Abstract
Background
In an individual, the development and severity of Non-Communicable Diseases (NCDs) are determined by the presence or absence of clustering of NCD risk factors in them. We aimed to determine the prevalence and the factors associated with clustering of risk factors of NCDs in the district of Puducherry in India.
Methodology
We conducted a community-based cross-sectional survey among the adult population (18–69 years) of Puducherry district (N = 1114) between February 2019 and February 2020. Ten risk factors of NCDs (behavioral, physical measurements and biochemical) were assessed. Individuals having ≥ 3 risk factors were regarded as having clustering of risk factors. Categorical variables are summarized using proportions (95% CI). Adjusted prevalence ratio was estimated using weighted forward stepwise generalized linear modelling.
Results
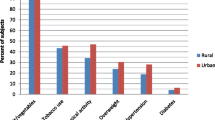
Clustering of NCD risk factors was present in majority (95.2%, 95% CI: 93.8–96.3) of the population. The presence of clustering was significantly higher among women (97.1%, 95% CI: 95.9–98.3) and the urban population (97.2%, 95% CI: 96.1–98.3). The risk factors that primarily drove the high prevalence of clustering were raised salt intake and inadequate intake for fruits and vegetables in nine out of 10 people in the district. Nearly 1 in 10 (13.3%, 95% CI: 11.3–15.3), 1 in 5 (21.5%, 95% CI: 19.1–23.8) and 1 in 4 (26.8%, 95% CI: 24.1–29.4) participants had three, four and five risk factors, respectively.
Conclusion
We highlight the urgent need for population-based health promotion interventions in the district of Puducherry targeting the highly prevalent NCD risk factors, especially among the women and urban populations.

Similar content being viewed by others
References
“Global status report on noncommunicable diseases 2010,” World Health Organization, World Health Organization Regional Office, Geneva. ISBN 978 92 4 068645 8, 2011. [Online]. Available: https://www.who.int/nmh/publications/ncd_report_full_en.pdf.
Indian Council of Medical Research, Public Health Foundation of India, and Institute for Health Metrics and Evaluation., “India: Health of the Nation’s States: The India State-Level Disease Burden Initiative,” New Delhi, ISBN: 978-0-9976462-1-4, 2017. Accessed: Oct. 21, 2020. [Online]. Available: https://phfi.org/the-work/research/the-india-state-level-disease-burden-initiative/.
Organization WH. “From Burden to ‘Best Buys’: Reducing the Economic Impact of Non-Communicable Diseases in Low- and Middle-Income Countries,” World Health Organization, Geneva, Switzerland. [Online]. Available: https://www.who.int/nmh/publications/best_buys_summary.pdf.
Ahmed SM et al. “Clustering of chronic non-communicable disease risk factors among selected Asian populations: levels and determinants,” Glob. Health Action, vol. 2, no. 1, p. 1986, Nov. 2009, https://doi.org/10.3402/gha.v2i0.1986.
Selvaraj K, Kar SS, Ramaswamy G, Premarajan KC, Saya GK, Kalidoss V. “Clustering of cardiovascular disease risk factors - Syndemic approach: Is sit a time to shift toward integrated noncommunicable disease clinic?” Indian J. Public Health, vol. 63, no. 3, pp. 186–193, Sep. 2019, https://doi.org/10.4103/ijph.IJPH_158_18.
Yusuf S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet Lond Engl. Sep. 2004;364:937–52. https://doi.org/10.1016/S0140-6736(04)17018-9.
Gupta R, Misra A, Pais P, Rastogi P, Gupta VP. “Correlation of regional cardiovascular disease mortality in India with lifestyle and nutritional factors,” Int. J. Cardiol, vol. 108, no. 3, pp. 291–300, Apr. 2006, https://doi.org/10.1016/j.ijcard.2005.05.044.
Anjana RM, et al. Prevalence of diabetes and prediabetes in 15 states of India: results from the ICMR-INDIAB population-based cross-sectional study. Lancet Diabetes Endocrinol. 2017;5(8):585–96. https://doi.org/10.1016/S2213-8587(17)30174-2.
National Institute of Medical Statistics and Council of Medical Research., “Integrated Disease Surveillance Project (IDSP): Non-Communicable Disease Risk Factors Survey, Phase 1 states of India, 2007-08,” New Delhi, 2009. Accessed: May 29, 2018. [Online]. Available: http://www.who.int/ncds/surveillance/steps/2007_STEPS_Report_India_7States.pdf.
Pelzom D, Isaakidis P, Oo MM, Gurung MS, Yangchen P. “Alarming prevalence and clustering of modifiable noncommunicable disease risk factors among adults in Bhutan: a nationwide cross-sectional community survey,” BMC Public Health, vol. 17, no. 1, p. 975, Dec. 2017, https://doi.org/10.1186/s12889-017-4989-x.
Aryal KK, et al. The Burden and Determinants of non communicable Diseases Risk factors in Nepal: findings from a nationwide STEPS Survey. PLoS ONE. Aug. 2015;10:e0134834. https://doi.org/10.1371/journal.pone.0134834. no. 8.
Zaman MM, et al. Clustering of non-communicable diseases risk factors in bangladeshi adults: an analysis of STEPS survey 2013. BMC Public Health. Jul. 2015;15(1):659. https://doi.org/10.1186/s12889-015-1938-4.
Directorate General of Health Services and Ministry of Health. & Family welfare, “National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular diseases and Stroke (NPCDCS): Operational Guidelines (Revised: 2013-17),” New Delhi, 2013. Accessed: Jan. 09, 2020. [Online]. Available: https://main.mohfw.gov.in/sites/default/files/Operational%20Guidelines%20of%20NPCDCS%20%28Revised%20-%202013-17%29_1.pdf.
Narain JP. “Integrating Services for Noncommunicable Diseases Prevention and Control: Use of Primary Health Care Approach,” Indian J. Community Med. Off. Publ. Indian Assoc. Prev. Soc. Med, vol. 36, no. Suppl1, pp. S67–S71, Dec. 2011, https://doi.org/10.4103/0970-0218.94712.
“World Health Organization Regional Office for the Western. Global status report on noncommunicable diseases 2010 [Internet]. Geneva: World Health Organization. ; 2011 p. 164. Report No.: ISBN 978 92 4 068645 8. Available from: https://www.who.int/nmh/publications/ncd_report_full_en.pdf”.
Sivanantham P, Sahoo J, Lakshminarayanan S, Bobby Z, Kar SS. Profile of risk factors for non-communicable Diseases (NCDs) in a highly urbanized district of India: findings from Puducherry district-wide STEPS Survey, 2019-20. PLoS ONE. 2021;16(1):e0245254. https://doi.org/10.1371/journal.pone.0245254.
Census of India., “Puducherry (Pondicherry) District Population Census 2011–2020, Puducherry literacy sex ratio and density,” Population Census 2011, 2011. https://www.census2011.co.in/census/district/482-puducherry.html (accessed May 26, 2020).
Metcalfe C, “Biostatistics: A Foundation for Analysis in the Health Sciences. 7th edn. Wayne W. Daniel, Wiley. 1999. No. of. pages: xiv + 755 + appendices. Price: £28.95. ISBN 0-471-16386-4,” Stat. Med, vol. 20, no. 2, pp. 324–326, 2001, https://doi.org/10.1002/1097-0258(20010130)20:2<324::AID-SIM635>3.0.CO;2-O.
Organization WH, “WHO STEPS Surveillance Manual. : STEPwise Approach to Non Communicable Disease risk factors surveillance,” World Health Organization, Geneva, Jan. 2017. Accessed: Feb. 12, 2019. [Online]. Available: http://www.who.int/ncds/surveillance/steps/en/.
Thakur JS, et al. Non-communicable diseases risk factors and their determinants: a cross-sectional state-wide STEPS survey, Haryana, North India. PLoS ONE. 2019;14(11):e0208872. https://doi.org/10.1371/journal.pone.0208872.
Thakur JS, et al. Non-communicable diseases risk factors and their determinants: a cross-sectional state-wide STEPS survey, Haryana, North India. PLoS ONE. Nov. 2019;14(11):e0208872. https://doi.org/10.1371/journal.pone.0208872.
Tripathy JP, Thakur JS, Jeet G, Chawla S, Jain S, Prasad R. Urban rural differences in diet, physical activity and obesity in India: are we witnessing the great indian equalisation? Results from a cross-sectional STEPS survey. BMC Public Health. 18 2016;16(1):816. https://doi.org/10.1186/s12889-016-3489-8.
Patel SA, et al. Chronic disease concordance within indian households: a cross-sectional study. PLOS Med. Sep. 2017;14(9):e1002395. https://doi.org/10.1371/journal.pmed.1002395.
Sarma PS, et al. Prevalence of risk factors of non-communicable diseases in Kerala, India: results of a cross-sectional study. BMJ Open. Nov. 2019;9(11):e027880. https://doi.org/10.1136/bmjopen-2018-027880.
Sarveswaran G, Kulothungan V, Mathur P. “Clustering of noncommunicable disease risk factors among adults (18–69 years) in rural population, South-India,” Diabetes Metab. Syndr, vol. 14, no. 5, pp. 1005–1014, Oct. 2020, https://doi.org/10.1016/j.dsx.2020.05.042.
“Ministry of Health and Family Welfare. National multisectoral action plan for prevention and control of common noncommunicable diseases (2017–2022) [Internet]. New Delhi: Ministry of Health and Family Welfare; 2017 Oct [cited 2020 Jun 5] p. 52. Available from: https://main.mohfw.gov.in/sites/default/files/National%20Multisectoral%20Action%20Plan%20%28NMAP%29%20for%20Prevention%20and%20Control%20of%20Common%20NCDs%20%282017-22%29_1.pdf”.
Yadav K, Krishnan A. “Changing patterns of diet, physical activity and obesity among urban, rural and slum populations in north India,” Obes. Rev. Off. J. Int. Assoc. Study Obes, vol. 9, no. 5, pp. 400–408, Sep. 2008, https://doi.org/10.1111/j.1467-789X.2008.00505.x.
Armstrong T, Bull F. “Development of the World Health Organization Global Physical Activity Questionnaire (GPAQ),” J. Public Health, vol. 14, no. 2, pp. 66–70, Apr. 2006, https://doi.org/10.1007/s10389-006-0024-x.
Funding
Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER) institute, India [Grant Number: JIP/Dean (R)/Intramural/Phs 1/2019-20] has funded this project through the intramural funding for Ph.D. studies.
Author information
Authors and Affiliations
Contributions
PS, JPS, SL, ZB, JA and SSK conceptualized the study design and methodology. PS conducted the field data collection. All authors contributed to the analysis plan of the manuscript, and PS carried out the analysis. PS wrote the first draft of the manuscript with inputs from SKK and JPS. All authors reviewed the manuscript, provided information for data interpretation, and approved its final version.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Ethics Committee of institute ‘Jawaharlal Institute of Postgraduate Medical Education and Research’ (No: JIP/IEC/2018/0246).
Consent for publication
Not applicable.
Competing interests
We declare no competing interests.
Data sharing
The data underlying this manuscript could be shared by the corresponding author upon reasonable request (email: drsitanshukar@gmail.com).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sivanantham, P., Sahoo, J.P., Lakshminarayanan, S. et al. Prevalence of clustering of non-communicable disease risk factors in a highly urbanized district of India: findings of a cross-sectional survey in Puducherry. J Diabetes Metab Disord (2023). https://doi.org/10.1007/s40200-023-01318-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40200-023-01318-x