Abstract
Background
Several initiatives to provide trauma care, including ambulance services, creation of a network of trauma hospitals and insurance schemes for cashless treatment, are currently being implemented in India. However, lack of information on the cost of trauma care is an impediment to the evidence-based planning for such initiatives. In this study, we aim to bridge this gap in evidence by estimating the unit cost of an outpatient consultation, inpatient bed-day of hospitalization, surgical procedure and diagnostics for providing trauma care through secondary- and tertiary-level hospitals in India.
Methods
We undertook an economic costing of trauma care in a secondary-care district hospital and a tertiary-level teaching and research hospital in North India. Cost analysis was undertaken using a health system perspective, employing a bottom-up costing methodology. Data on all resources—capital or recurrent—on delivery of trauma care during the period of April 2014 to March 2015 were collected. Standardized unit costs were estimated after adjusting for bed occupancy rates. Sensitivity analysis was performed to account for the uncertainties due to differences in prices and other assumptions.
Results
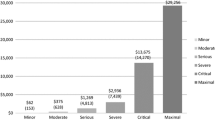
The cost of trauma care in the tertiary care hospital was INR 9585 (US$147.4) per day-care consultation; INR 2470 (US$37.7) per bed-day hospitalization (excluding ICU), INR 12,905 (US$198.5) per bed day in ICU and INR 21,499 (US$330.8) per surgery. Similarly, in the secondary-care hospital, the cost of trauma care was INR 482 (US$7.4) per outpatient consultation, INR 791 (US$12.2) per bed day of hospitalization, INR 186 (US$2.9) per minor surgery and INR 6505 (US$100.1) per major surgery.
Conclusion
The estimates generated can be used for planning and managing trauma care services in India. The findings may also be used for undertaking future research in estimating the cost effectiveness of trauma care services or models of care.


Similar content being viewed by others
References
WHO. Global Health Estimates. Geneva: World Health Organization; 2014.
Pal R, Agarwal A, Galwankar S, Swaroop M, Stawicki S, Rajaram L, et al. The Academic College of Emergency Experts in India’s INDO-US Joint Working Group (JWG) White Paper on “Developing Trauma Sciences and Injury Care in India”. Int J Crit Illn Inj Sci. 2014;4:114–30.
Mohan D. The Road Ahead Traffic Injuries and Fatalities in India. Indian Institute of Technology, New Delhi. WHO Collabrating Centre. 2004.
GoI. Opening of Trauma Centres on the Highways. Press Information Bureau. Government of India. Ministry of Health and Family Welfare. 11-August-2015 13:23 IST; 2015.
Prinja S, Chauhan AS, Karan A, Kaur G, Kumar R. Impact of publicly financed health insurance schemes on health care utilization and financial risk protection in India. PLoS One. 2017;12(2):e0170996.
Prinja S, Jagnoor J, Kaur M, Ivers R. Study for evaluation of ‘National Highway Accident Relief Service Scheme’andcashless scheme of health insurance for road accident victims. 2015. Post Graduate Institute of Medical Education and Research; (unpublished). 2015.
Wesson H, Boikhutso N, Bachani A, Hofman K, Hyder A. The cost of injury and trauma care in low and middle-income countries: a review of economic evidence. Health Policy Plan. 2014;29(6):795.
GoI. Financing and Delivery of Health Care Services in India. National Commission on Macroeconomics and Health. Ministry of Health and family Welfare. Government of India. New Delhi. 2005. www.who.int/macrohealth/action/Background%20Papers%20report.pdf. Accessed 30 Aug 2015.
Kumar GA, Dilip T, Dandona L, Dandona R. Burden of out-of-pocket expenditure for road traffic injuries in urban India. BMC Health Serv Res. 2012;12:285.
Mohanty SK, Srivastava A. Out of Pocket expenditure on institutional delivery in India. Health Policy Plan. 2013;28(3):247–62.
Prinja S, Bahuguna P, Duseja A, Kaur M, Chawla YK. Cost of intensive care treatment for liver disorders in India. Chandigarh: Post Graduate Institute of Medical Education and Research; 2015.
Prinja S, Jagnoor J, Chauhan AS, Aggarwal S, Nguyen H, Ivers R. Economic burden of hospitalization due to injuries in North India: a cohort study. Int J Environ Res Public Health. 2016;13(7):673.
Chatterjee S, Laxminarayan R. Costs of surgical procedures in Indian hospitals. BMJ Open. 2013;3(6):e002844.
Chatterjee S, Levin C, Laxminarayan R. Unit cost of medical services at different hospitals in India. PloS One. 2013;8(7):e69728.
Olukoga A. Unit costs of inpatient days in district hospitals in South Africa. Singap Med J. 2007;48(2):143–7.
La Foucade A, Scott E, Theodore K. Estimating the cost of hospital services in a small island state: a case study of the Milton Cato Memorial Hospital in St Vincent and the Grenadines. West Indian Med J. 2005;54(2):116–22.
Younis M, Jaber S, Mawson A, Hartmann M. Estimating the unit costs of public hospitals and primary healthcare centers. Int J Health Plann Manag. 2013;28(4):320–32.
GoI. Indian Public Health Standards (IPHS). Guidelines for District Hospital. Directorate General of Health Services Ministry of Health & Family Welfare. Government of India. Revised 2012.
Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programme. Third Edition ed. Oxford, 2005.
Prinja S, Manchanda N, Mohan P, Gupta G, Sethy G, Sen A, et al. Cost of neonatal intensive care delivered through district level public hospitals in India. Indian Pediatr. 2013;50:839–46.
Prinja S, Bala D, Jeet G, Verma R, Kumar D, Bahuguna P, et al. Cost of Delivering Secondary Level Health Care Services through Public Sector District Hospitals in India. (Unpublished). 2015.
The Economic Times: Forex Rates. 2015. http://economictimes.indiatimes.com/markets/forex. Accessed 12 Jan 2016.
Hyder AA, Puvanachandra P, Allen KA. Road Traffic Injury and Trauma care: innovations for policy (road trip). World Innovation Summit for Health (WISH). http://www.wish-qatar.org/search-results?q=Road+Traffic+Injury+Report. Doha, Qatar: 2013.
The Economic Times: Government working on ‘pan-India trauma care network’ for road mishaps victims. 2015. http://articles.economictimes.indiatimes.com/2015-08-11/news/65452810_1_trauma-care-facilities-health-minister-jp-nadda-trauma-victim. Accessed 14 Jan 2016.
GoI. Report of the working group on tertiary care institutions for 12th five-year plan (2012–17). Planning Commission. Planning Commission. 2011. www.pmssy-mohfw.nic.in/files/WG_2tertiary.pdf. Accessed 24 Sep 2015.
Kruk ME, Wladis A, Mbembati N, Ndao-Brumblay SK, Hsia RY, et al. Human resource and funding constraints for essential surgery in district hospitalsin Africa: a retrospective cross-sectional survey. PLos Med. 2010;7:e1000242.
Minh HV, Giang KB, Huong DL, Huong LH, Huong NT, et al. Costing of clinical services in rural district hospitals in northern Vietnam. Int J Health Plan Manag. 2010;25:63–73.
Oostenbrink JB, Van der Woude TB, Van Agthoven M, Koopmanschap MA, Rutten FF. Unit costs of inpatient hospital days. Pharmacoeconomics. 2003;21:263–71.
MoHFW. Rashtriya Swasthya Bima Yojana 2014 [cited 2015 20 November]. 2014. http://www.rsby.gov.in/. Accessed 20 Nov 2015.
MoHFW. Central Government Health Scheme India. New Delhi. http://msotransparent.nic.in/cghsnew/index.asp. Accessed 2016 22 July.
Anand K, Kapoor SK, Pandav CS. Cost analysis of a primary health centre in northern India. Natl Med J India. 1993;6(4):160–3.
Krishnan A, Arora N, Pandav C, Kapoor S. Cost of curative pediatric services in a public sector setting. Indian J Pediatr. 2005;72(8):657–60.
Prinja S, Balasubramanian D, Jeet G, Verma R, Kumar D, Bahuguna P, et al. Cost of delivering secondary level health care services through public sector District Hospitals in India. Indian J Med Res (Forthcoming). 2017.
Prinja S, Gupta A, Verma R, Bahuguna P, Kumar D, Kaur M, et al. Cost of delivering health care services in public sector primary and community health centres in North India. PLoS One. 2016;11(8):e0160986. doi:10.1371/journal.pone.
Prinja S, Jeet G, Verma R, Kumar D, Bahuguna P, Kaur M, et al. Economic analysis of delivering primary health care services through community health workers in 3 North Indian States. PLoS One. 2014;9(3):e91781.
Prinja S, Mazumder S, Taneja S, Bahuguna P, Bhandari N, Mohan P, et al. Cost of delivering child health care through community level health workers: how much extra does IMNCI Program Cost? J Trop Pediatr. 2013;59(6):489–95.
Prinja S, Gupta R, Bahuguna P, Sharma A, Aggarwal A, Phogat A, et al. A composite indicator to measure universal health care coverage in India: way forward for post-2015 health system performance monitoring framework. Health Policy and Plann. 2017;32(1):43–56.
Acknowledgements
We are grateful to the office of Medical Superintendent and Accounts Department in Post Graduate Institute of Medical Education and Research, Chandigarh, India for their cooperation in data collection.
Author Contributions
SP and SA conceived the study; AS and SP designed the methods and tools; JJ and RI contributed to development of study methods; AS collected data; SP and SA supervised data collection; AS and PB analysed the data; AS wrote the first draft. All authors revised the manuscript and approved the final version.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No funding was received for this study. AS, SP, SA, JJ, PB and RI declare no conflicts of interest.
Glossary of Abbreviations
Glossary of Abbreviations
Abbreviation | Full form | Remarks |
|---|---|---|
ATC | Advanced Trauma Centre | Centre for provision of specialized trauma care |
CGHS | Central Government Health Scheme | Social health insurance scheme for Central Government Employees |
CT | Computerized tomography | Radiological diagnostic test |
DH | District Hospital | District-based secondary care hospital |
ENT | Ear–Nose–Throat (Otoloaryngology) | Surgical specialty in hospital |
GOI | Government of India | |
INR | Indian National Rupee | Indian currency |
IPD | Inpatient Department | Hospital department providing care after admission, i.e. wards |
IPHS | Indian Public Health Standards | Indian quality standards for health care facilities |
MRI | Magnetic resonance imaging | Radiological diagnostic test |
OPD | Outpatient Department | Hospital department providing outpatient consultations |
OT | Operation theatre | Surgical care |
PCC | Primary Cost Centre | Centre which is responsible for utilization of resources and providing direct patient care |
PMSSY | Prime Minister’s Health Protection Scheme | Central Government’s scheme for strengthening tertiary-care facilities |
RSBY | Rashtriya Swasthya Bima Yojana | India’s national publicly financed health insurance scheme for below poverty line households |
SCC | Secondary Cost Centre | Centre which is responsible for utilization of resources and providing supportive services |
TH | Tertiary Hospital | Hospital providing specialized tertiary-care services |
US$ | United States Dollar | US currency |
Rights and permissions
About this article
Cite this article
Sangwan, A., Prinja, S., Aggarwal, S. et al. Cost of Trauma Care in Secondary- and Tertiary-Care Public Sector Hospitals in North India. Appl Health Econ Health Policy 15, 681–692 (2017). https://doi.org/10.1007/s40258-017-0329-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-017-0329-7