1a), patients with T1D (Fig. 1b), and patients with T2D (Fig. 1c), demonstrating accelerated insulin lispro absorption, reduced late exposure, and overall shorter exposure duration with URLi vs Humalog consistently in all populations.
Mean (± standard error) serum insulin lispro concentration–time profile (top panels) and mean glucose infusion rates vs time profiles (bottom panels) for ultra rapid lispro (URLi) and Humalog in healthy subjects (left panels), patients with type 1 diabetes (younger adults; middle panels), and patients with type 2 diabetes (right panels). Data from [21,22,23]. U units
3.2.2 Early Insulin Exposure
Insulin absorption was consistently faster with URLi compared with Humalog for all study populations and dose levels (Fig. 2). The onset of appearance of insulin lispro with URLi was 3.5–5.6 min faster compared with Humalog across the individual studies and was 4.8 min faster in the pooled analysis. Early 50% tmax was 10.9–19.9 min earlier across the individual studies and was 14.0 min earlier in the pooled analysis following URLi compared with Humalog. This accelerated absorption increased the early serum insulin lispro exposure across all populations and the dose range. The largest increase was observed in the first 15 min after injection. The exposure in the first 15 min was increased by 6.1–12.3-fold in the individual studies and was increased by 7.5-fold in the pooled analysis with URLi compared with Humalog. Significant increases in exposure were also demonstrated at 30 min and 1 h after injection. The exposure in the first 30 min was increased with URLi by 2.3–4.6-fold in the individual studies and 3.0-fold in the pooled analysis compared with Humalog. Similarly, the exposure in the first hour was increased with URLi by 1.4–2.0-fold in the individual studies and 1.5-fold in the pooled analysis compared with Humalog.
Forest plots of the difference and ratio of geometric least-squares means and 95% confidence interval (CI) between ultra rapid lispro (URLi) and Humalog for early insulin lispro pharmacokinetic parameters in adults in individual studies and in the pooled analysis. AUC area under the concentration–time curve, AUC0–15min AUC from 0 to 15 min, AUC0–30min AUC from 0 to 30 min, AUC0–1h AUC from 0 to 1 h, early 50% tmax time to early half-maximal drug concentration, T1D type 1 diabetes, T2D type 2 diabetes, U units
3.2.3 Late Insulin Exposure
Late insulin exposure was reduced with URLi compared with Humalog for all study populations and the dose range studied (Fig. 3). A statistically significant reduction was consistently shown in the insulin lispro exposure after 3 h with URLi compared with Humalog. There was a 26–52% reduction (ratio of 0.74–0.48) across the individual studies with a 43% reduction based on the pooled analysis. The late 50% tmax was reduced by 17.6 min with URLi compared with Humalog in the pooled analysis. Although a reduction in timing of the late 50% tmax was observed with URLi compared with Humalog within all studies, not all differences achieved a statistical significance. The duration of exposure was significantly reduced with URLi compared with Humalog across all studies, except in one trial in healthy subjects (trial 1), which had a shorter PK collection period. The duration of exposure was 5.9–86.3 min shorter across the individual studies and 68.2 mins shorter in the pooled analysis with URLi compared with Humalog.
Forest plots of the difference and ratio of geometric least-squares means and 95% confidence interval (CI) between ultra rapid lispro (URLi) and Humalog for late insulin lispro pharmacokinetic parameters in adults in individual studies and in the pooled analysis. AUC area under the concentration–time curve, AUC2–Xh AUC from 2 to X h, AUC3–Xh AUC from 3 to X h, late 50% tmax time to late half-maximal drug concentration, T1D type 1 diabetes, T2D type 2 diabetes, U units, X 8 h for trial 1 and 10 h for all other trials
3.2.4 Overall Insulin Exposure
The overall insulin exposure (AUC0–∞) and tmax were comparable between URLi and Humalog in the individual studies and in the pooled analysis (Fig. 4). However, the accelerated insulin lispro absorption and shorter exposure duration following URLi administration resulted in a higher Cmax compared with Humalog, which was 14% higher in the pooled analysis.
Forest plots of the difference and ratio of geometric least-squares means and 95% confidence interval (CI) between ultra rapid lispro (URLi) and Humalog for overall insulin lispro pharmacokinetic parameters in adults in individual studies and in the pooled analysis. AUC area under the concentration–time curve, AUC0–∞ AUC from time 0 to infinity, Cmax maximum observed drug concentration, T1D type 1 diabetes, T2D type 2 diabetes, tmax time to maximum observed drug concentration, U units
3.3 Glucodynamic Endpoints
3.3.1 Glucose Infusion Profiles
Mean GIR profiles with URLi were left-shifted compared with Humalog in healthy subjects (Fig. 1d), patients with T1D (Fig. 1e), and patients with T2D (Fig. 1f), indicating a faster onset of insulin action, reduced late insulin action, and shorter duration of insulin action with URLi vs Humalog consistently across populations and the studied dose range.
3.3.2 Early Insulin Action
A consistently faster insulin action with URLi compared with Humalog was observed in all study populations and studied dose range (Fig. 5). The onset of action was 6.3–13.9 min faster across the individual studies and 10.3 min faster in the pooled analysis with URLi compared with Humalog. The faster insulin action resulted in an increased amount of glucose infused in the early part of the euglycemic clamp procedure. The largest increase was observed in the first 30 min after injection, which was increased by 2.4-fold and 6.1-fold in the individual studies and 3.1-fold in the pooled analysis with URLi compared with Humalog. Similarly, the insulin action in the first hour was increased 1.6-fold and 2.2-fold in the individual studies and 1.7 in the pooled analysis with URLi compared with Humalog. The early 50% tRmax occurred earlier with URLi compared with Humalog across all studies; however, the change was not significant in trial 4. From the pooled analysis, the early 50% tRmax was 12.3 min earlier with URLi compared with Humalog.
Forest plots of the difference and ratio of geometric least-squares means and 95% confidence interval (CI) between ultra rapid lispro (URLi) and Humalog for early insulin action in adults in individual studies and in the pooled analysis. Note: For glucodynamic parameters with at least one patient with a value of 0, treatment ratios of least-squares means and their 95% CIs were estimated using Fieller’s method. early 50% tRmax time to half-maximal glucose infusion rate before maximum glucose infusion rate, Gtot total amount of glucose infused over the duration of the clamp procedure, Gtot,0–30min total amount of glucose infused over 30 min, Gtot,0–1h total amount of glucose infused over 1 h, T1D type 1 diabetes, T2D type 2 diabetes, Tonset time to onset of insulin action, U units
3.3.3 Late Insulin Action
Late insulin action was reduced with URLi compared with Humalog for all study populations and dose levels (Fig. 6). The most consistent and significant reduction was shown in the
Forest plots of the difference and ratio of geometric least-squares means and 95% confidence interval (CI) between ultra rapid lispro (URLi) and Humalog for late insulin action in adults in individual studies and in the pooled analysis. Note: For glucodynamic parameters with at least one patient with a value of 0, treatment ratios of least-squares means and their 95% CIs were estimated using Fieller’s method. Gtot total amount of glucose infused over the duration of the clamp procedure, Gtot,2h–End total amount of glucose infused from 2 h post-dose until the end of the clamp, Gtot,3h–End total amount of glucose infused from 3 h post-dose until the end of the clamp, Gtot,4h–End total amount of glucose infused from 4 h post-dose until the end of the clamp, late 50% tRmax time to half-maximal glucose infusion rate after maximum glucose infusion rate, T1D type 1 diabetes, T2D type 2 diabetes, U units
Gtot,4h–End, which was reduced by 35% (ratio of 0.65) with URLi compared with Humalog. The treatment ratio between URLi and Humalog for Gtot, 4 h–End ranged between 0.46 and 0.84 in the individual studies. Both the late 50% tRmax and the duration of action were reduced with URLi compared with Humalog but were not statistically significant in trial 4. Based on the pooled analysis, the duration of insulin action was 43.8 min shorter and late 50% tRmax was 37.9 min earlier with URLi vs Humalog.
3.3.4 Total Insulin Action
The overall insulin action (Gtot) was similar between URLi and Humalog, in both the individual studies and the pooled analysis (Fig. 7). The faster insulin action and shorter duration of insulin action following URLi administration resulted in a higher Rmax compared with Humalog, which was 12% higher from the pooled analysis.
Forest plots of the ratio of geometric least-squares means and 95% confidence interval (CI) between ultra rapid lispro (URLi) and Humalog for overall insulin action in adults in individual studies and in the pooled analysis. Gtot total amount of glucose infused over the duration of the clamp procedure, Rmax maximum glucose infusion rate, T1D type 1 diabetes, T2D type 2 diabetes, U units
4 Discussion
This pooled analysis from four phase I studies consistently demonstrated accelerated insulin lispro absorption with a reduction in late exposure and an overall shorter exposure duration with URLi compared with Humalog. Similarly, an earlier insulin action, reduced late insulin action, and an overall shorter duration of insulin action were demonstrated with URLi compared with Humalog. These changes were consistently demonstrated across the dose range, age groups, and study populations.
From the pooled analysis, the onset of appearance was 5 min earlier, resulting in ~8 times more exposure in the circulation during the first 15 min and 3 times more exposure in the circulation during the first 30 min with URLi compared with Humalog. URLi had 43% less exposure in the circulation after 3 h following injection, and the duration of exposure was ~ 1 h shorter with URLi compared with Humalog. Similarly, URLi had a 10-min earlier onset of insulin action, with a 13-min reduction in the time to early 50% tRmax, with URLi compared with Humalog. This faster insulin action resulted in a three-fold greater glucose lowering in the first 30 min with URLi compared with Humalog. In addition, the insulin action from 4 h to end of the clamp was reduced by 35%, the late 50% tRmax was ~40 min earlier, and the duration of action was 44 min shorter with URLi than with Humalog. Overall insulin lispro exposure and total glucose infused were similar for URLi and Humalog, which supports that no dose conversion is required when transitioning patients from Humalog to URLi.
Two main clinical challenges with exogenous prandial insulin therapies are the delayed absorption of insulin from subcutaneous tissues into systemic circulation, which may lead to postprandial hyperglycemia, and extended postprandial insulin action, which may result in late postprandial hypoglycemia [24, 25]. Across the three populations, URLi had a faster absorption and earlier insulin action while significantly reducing the late insulin action compared with Humalog, as observed in this pooled analysis, suggesting that URLi may be able to better address these challenges. This is supported by the results from the phase III studies, which showed that URLi significantly reduced PPG levels compared with Humalog when dosed immediately before a meal in patients with T1D (PRONTO-T1D) and T2D (PRONTO-T2D) treated with a bolus-basal regimen [19, 20]. These studies also demonstrated that URLi reduced the hypoglycemia rate in the period >4 h post-dose by 37% (glucose level < 54 mg/dL [3.0 mmol/L]) in patients with T1D and by 27% (glucose level ≤ 70 mg/dL [3.9 mmol/L]) in patients with T2D compared with Humalog [19, 20]. Additionally, accelerated insulin absorption profile of URLi and reduced late insulin action may allow for improved PPG control in patients who choose to dose after meals. This could be especially beneficial in patients who may have difficulty adhering to pre-meal dosing schedules. Together these results suggest that URLi offers the potential to improve glycemic control in patients with T1D and T2D.
Of particular interest in this pooled analysis was the consistency in PK and GD changes between URLi and Humalog across different clinically relevant therapeutic doses in healthy subjects, which were also consistent with the changes observed in patients with T1D and T2D. Patients with diabetes receiving insulin therapy require dose adjustments based on meal content and pre-meal glucose levels to maintain glucose control [26]. The consistency of results across a range of clinically relevant therapeutic doses [21] indicates that URLi dose adjustment would maintain the benefits of URLi compared with Humalog. Moreover, URLi showed consistent pharmacokinetics and glucodynamics between younger and elderly patients with T1D, suggesting that URLi may be used to control PPG levels in elderly patients.
The inclusion of a study containing well-controlled patients with T1D (both younger and elderly adults) with no endogenous insulin secretion allowed for accurate assessment of insulin action. In both younger and elderly adult patients with T1D, URLi significantly reduced the duration of insulin action compared with Humalog. As endogenous insulin secretion occurs in healthy subjects and can occur in patients with T2D, it is challenging to accurately estimate the true duration of insulin action during the clamp procedure as the GIR does not return to zero as observed in patients with T1D. Within both of these populations, the duration of insulin action was estimated using mean GIR response for all participants from 9 to 10 h after injection when the insulin lispro concentration for both Humalog and URLi was at or near the LLOQ [21, 22]. Notably, the duration of insulin action of URLi was not significantly reduced compared with Humalog in patients with T2D, suggesting that this correction was likely a conservative approach. In support of this, a statistically significant reduction in the duration of exposure was demonstrated with URLi compared with Humalog in patients with T2D. Using the GIR plot, URLi achieves a lower mean GIR than Humalog at 6.5 h post-dose, which was maintained for the remaining duration of the clamp procedure, suggesting a shorter duration of action is likely present if a correction for endogenous insulin action is accurately defined for this population [22].
The main strengths of this pooled analysis were: (1) individual trials had a similar study design, allowing pooling of the individual subject-level data; (2) the crossover design provided a treatment comparison within individuals; (3) washout of previous insulin therapy before treatment allowed for the characterization of only the test insulins; (4) use of an assay specific to insulin lispro to measure pharmacokinetics that prevents interference from endogenous insulin; (5) use of insulin glulisine during the run-in, which has a short half-life and does not cross-react with insulin lispro; and (6) termination of the intravenous glucose and insulin glulisine infusions at least 30 min before dosing, which avoided carryover effects on the PK and GD responses. The studies used a euglycemic clamp procedure, which is considered the gold-standard methodology for assessing insulin action. However, a limitation of this method is that it does not provide data on the effect of the insulin on PPG as it is conducted under fasting conditions. In addition, despite having some patients aged over 65 years, the pooled analysis had few patients aged > 75 years. The impact of adiposity or body mass index has not been assessed within this pooled analysis. Further investigation is required into the effects of URLi in special populations such as pediatrics.
5 Conclusions
In summary, this pooled analysis demonstrated that URLi had accelerated insulin lispro absorption with reduced late insulin exposure and shorter duration, which corresponded to a significantly earlier onset and greater early insulin action and a reduced late insulin action and shorter duration of action compared with Humalog. The overall insulin exposure and insulin action were similar between the two treatments, suggesting that no dose conversion is required when transitioning patients from Humalog to URLi. These changes were consistently demonstrated across the dose range, age groups, and study populations. These results, together with the improvement in PPG demonstrated in the phase III studies [19, 20], indicate that URLi offers the potential to improve glycemic control in patients with T1D and T2D.
References
Ceriello A. Glucose variability and diabetic complications: is it time to treat? Diabetes Care. 2020;43(6):1169–71.
Hirsch IB. Glycemic variability and diabetes complications: does it matter? Of course it does! Diabetes Care. 2015;38(8):1610–4.
Umpierrez GE, Kovatchev PB. Glycemic variability: how to measure and its clinical implication for type 2 diabetes. Am J Med Sci. 2018;356(6):518–27.
American Diabetes Association. Classification and diagnosis of diabetes: standards of medical care in diabetes: 2020. Diabetes Care. 2020;43(Suppl 1):S14-31.
Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, Diabetes Control and Complications Trial Research Group, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–86.
International Diabetes Federation Guideline Development Group. Guideline for management of postmeal glucose in diabetes. Diabetes Res Clin Pract. 2014;103(2):256–68.
Madsbad S. Impact of postprandial glucose control on diabetes-related complications: how is the evidence evolving? J Diabetes Complications. 2016;30(2):374–85.
American Diabetes Association. Pharmacologic approaches to glycemic treatment. Standards of medical care in diabetes: 2020. Diabetes Care. 2020;43(Suppl 1):S98–110.
Davies MJ, D’Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, et al. Management of hyperglycemia in type 2 diabetes, 2018: a consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669–701.
Guerci B, Sauvanet JP. Subcutaneous insulin: pharmacokinetic variability and glycemic variability. Diabetes Metab. 2005;31(4 Pt 2):4s7-24.
Grunberger G. Insulin analogs: are they worth it? Yes! Diabetes Care. 2014;37(6):1767–70.
Heinemann L, Heise T, Wahl LC, Trautmann ME, Ampudia J, Starke AA, et al. Prandial glycaemia after a carbohydrate-rich meal in type I diabetic patients: using the rapid acting insulin analogue [Lys(B28), Pro(B29)] human insulin. Diabet Med. 1996;13(7):625–9.
Heinemann L, Muchmore DB. Ultrafast-acting insulins: state of the art. J Diabetes Sci Technol. 2012;6(4):728–42.
Kalra S, Gupta Y. Ultra-fast acting insulin analogues. Recent Pat Endocr Metab Immune Drug Discov. 2014;8(2):117–23.
Eli Lilly and Company. Humalog (insulin lispro injection): highlights of prescribing information. 2015. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/020563s172,205747s008lbl.pdf. Accessed 24 Oct 2019.
Pratt E, Leohr J, Heilmann C, Johnson J, Landschulz W. Treprostinil causes local vasodilation, is well tolerated, and results in faster absorption of insulin lispro (abstract 975-P). Diabetes. 2017;66(Suppl 1):A253.
Michael M, Zhang C, Siesky A, Cox A, Sperry A, Hansen R, et al. Exploration of the mechanism of accelerated absorption for a novel insulin lispro formulation. Diabetes. 2017;66(Suppl 1):A250.
Heise T, Linnebjerg H, Coutant D, LaBell E, Zijlstra E, Kapitza C, et al. Ultra rapid lispro lowers postprandial glucose and more closely matches normal physiological glucose response compared to other rapid insulin analogues: a phase 1 randomized, crossover study. Diabetes Obes Metab. 2020;22(10):1789–98.
Klaff L, Cao D, Dellva MA, Tobian J, Miura J, Dahl D, et al. Ultra rapid lispro improves postprandial glucose control compared with lispro in patients with type 1 diabetes: results from the 26-week PRONTO-T1D study. Diabetes Obes Metab. 2020;22(10):1799–807.
Blevins T, Zhang Q, Frias JP, Jinnouchi H, Chang AM. Randomized double-blind clinical trial comparing ultra rapid lispro with lispro in a basal-bolus regimen in patients with type 2 diabetes: PRONTO-T2D. Diabetes Care. 2020;43(12):2991–8.
Leohr J, Dellva MA, LaBell ES, Coutant DE, Klein O, Plum-Moerschel L, et al. Pharmacokinetic and glucodynamic responses of ultra rapid lispro (URLi) vs Humalog (Lispro) across a clinically relevant range of subcutaneous doses in healthy subjects. Clin Ther. 2020;42(9):1762-77.e4. https://doi.org/10.1016/j.clinthera.2020.07.005.
Linnebjerg H, Zhang Q, LaBell E, Dellva MA, Coutant DE, Hövelmann U, et al. Pharmacokinetics and glucodynamics of ultra rapid Lispro (URLi) versus Humalog® (Lispro) in younger adults and elderly patients with type 1 diabetes mellitus: a randomised controlled trial. Clin Pharmacokinet. 2020;59(12):1589–99. https://doi.org/10.1007/s40262-020-00903-0.
Leohr J, Dellva MA, Coutant DE, LaBell E, Heise T, Andersen G, et al. Pharmacokinetics and glucodynamics of ultra rapid lispro (URLi) versus Humalog® (Lispro) in patients with type 2 diabetes mellitus: a phase I randomised, crossover study. Clin Pharmacokinet. 2020;59(12):1601–10. https://doi.org/10.1007/s40262-020-00901-2.
Haidar A, Duval C, Legault L, Rabasa-Lhoret R. Pharmacokinetics of insulin aspart and glucagon in type 1 diabetes during closed-loop operation. J Diabetes Sci Technol. 2013;7(6):1507–12.
Monnier L, Lapinski H, Colette C. Contributions of fasting and postprandial plasma glucose increments to the overall diurnal hyperglycemia of type 2 diabetic patients: variations with increasing levels of HbA(1c). Diabetes Care. 2003;26(3):881–5.
Krzymien J, Ladyzynski P. Insulin in type 1 and type 2 diabetes: should the dose of insulin before a meal be based on glycemia or meal content? Nutrients. 2019;11(3):607.
Acknowledgements
Medical writing assistance was provided by Sandra Kurian, MPharm, and Tania Dickson, PhD, CMPP, of ProScribe—Envision Pharma Group, and was funded by Eli Lilly and Company. ProScribe’s services complied with the international guidelines for Good Publication Practice (GPP3).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was sponsored by Eli Lilly and Company. Eli Lilly and Company was involved in the study design, data analysis, and preparation of the manuscript, and provided support for Open Access.
Conflicts of Interest/Competing Interests
Jennifer Leohr, Mary Anne Dellva, Kallin Carter, Elizabeth LaBell, and Helle Linnebjerg are employees and shareholders of Eli Lilly and Company.
Ethics approval
All trials were conducted in accordance with the principles of the Declaration of Helsinki (2000), International Council for Harmonisation, and the E6 Guideline for Good Clinical Practice. Institutional review board approval and written informed consent were obtained from all subjects before conducting any evaluations or study procedures.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Availability of data and material
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
The code used and/or analyzed in the current study is available from the corresponding author on reasonable request.
Authors’ contributions
All authors participated in the interpretation of the study results, and in the drafting, critical revision, and approval of the final version of the manuscript. HL, JL, and MAD were involved in the study design and interpretation of the results. EL was involved in the data extraction. MAD and KC were involved in the statistical analysis. EL and JL conducted the pharmacodynamic and pharmacokinetic analyses.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Leohr, J., Dellva, M.A., Carter, K. et al. Ultra Rapid Lispro (URLi) Accelerates Insulin Lispro Absorption and Insulin Action vs Humalog® Consistently Across Study Populations: A Pooled Analysis of Pharmacokinetic and Glucodynamic Data. Clin Pharmacokinet 60, 1423–1434 (2021). https://doi.org/10.1007/s40262-021-01030-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-021-01030-0