Abstract
Background and Aims
The three direct-acting antiviral regimen of ombitasvir/paritaprevir/ritonavir and dasabuvir (3D regimen) is approved for treatment of hepatitis C virus (HCV) genotype 1 infection. Drug–drug interaction (DDI) studies of the 3D regimen and commonly used medications were conducted in healthy volunteers to provide information on coadministering these medications with or without dose adjustments.
Methods
Three phase I studies evaluated DDIs between the 3D regimen (ombitasvir/paritaprevir/ritonavir 25/150/100 mg once daily + dasabuvir 250 mg twice daily) and hydrocodone bitartrate/acetaminophen (5/300 mg), metformin hydrochloride (500 mg), diazepam (2 mg), cyclobenzaprine hydrochloride (5 mg), carisoprodol (250 mg), or sulfamethoxazole/trimethoprim (SMZ/TMP) (800/160 mg twice daily), all administered orally. DDI magnitude was determined using geometric mean ratios and 90 % confidence intervals for the maximum plasma concentration (C max) and area under the plasma concentration–time curve (AUC).
Results
Changes in exposures (C max and AUC geometric mean ratios) of acetaminophen, metformin, sulfamethoxazole, trimethoprim, and diazepam were ≤25 % upon coadministration with the 3D regimen. The C max and AUC of nordiazepam, an active metabolite of diazepam, increased by 10 % and decreased by 44 %, respectively. Exposures of cyclobenzaprine and carisoprodol decreased by ≤40 and ≤46 %, respectively, whereas exposures of hydrocodone increased up to 90 %. Ombitasvir, paritaprevir, ritonavir, and dasabuvir exposures changed by ≤25 %, except for a 37 % decrease in paritaprevir C max with metformin and a 33 % increase in dasabuvir AUC with SMZ/TMP.
Conclusions
Acetaminophen, metformin, sulfamethoxazole, and trimethoprim can be coadministered with the 3D regimen without dose adjustment. Higher doses may be needed for diazepam, cyclobenzaprine, and carisoprodol based on clinical monitoring. A 50 % lower dose and/or clinical monitoring should be considered for hydrocodone. No dose adjustment is necessary for the 3D regimen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The 3D regimen of ombitasvir/paritaprevir/ritonavir and dasabuvir is approved for the treatment of chronic hepatitis C virus (HCV) infection. As HCV-infected patients often have multiple co-morbidities, polypharmacy is prevalent and drug interactions are a clinically important consideration. |
This article describes three phase I drug interaction studies investigating the effects of coadministered medications on the pharmacokinetics of the 3D regimen, and vice versa. |
The results demonstrated that acetaminophen, metformin, sulfamethoxazole, and trimethoprim have minimal interactions with the 3D regimen and can be coadministered without dose adjustment. Overall exposures (area under the plasma concentration–time curve values) of diazepam (in particular nordiazepam), cyclobenzaprine, and carisoprodol decreased by up to 44 % upon coadministration with the 3D regimen and higher doses may be needed based on clinical monitoring. Plasma concentrations of hydrocodone increased by up to 90 % in the presence of the 3D regimen and a 50 % lower dose and/or clinical monitoring should be considered during coadministration. No dose adjustment is necessary for the 3D regimen when coadministered with any of these medications. |
1 Introduction
Hepatitis C virus (HCV)-infected patients may have multiple co-morbidities and are likely to use medications that have drug–drug interaction (DDI) potential with direct-acting antiviral (DAA) treatments. In a cross-sectional study in over 4000 HCV mono-infected Veteran’s Affairs patients between 2000 and 2013, patients had a median of seven co-morbidities and used seven medications; use of six or more medications was a predictor of contraindicated DDIs with sofosbuvir- or simeprevir-containing therapies [1]. It has been estimated that approximately two-thirds of HCV-infected patients may use one or more medications that have the potential for DDIs involving cytochrome P450 (CYP) 3A [2]. The characterization of DAA drug interaction profiles and the development of recommendations for clinical management of drug interactions will become increasingly important as these agents are used in diverse patient populations in real-world settings.
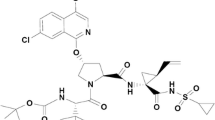
The 3D regimen of paritaprevir, an NS3/4A protease inhibitor, ombitasvir, an NS5A inhibitor, and dasabuvir, a non-nucleoside NS5B polymerase inhibitor, has been approved in several countries for the treatment of patients with chronic HCV genotype 1 infection [3–7]. In addition, the 2D regimen of ombitasvir and paritaprevir/ritonavir has been approved in the USA and Europe for the treatment of HCV genotype 4 infection [8, 9] and in Japan for the treatment of genotype 1 infection. In both regimens, paritaprevir is given with a low dose of the CYP3A inhibitor ritonavir as a pharmacokinetic enhancer to achieve higher peak, trough, and overall paritaprevir exposures [10].
The metabolic and transporter profiles of paritaprevir, ritonavir, ombitasvir, and dasabuvir have been characterized in vitro (Table 1) [11]. Paritaprevir and ritonavir are primarily metabolized by CYP3A, dasabuvir is primarily metabolized by CYP2C8, and to a lesser extent CYP3A, and ombitasvir is predominantly metabolized by amide hydrolysis followed by oxidative metabolism. Ritonavir inhibits CYP3A, whereas the DAAs do not inhibit CYP enzymes. In addition, ritonavir induces CYP3A (in a dose- and time-dependent manner), CYP1A2, CYP2B6, CYP2C9, CYP2C19, and glucuronosyl transferase [12]. At clinically relevant concentrations, paritaprevir inhibits organic anion transporting polypeptide (OATP) 1B1/B3, and paritaprevir, ritonavir, and dasabuvir may inhibit P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP). The DAAs and ritonavir are in vitro substrates of P-gp and BCRP, and paritaprevir is also a substrate of OATP1B1/B3 [11].
Given that the metabolic and transporter profile of the DAA regimens involve multiple enzymes (including CYP3A) and transporters, and that in clinical trials for the 3D regimen, approximately two-thirds of patients were taking two or more concomitant medications [13–15], use of concomitant medications in patients being treated with the 2D or 3D regimen warrants careful consideration with respect to potential drug interactions. In this report, we describe the drug interactions that were evaluated between the 3D regimen and eight medications that are among the top 40 medications used by HCV-infected patients in clinical practice in the USA: hydrocodone/acetaminophen, metformin, diazepam, cyclobenzaprine, carisoprodol, and sulfamethoxazole/trimethoprim (SMZ/TMP) [2]. Hydrocodone, diazepam, cyclobenzaprine, carisoprodol, and SMZ/TMP are substrates or inhibitors of various CYP enzymes [16–20] and may interact with the 2D or 3D regimen. Acetaminophen is metabolized by glucuronidation [21] and is not expected to interact with the 3D regimen but, together with hydrocodone, is the most frequently prescribed medication in HCV-infected patients [2]. Similarly, metformin, which is a substrate for organic cation transporter (OCT) 1 and OCT2 transporters and has low drug interaction potential, is prescribed in patients with type 2 diabetes mellitus [22, 23], a common co-morbidity in patients with chronic HCV infection [2].
2 Subjects and Methods
2.1 Participants and Study Designs
Three open-label, two-arm, phase I clinical studies were conducted at two clinical study sites in accordance with Good Clinical Practice guidelines and ethical principles that have their origin in the Declaration of Helsinki. All study protocols and amendments were approved by the institutional review boards at each site and written informed consent was obtained from each subject before any study-related procedures were performed.
Male and female subjects between the ages of 18 and 55 years, inclusive, who were in general good health and had a body mass index of ≥18 to <30 kg/m2 were eligible to enroll. Subjects who had positive test results for HIV or hepatitis A, B, or C, or use of known inhibitors or inducers of CYP3A or 2C8 enzymes or OATP1B1/1B3 within 1 month prior to study drug administration were excluded from participation. Subjects who had a history of immune thrombocytopenia, folate deficiency, bronchial asthma, malabsorption syndrome, current malnutrition status, thyroid dysfunction, or porphyria were excluded from enrollment in the SMZ/TMP treatment arm. Consumption of grapefruit, Seville oranges, starfruit, or products containing any of these ingredients, alcohol, and/or quinine/tonic water within 72 h, or use of tobacco or nicotine-containing products within 6 months prior to study drug administration was not allowed.
Key elements of the parallel-arm designs used in each of the three studies are presented in Fig. 1. Subjects received standardized diets of approximately 2200 calories per day, with 40 % of calories from fat and up to 45 % of calories from carbohydrates, throughout the studies. Once-daily doses of ombitasvir/paritaprevir/ritonavir 25/150/100 mg were administered orally 30 min after breakfast, and twice-daily doses of dasabuvir 250 mg were administered orally 30 min after breakfast and the evening snack for 14 days. Single oral doses of hydrocodone bitartrate/acetaminophen, metformin hydrochloride, diazepam, cyclobenzaprine hydrochloride, and carisoprodol (Table 2) were each administered approximately 30 min after breakfast on Day 1, and again on Days 17, 19, 36, 20, and 18, respectively, at the same time as ombitasvir/paritaprevir/ritonavir and the morning dose of dasabuvir (Fig. 1).
For the SMZ/TMP treatment arm, a single dose of ombitasvir/paritaprevir/ritonavir 25/150/100 mg and dasabuvir 250 mg was administered 30 min after breakfast on Day 1 and Day 11. Twice-daily oral doses of SMZ/TMP (Table 2) were administered 30 min after breakfast and the evening snack on Days 9 through 14 (Fig. 1).
Each subject received the 3D regimen alone, one of the medications alone, and the 3D regimen and a medication in combination.
2.2 Safety and Tolerability Assessments
Safety and tolerability were assessed throughout each study based on adverse event monitoring, vital signs measurements, physical examinations, electrocardiogram assessments, and laboratory tests.
2.3 Pharmacokinetic Assessments
Blood samples for determination of plasma concentrations of paritaprevir, ritonavir, ombitasvir, dasabuvir, dasabuvir metabolite M1, and the interacting medications and their metabolites, if applicable, were collected by venipuncture during the intensive pharmacokinetic sampling intervals shown in Fig. 1. Plasma concentrations of the DAAs and ritonavir were determined simultaneously using a validated liquid chromatography with tandem mass spectrometric detection (LC–MS/MS) method, as described previously [26]. Blood samples for determination of plasma concentrations of the concomitant medications were collected into potassium-EDTA tubes and centrifuged at 1100–1600×g to separate plasma. Plasma concentrations of the medications were measured using validated LC-MS/MS methods (hydrocodone and acetaminophen—PPD, Middleton, WI, USA; metformin, diazepam, and nordiazepam—Worldwide Clinical Trials, Austin, TX, USA; cyclobenzaprine, norcyclobenzaprine, carisoprodol, meprobamate, sulfamethoxazole, and trimethoprim—inVentiv Health Clinique Inc., Quebec, QC, Canada). The calibration curves for paritaprevir, ombitasvir, dasabuvir, dasabuvir M1 metabolite, and ritonavir ranged from 0.601 to 408, 0.462 to 313, 4.58 to 3100, 4.77 to 3230, and 4.98 to 3340 ng/mL, respectively. The calibration ranges for the concomitant medications were hydrocodone 0.10–50.0 ng/mL, acetaminophen 100–15,000 ng/mL, metformin 20–3000 ng/mL, diazepam and nordiazepam 1–500 ng/mL, cyclobenzaprine 0.05–12.5 ng/mL, norcyclobenzaprine 0.005–2.5 ng/mL, carisoprodol and meprobamate 30–3000 ng/mL, sulfamethoxazole 500–200,000 ng/mL, and trimethoprim 10–4000 ng/mL. Samples quantified below the lowest standard were reported as zero.
Pharmacokinetic parameters were estimated by non-compartmental methods using SAS® version 9.2 (SAS Institute, Inc., Cary, NC, USA). The primary pharmacokinetic parameters of interest were the maximum observed plasma concentration (C max), the area under the plasma concentration–time curve (AUC) during a dosing interval (AUC12 for twice-daily administration; AUC24 for once-daily administration) or from time zero to infinity (AUC∞ for single dose), and plasma trough concentration (C trough; C 24 for medications administered once daily and C 12 for medications administered twice daily) where applicable. Additional pharmacokinetic parameters that were calculated and reported were the time to C max (t max), and, where appropriate, terminal phase elimination half-life(t ½).
2.4 Statistical Analyses
To assess the effect of the 3D regimen on each concomitant medication, and vice versa, repeated measures analyses were performed for the natural logarithms of C max, AUC, and C trough (where applicable). The models had study day as a fixed effect. The within-subject correlation was accounted for by utilizing the repeated statement for the effect of day. The effect of coadministration of the 3D regimen with each medication compared with that of the 3D regimen or each medication administered alone was assessed by the point estimates and the 90 % confidence intervals (CIs) of the geometric mean ratios for C max, AUC, and C trough (where applicable) based on the repeated measures analyses. The point estimates and the 90 % CIs were obtained by taking the anti-logarithm of the differences in the least squares means on the logarithmic scale, as well as the upper and lower limits of the 90 % CIs for the differences within the framework of the repeated measures analysis models. Statistical analyses were conducted using SAS® version 9.2.
3 Results
3.1 Subject Demographics
A total of 82 subjects (60 male, 22 female) were enrolled in the three studies. One male subject withdrew from the SMZ/TMP arm on Day 7 due to non-medical personal reasons and was not included in the pharmacokinetic analyses. Across the studies, 52.4 % of subjects were white, 46.3 % of subjects were black, and 1.2 % of subjects were Asian. Across the treatment arms, the mean age of subjects ranged from 31.9 to 37.7 years (minimum–maximum: 20–52 years) and the mean body mass index ranged from 25.0 to 26.5 kg/m2 (minimum–maximum: 19.3–30.3 kg/m2).
3.2 Pharmacokinetics
Changes in C max, AUC, and C trough values for the DAAs and ritonavir are presented in Fig. 2. Changes in C max, AUC, and C trough (where applicable) values for the concomitant medications and metabolites are presented in Fig. 3. DDIs between the 3D regimen and each medication are discussed below. Changes in exposures of the dasabuvir M1 metabolite, which possesses antiviral activity, generally mirrored those of dasabuvir and are not shown.
Effect of commonly coadministered medications on ombitasvir, paritaprevir, ritonavir, and dasabuvir exposures. Geometric mean ratios indicate C max (open circles), AUC (open squares), and C trough (open triangles) values for coadministration of the 3D regimen with the medication versus administration of the 3D regimen alone. C trough samples were not obtained in the presence of SMZ/TMP. Geometric mean ratios were obtained by taking antilogarithm of the difference of the least squares means on the logarithmic scale within the framework of the repeated measures analysis model. 3D regimen ombitasvir/paritaprevir/ritonavir and dasabuvir, AUC area under the plasma concentration–time curve from time 0–24 h (AUC24) for ombitasvir, paritaprevir, and ritonavir, time 0–12 h (AUC12) for dasabuvir, and time 0 to infinity (AUC∞) for ombitasvir, paritaprevir, dasabuvir, and ritonavir during coadministration with SMZ/TMP, CI confidence interval, C max maximum plasma concentration, C trough plasma trough concentration at 24 h (C 24) for medications administered once daily and 12 h (C 12) for medications administered twice daily, SMZ/TMP sulfamethoxazole/trimethoprim
Effect of the 3D regimen on exposures of commonly coadministered medications and applicable metabolites. Geometric mean ratios indicate C max (open circles), AUC (open squares), and C trough (open triangles) values for coadministration of the medication with the 3D regimen versus administration of the medication alone. C trough samples were obtained only for sulfamethoxazole and trimethoprim. Geometric mean ratios were obtained by taking the antilogarithm of the difference of the least squares means on the logarithmic scale within the framework of the repeated measures analysis model. 3D regimen ombitasvir/paritaprevir/ritonavir and dasabuvir, AUC area under the plasma concentration–time curve from time 0 to 12 h (AUC12) for sulfamethoxazole and trimethoprim and time 0 to infinity (AUC∞) for all other medications and metabolites, CI confidence interval, C trough plasma trough concentration at 24 h (C 24) for medications administered once daily and 12 h (C 12) for medications administered twice daily
3.2.1 Hydrocodone/Acetaminophen
In the presence of the 3D regimen, hydrocodone C max and AUC values increased by 27 and 90 %, respectively, while acetaminophen C max and AUC values were not affected (<20 % increase). The median t max occurred at 2.0 h for hydrocodone and acetaminophen and did not change in the presence of the 3D regimen. The hydrocodone harmonic mean t ½ increased from 5.1 to 8.0 h and the acetaminophen harmonic mean t ½ increased from 3.7 to 5.0 h.
DAA and ritonavir exposures (C max, AUC, and C trough) were unaffected by coadministration with hydrocodone/acetaminophen (<20 % change).
3.2.2 Metformin
The metformin C max decreased by 23 % in the presence of the 3D regimen, but the AUC value did not change (<20 % decrease). The metformin median t max (4.0 h) and harmonic mean t ½ (3.3–3.8 h) were not affected by coadministration with the 3D regimen.
The C max and AUC values for the DAAs and ritonavir were similar with and without metformin, except for a 37 % decrease in the C max for paritaprevir. The C trough value increased slightly for paritaprevir (22 %) and did not change (<20 % increase or decrease) for the other DAAs or ritonavir.
3.2.3 Diazepam
Coadministration of the 3D regimen with diazepam had no effect (<20 % increase) on the C max values for diazepam or nordiazepam (major metabolite of diazepam), but decreased the AUC values of diazepam and nordiazepam by 22 and 44 %, respectively. The diazepam median t max (2.0 h) was the same and the harmonic mean t ½ (31–36 h) was similar during coadministration with the 3D regimen; however, the nordiazepam median t max decreased from 96 to 48 h and the nordiazepam harmonic mean t ½ decreased from 137 to 66 h.
The exposures (C max, AUC, and C trough) of the DAAs and ritonavir did not change (<20 % change) upon coadministration with diazepam.
3.2.4 Cyclobenzaprine
Cyclobenzaprine exposures decreased in the presence of the 3D regimen by 32 and 40 % for C max and AUC, respectively. Norcyclobenzaprine (cyclobenzaprine metabolite) C max was not affected (<20 % change) by the 3D regimen, but norcyclobenzaprine AUC decreased by 26 %. Coadministration of cyclobenzaprine with the 3D regimen did not affect the cyclobenzaprine median t max (5.0 h) or harmonic mean t ½ (28–32 h), but decreased the norcyclobenzaprine median t max from 36 to 24 h and the harmonic mean t ½ from 86 to 53 h.
Cyclobenzaprine had no effect on the exposures (<20 % change in C max, AUC, or C trough) of the DAAs or ritonavir.
3.2.5 Carisoprodol
During coadministration with the 3D regimen, carisoprodol C max and AUC values decreased by 46 and 38 %, respectively, whereas meprobamate (carisoprodol metabolite) C max and AUC values did not change (<20 % increase or decrease). The carisoprodol median t max (2.0 h) and harmonic mean t ½ (1.6–1.7 h) and meprobamate median t max (3.0–4.0 h) and harmonic mean t ½ (8.6–9.6 h) were similar (<20 % change) in the presence of the 3D regimen.
The exposures of the DAAs and ritonavir were similar (<20 % change) in the absence and presence of carisoprodol.
3.2.6 Sulfamethoxazole/Trimethoprim (SMZ/TMP)
Sulfamethoxazole and trimethoprim exposures did not change (≤20 % increase) in the presence of the 3D regimen except for the sulfamethoxazole C max, which increased by 21 %, and the trimethoprim AUC and C trough, which increased by 22 and 25 %, respectively. Median t max values for sulfamethoxazole (3.0 h) and trimethoprim (2.0 h) were not affected.
In the presence of SMZ/TMP, the paritaprevir C max value decreased by 22 % and the dasabuvir AUC value increased by 33 %. Other exposure parameters for paritaprevir and dasabuvir were unaffected (<20 % change). Exposures of ombitasvir and ritonavir were likewise not affected (<20 % change).
3.2.7 Direct-Acting Antiviral and Ritonavir Time to Maximum Concentration and Half-Life
Coadministration of the 3D regimen with the medications described above generally had little to no effect on the median t max values (4.0–5.0 h) for the DAAs or ritonavir. The only exception was for the paritaprevir median t max, which increased from 4.0 to 5.5 h in the presence of metformin.
The harmonic mean t ½ of dasabuvir increased from 5.4 to 7.7 h in the presence of SMZ/TMP, but the harmonic mean t ½ values for the other DAAs and ritonavir were not affected. DAA and ritonavir harmonic mean t ½ values were not calculated for the other arms because the blood sampling times were limited to 24 h due to the multiple-dose study designs.
3.3 Safety
Coadministration of single and multiple doses of the 3D regimen with the concomitant medications was well-tolerated by the 82 healthy subjects in the three phase I studies. No unexpected safety findings were observed. The majority of adverse events were mild in severity and, aside from somnolence, which was reported by five subjects receiving carisoprodol, no other adverse event was reported by more than two subjects in any treatment period. One subject was discontinued from the diazepam arm due to a non-serious, mild adverse event of angioedema to the lower lip on Day 35 (post-treatment Day 1) while receiving the 3D regimen. The last dose administration of study drugs occurred on the evening of Day 34 and the investigator considered the event to have a reasonable possibility of being related to study drug. The event resolved with diphenhydramine. One subject in the hydrocodone/acetaminophen arm became pregnant during the study and elected to end the pregnancy on Day 22, 4 days after the last dose of study drugs. The subject had negative serum pregnancy tests on Day –15 (screening) and Day –1, and a positive serum pregnancy test on Day 19 (post-treatment Day 1).
Across studies, no clinically meaningful changes in vital signs values, electrocardiogram parameters, or laboratory values were observed. One subject in the SMZ/TMP arm experienced an increase in systolic blood pressure, reported as moderate hypertension, on Day 8. The event was assessed as having no possibility of being related to the single dose of the 3D regimen administered on Day 1.
4 Discussion
Patients being treated for chronic HCV infection are at risk for drug interactions due to a high burden of age-related and disease co-morbidity. Drug interactions may lead to poor treatment outcomes, including toxicity and discontinuation of treatment, which increases the chance of viral resistance and may limit future treatment options. The clinical relevance of potential drug interactions was evaluated in light of information available in the prescribing information and published literature for each medication. Dosing recommendations for these medications are discussed in the following sections and are summarized in Table 3.
4.1 Hydrocodone/Acetaminophen
The risk of drug interactions with hydrocodone/acetaminophen and other opioids and analgesics is a concern not only because they are commonly used, but also because the doses may be adjusted by patients based on their pain levels, and prescribers may not be aware of the total acetaminophen intake, which could come from multiple sources [24, 25].
Hydrocodone is metabolized by CYP3A4 and CYP2D6 and its exposures are increased by drugs known to inhibit these enzymes [16]. Acetaminophen is metabolized via glucuronidation [16] and was not expected to interact with the 3D regimen, although inhibition of UDP glucuronosyltransferases (UGTs) by the DAAs could have affected acetaminophen exposures.
Coadministration of hydrocodone/acetaminophen with the 3D regimen increased hydrocodone exposures by 27–90 %, consistent with ritonavir-mediated inhibition of CYP3A4 [11]. Based on the magnitude of the interaction, a 50 % reduction in hydrocodone dose and/or clinical monitoring are recommended when hydrocodone is coadministered with the 3D regimen. Coadministration of hydrocodone/acetaminophen with the 3D regimen had a small effect on the acetaminophen t ½ (increase from 3.7 to 5.0 h) and overall exposure (17 % increase in AUC), suggesting little or no effect of the 3D regimen on UGTs. The small increase in acetaminophen overall exposure may have been due to the increase in t ½. The acetaminophen C max value did not change, suggesting that the 3D regimen did not affect acetaminophen uptake or metabolism in the gut. Because slight increases in acetaminophen exposures are not expected to affect the safety profile, no dose adjustment is needed for acetaminophen when it is coadministered with the 3D regimen.
4.2 Metformin
Although interactions were not expected because metformin is not a substrate or inhibitor of CYP enzymes, a lack of interaction with the 3D regimen had not been demonstrated in vivo. The 10 % decrease in metformin AUC in the presence of the 3D regimen confirmed that no dose adjustment is needed when metformin is coadministered with the 3D regimen. The small change in the metformin AUC also confirmed that the 3D regimen does not inhibit OCT1 or OCT2 transporters in vivo.
4.3 Diazepam
Diazepam undergoes metabolism via CYP3A4 and CYP2C19 and forms a major N-demethylated active metabolite, nordiazepam [17]. Drug interactions may be expected when diazepam is coadministered with agents that affect CYP2C19 and/or CYP3A4. The AUC values for diazepam and nordiazepam decreased by 22 and 44 %, respectively, when diazepam was coadministered with the 3D regimen, indicating that the 3D regimen had a mild inductive effect on CYP2C19 that outweighed CYP3A4 inhibition by ritonavir. Inhibition of CYP3A4 by ritonavir may have shifted diazepam metabolism primarily to CYP2C19, which can be induced by ritonavir, resulting in a decrease in diazepam AUC. In addition, inhibition of intestinal CYP3A may have caused the 18 % increase in diazepam C max. By this mechanism, the overall exposure (AUC∞) of nordiazepam would have been expected to increase; however, in the current study it decreased by 44 %. The mechanism by which this phenomenon occurred is unknown. There may be other hepatic enzymes and/or transporters in addition to CYP3A4 that are involved in the disposition of nordiazepam that were affected by the 3D regimen.
Whereas the nordiazepam AUC∞ decreased by 44 %, the nordiazepam AUC from time zero to time t (AUCt) decreased by only 3 % (data not shown). This difference reflects the greater proportion of AUC that was extrapolated after the last measurable timepoint for nordiazepam (46 vs. 20 % without and with the 3D regimen, respectively) due to the decrease in the nordiazepam harmonic mean t ½ from 137 to 66 h.
The minimal to modest decreases in diazepam and nordiazepam AUC values do not necessitate a priori dose adjustment for diazepam, though higher doses should be considered if clinically indicated.
4.4 Cyclobenzaprine and Carisoprodol
Cyclobenzaprine is extensively metabolized and is excreted primarily as glucuronides by the kidneys. The major pathway of carisoprodol metabolism is via the liver by CYP2C19 to form meprobamate, which has anxiolytic and sedative properties. CYP3A4, CYP1A2, and to a lesser extent CYP2D6 mediate N-demethylation, one of the oxidative pathways for cyclobenzaprine metabolism.
Cyclobenzaprine and carisoprodol exposures decreased by up to 46 % in the presence of the 3D regimen, likely due to CYP1A2 and CYP2C19 induction, respectively, by ritonavir. A similar interaction was observed when the CYP2C19 substrate omeprazole was coadministered with the 3D regimen—omeprazole exposures decreased by ~40 % [26]. For both cyclobenzaprine and carisoprodol, exposures of the major metabolites were minimally affected (≤26 % change).
Elimination of the cyclobenzaprine metabolite norcyclobenzaprine has not been well-characterized due to its long t ½, and in the current study the pharmacokinetic sampling times were based primarily on the t ½ of the parent compound. Whereas norcyclobenzaprine AUC∞ decreased by 26 %, norcyclobenzaprine AUCt decreased by only 7 % (data not shown). This difference reflects the greater proportion of AUC extrapolated after the last measurable timepoint for norcyclobenzaprine (42 vs. 21 % without and with the 3D regimen, respectively) due to the decrease in norcyclobenzaprine harmonic mean t ½ from 86 to 53 h. The reason for the decreased norcyclobenzaprine t max during coadministration with the 3D regimen is unclear due to the limited information regarding norcyclobenzaprine distribution and elimination.
Carisoprodol is almost entirely metabolized by CYP2C19 to meprobamate; thus, induction of CYP2C19 would not be expected to affect the fraction of carisoprodol metabolized to meprobamate. A similar interaction has been reported for the effect of rifampicin (rifampin) on midazolam, where induction reduces the plasma concentration of midazolam but has minimal effect on urinary excretion of the metabolite 1-hydroxy midazolam [27].
No a priori dose adjustments are required for cyclobenzaprine or carisoprodol in HCV-infected patients being treated with the 3D regimen, but higher doses should be considered if clinically indicated.
4.5 Sulfamethoxazole/Trimethoprim (SMZ/TMP)
Potential interactions between SMZ/TMP and the 3D regimen were evaluated because trimethoprim is a weak to moderate CYP2C8 inhibitor [20, 28, 29] that has the potential to increase exposures of dasabuvir, which is metabolized by CYP2C8. Strong CYP2C8 inhibitors such as gemfibrozil are contraindicated with the 3D regimen [30]. In the presence of SMZ/TMP, dasabuvir exposures increased by ≤33 % but dasabuvir M1 exposures decreased by ≤19 % (data not shown), suggesting that weak to moderate CYP2C8 inhibitors do not have a clinically meaningful effect on dasabuvir metabolism. SMZ/TMP exposures increased slightly (≤25 %) upon coadministration with the 3D regimen. The mechanism for these interactions is not known. Similar magnitudes of change in sulfamethoxazole (20 % decrease in AUC) and trimethoprim (20 % increase in AUC) exposures have been observed upon coadministration with ritonavir and no dose adjustments were required [31]. Thus, no dose adjustment is required for sulfamethoxazole or trimethoprim when coadministered with the 3D regimen.
4.6 3D Regimen
Ombitasvir, paritaprevir, ritonavir, and dasabuvir exposures did not change to a clinically meaningful extent upon coadministration with any of the medications. The maximum change in the paritaprevir C max was a 37 % decrease in the presence of metformin. The mechanism for this decrease is not clear and is difficult to determine given the multiple uptake/efflux transporters and enzymes involved in paritaprevir disposition. This small decrease in paritaprevir exposure is not expected to affect the efficacy of the 3D regimen based on evaluations of lower doses of paritaprevir in phase II studies [32, 33]. No dose adjustments are required for the 3D regimen when coadministered with any of the medications evaluated in these studies.
4.7 Extrapolation to 2D Regimen
DDI results from evaluations conducted with the 3D regimen can be extrapolated to the 2D regimen (ombitasvir/paritaprevir/ritonavir 25/150/100 mg once daily) based on the mechanism of interaction. Similar to the 3D regimen, no interactions are expected between the 2D regimen and acetaminophen, metformin, sulfamethoxazole, or trimethoprim; thus, no dose adjustments are required for these medications. Diazepam, carisoprodol, cyclobenzaprine, and hydrocodone interactions with the 3D regimen appear to be mediated primarily by ritonavir, which is also part of the 2D regimen; therefore, the dosing recommendations for the 2D regimen are the same as for the 3D regimen—a higher dose may be needed for diazepam, carisoprodol, and cyclobenzaprine based on clinical monitoring and a 50 % dose reduction and/or clinical monitoring should be considered for hydrocodone. No dose adjustments are required for the 2D regimen when it is coadministered with any of the medications.
5 Conclusions
Drug interactions between the 3D regimen and eight medications commonly prescribed in HCV-infected patients were evaluated in healthy volunteers to provide dosing recommendations for HCV-infected patients. Results from these studies can be applied to the 2D regimen and to other medications that have metabolic or transporter profiles that overlap with those of the DAAs and ritonavir [15, 30, 34]. Similarly, although these studies were conducted in healthy volunteers, population pharmacokinetic analyses have shown that DAA and ritonavir exposures in HCV genotype 1-infected patients are comparable with those from healthy volunteers [35] and the magnitudes of drug interactions are expected to be the same. Acetaminophen, metformin, sulfamethoxazole, and trimethoprim can be coadministered with the DAA regimens without dose adjustment. A higher dose may be needed for diazepam, carisoprodol, and cyclobenzaprine based on clinical monitoring. A 50 % dose reduction and/or clinical monitoring should be considered for hydrocodone. No dose adjustment is necessary for the 2D or 3D regimen when coadministered with any of the concomitant medications.
References
Patel N, Nasiri M, Koroglu A, Bliss S, Davis M, McNutt LA, et al. A cross-sectional study comparing the frequency of drug interactions after adding simeprevir- or sofosbuvir-containing therapy to medication profiles of hepatitis C monoinfected patients. Infect Dis Ther. 2015;4:67–78.
Lauffenburger JC, Mayer CL, Hawke RL, Brouwer KL, Fried MW, Farley JF. Medication use and medical comorbidity in patients with chronic hepatitis C from a US commercial claims database: high utilization of drugs with interaction potential. Eur J Gastroenterol Hepatol. 2014;26:1073–82.
Feld JJ, Kowdley KV, Coakley E, Sigal S, Nelson DR, Crawford D, et al. Treatment of HCV with ABT-450/r-ombitasvir and dasabuvir with ribavirin. N Engl J Med. 2014;370:1594–603.
Zeuzem S, Jacobson IM, Baykal T, Marinho RT, Poordad F, Bourlière M, et al. Retreatment of HCV with ABT-450/r-ombitasvir and dasabuvir with ribavirin. N Engl J Med. 2014;370:1604–14.
Andreone P, Colombo MG, Enejosa JV, Koksal I, Ferenci P, Maieron A, et al. ABT-450, ritonavir, ombitasvir, and dasabuvir achieves 97 and 100 % sustained virologic response with or without ribavirin in treatment-experienced patients with HCV genotype 1b infection. Gastroenterology. 2014;147:359–65.
Poordad F, Hezode C, Trinh R, Kowdley KV, Zeuzem S, Agarwal K, et al. ABT-450/r-ombitasvir and dasabuvir with ribavirin for hepatitis C with cirrhosis. N Engl J Med. 2014;370:1973–82.
Ferenci P, Bernstein D, Lalezari J, Cohen D, Luo Y, Cooper C, et al. ABT-450/r-ombitasvir and dasabuvir with or without ribavirin for HCV. N Engl J Med. 2014;370:1983–92.
Chayama K, Notsumata K, Kurosaki M, Sato K, Rodrigues L Jr, Setze C, et al. Randomized trial of interferon- and ribavirin-free ombitasvir/paritaprevir/ritonavir in treatment-experienced HCV-infected patients. Hepatology. 2015;61:1523–32.
Hézode C, Asselah T, Reddy KR, Hassanein T, Berenguer M, Fleischer-Stepniewska K, et al. Ombitasvir plus paritaprevir plus ritonavir with or without ribavirin in treatment-naive and treatment-experienced patients with genotype 4 chronic hepatitis C virus infection (PEARL-I): a randomised, open-label trial. Lancet. 2015;385:2502–9.
Menon RM, Klein CE, Podsadecki TJ, Chiu Y-L, Dutta S, Awni WM. Pharmacokinetics and tolerability of paritaprevir, a direct-acting antiviral agent for HCV treatment, with and without ritonavir in healthy volunteers. Br J Clin Pharmacol. 2016. doi:10.1111/bcp.12873
Bow DAJ, Liu J, Kavetskaia O, Menon R, de Morais SM, Nijsen M, et al. A mechanistic non-clinical assessment of drug-drug interactions (metabolism and transporters) with the hepatitis C virus (HCV) regimen: ABT-450/r, ombitasvir and dasabuvir [poster]. 2014 American Association for the Study of Liver Diseases/European Association for the Study of the Liver Special Conference on Hepatitis C; 12–13 Sep 2014; New York.
Foisy MM, Yakiwchuk EM, Hughes CA. Induction effects of ritonavir: implications for drug interactions. Ann Pharmacother. 2008;42:1048–59.
Mensing S, Sharma S, Eckert D, Polepally A, Khatri A, Podsadecki T, et al. Pharmacokinetics of paritaprevir, ombitasvir, dasabuvir, ritonavir and ribavirin in subjects with HCV genotype 1 infection in phase 3 studies. J Hepatol. 2015;62:S644.
Polepally AR, Badri P, Coakley EP, Parikh A, Rodrigues L Jr, DaSilva-Tillmann BA, et al. Effect of comedications on paritaprevir, ritonavir, ombitasvir, dasabuvir and ribavirin pharmacokinetics [abstract no. 52]. Rev Antiviral Ther Infect Dis. 2015;4:56.
Badri PS, King JR, Polepally AR, McGovern BH, Dutta S, Menon RM. Dosing recommendations for concomitant medications during 3D anti-HCV therapy. Clin Pharmacokinet. 2015. doi:10.1007/s40262-015-0317-8 (Epub 2015 Sep 2).
Vicodin® (hydrocodone bitartrate/acetaminophen) tablets [package insert]. Whippany: Manufactured for AbbVie Inc. by Halo Pharmaceutical Inc.; 2013.
Valium® (diazepam) tablets [package insert]. Nutley: Roche Products Inc.; 2008.
Cyclobenzaprine hydrochloride tablets [package insert]. Salisbury: Jubilant Cadista Pharmaceuticals Inc.; 2013.
Soma® (carisoprodol) tablets [package insert]. Somerset: Meda Pharmaceuticals Inc.; 2013.
Bactrim™ (sulfamethoxazole/trimethoprim) [package insert]. Philadelphia: AR Scientific, Inc.; 2013.
Tylenol® (acetaminophen) tablets [professional product information]. Washington: McNeil Consumer Healthcare; 2010.
Glucophage® (metformin) [package insert]. Princeton: Bristol-Myers Squibb Company.; 2009.
Kimura N, Masuda S, Tanihara Y, Ueo H, Okuda M, Katsura T, Inui K. Metformin is a superior substrate for renal organic cation transporter OCT2 rather than hepatic OCT1. Drug Metab Pharmacokinet. 2005;20:379–86.
Smith HS. Opioid metabolism. Mayo Clin Proc. 2009;84:613–24.
Bruce RD, Moody DE, Altice FL, Gourevitch MN, Friedland GH. A review of pharmacological interactions between HIV or hepatitis C virus medications and opioid agonist therapy: implications and management for clinical practice. Expert Rev Clin Pharmacol. 2013;6:249–69.
Polepally AR, Dutta S, Hu B, Podsadecki TJ, Awni WM, Menon RM. Drug-drug interaction of omeprazole with the HCV direct-acting antiviral agents paritaprevir/ritonavir and ombitasvir with and without dasabuvir. Clin Pharm Drug Develop. doi:10.1002/cpdd.246 (Epub 2016 Jan 24).
Gorski JC, Vannaprasaht S, Hamman MA, Ambrosius WT, Bruce MA, Haehner-Daniels B, et al. The effect of age, sex, and rifampin administration on intestinal and hepatic cytochrome P450 3A activity. Clin Pharmacol Ther. 2003;74:275–87.
Tornio A, Niemi M, Neuvonen PJ, Backman JT. Trimethoprim and the CYP2C8*3 allele have opposite effects on the pharmacokinetics of pioglitazone. Drug Metab and Dispos. 2008;36:73–80.
Guidance for Industry: drug interaction studies - study design, data analysis, implications for dosing, and labeling recommendations. Rockville: US Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER); 2012.
Menon RM, Badri PS, Wang T, Polepally AR, Zha J, Khatri A, et al. Drug-drug interaction profile of the all-oral anti-hepatitis C virus regimen of paritaprevir/ritonavir, ombitasvir and dasabuvir. J Hepatol. 2015;63:20–9.
Norvir® (ritonavir) [package insert]. North Chicago: AbbVie, Inc.; 2015.
Poordad F, Lawitz E, Kowdley KV, Cohen DE, Podsadecki T, Siggelkow S, et al. Exploratory study of oral combination antiviral therapy for hepatitis C. N Engl J Med. 2013;368:45–53.
Kowdley KV, Lawitz E, Poordad F, Cohen DE, Nelson DR, Zeuzem S, et al. Phase 2b trial of interferon-free therapy for hepatitis C virus genotype 1. N Engl J Med. 2014;370:222–32.
Badri PS, Dutta S, Wang H, Podsadecki TJ, Polepally AR, Khatri A, et al. Drug interactions with the direct-acting antiviral combination of ombitasvir and paritaprevir/ritonavir (2D regimen). Antimicrob Agents Chemother. 2015;60(1):105–14. doi:10.1128/AAC.01778-15.
Mensing S, Polepally A, Konig D, Khatri A, Liu W, Podsadecki T, et al. Population pharmacokinetics of ABT-450, ombitasvir, dasabuvir, ritonavir, and ribavirin in subjects with HCV genotype 1 infection. J Pharmacokinet Pharmacodyn. 2014;41:S42–3.
Acknowledgments
The authors would like to thank the study investigators, subjects, clinical sites, and AbbVie personnel Kent Kamradt, James Jankowski, Brett Herzberg, Natalie Hycner, Nancy Shulman, Melanie Gloria, Jeffrey Arnold, Kathryn Joiner, Paula Glowinski, Teria Blagg, and Jill Polzin for their contributions to various aspects of the studies. The authors would also like to thank Allison Kitten, an employee of AbbVie, for medical writing support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was sponsored by AbbVie. AbbVie contributed to the study design, research, and interpretation of data, and the writing, reviewing, and approving of the publication. Medical writing support was provided by Allison Kitten, an employee of AbbVie.
Conflicts of interest
All authors are employees of AbbVie and may hold AbbVie stock or stock options.
Ethical approval
The studies were conducted in accordance with Good Clinical Practice guidelines and ethical principles that have their origin in the Declaration of Helsinki. All study protocols and amendments were approved by the institutional review boards at each site.
Informed consent
Written informed consent was obtained from each subject before any study-related procedures were performed.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Polepally, A.R., King, J.R., Ding, B. et al. Drug–Drug Interactions Between the Anti-Hepatitis C Virus 3D Regimen of Ombitasvir, Paritaprevir/Ritonavir, and Dasabuvir and Eight Commonly Used Medications in Healthy Volunteers. Clin Pharmacokinet 55, 1003–1014 (2016). https://doi.org/10.1007/s40262-016-0373-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-016-0373-8