Abstract
Background
Cardiovascular diseases are the first leading cause of mortality in the world. Practical guidelines recommend an accurate estimation of the risk of these events for effective treatment and care. The UK Prospective Diabetes Study (UKPDS) has a risk engine for predicting CHD risk in patients with type 2 diabetes, but in some countries, it has been shown that the risk of CHD is poorly estimated. Hence, we assessed the external validity of the UKPDS risk engine in patients with type 2 diabetes identified in the national diabetes program in Iran.
Methods
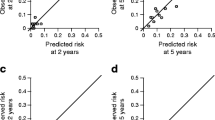
The cohort included 853 patients with type 2diabetes identified between March 21, 2007, and March 20, 2018 in Lorestan province of Iran. Patients were followed for the incidence of CHD. The performance of the models was assessed in terms of discrimination and calibration. Discrimination was examined using the c-statistic and calibration was assessed with the Hosmer–Lemeshow χ2 statistic (HLχ2) test and a calibration plot was depicted to show the predicted risks versus observed ones.
Results
During 7464.5 person-years of follow-up 170 first Coronary heart disease occurred. The median follow-up was 8.6 years. The UKPDS risk engine showed moderate discrimination for CHD (c-statistic was 0.72 for 10-year risk) and the calibration of the UKPDS risk engine was poor (HLχ2 = 69.9, p < 0.001) and the UKPDS risk engine78% overestimated the risk of heart disease in patients with type 2 diabetes identified in the national diabetes program in Iran.
Conclusion
This study shows that the ability of the UKPDS Risk Engine to discriminate patients who developed CHD events from those who did not; was moderate and the ability of the risk prediction model to accurately predict the absolute risk of CHD (calibration) was poor and it overestimated the CHD risk. To improve the prediction of CHD in patients with type 2 diabetes, this model should be updated in the Iranian diabetic population.

Similar content being viewed by others
Data Availability
The data is available on request from the authors.
Abbreviations
- AUROC:
-
Area Under the Receiver Operating Characteristic
- BMI:
-
Body mass index
- CVD:
-
Cardiovascular Disease
- DCCT:
-
Diabetes Control and Complications Trial
- DM:
-
Diabetes Mellitus
- EPIC-Norfolk:
-
(European Prospective Investigation into Cancer) Norfolk study
- FRS:
-
Framingham Risk Score Model
- HbA1C:
-
Glycated hemoglobin A
- HDL:
-
High-density lipoproteins
- LDL:
-
low-density lipoprotein) cholesterol
- ROC:
-
Receiver Operating Characteristic
- SCORE:
-
Systematic Coronary Risk Evaluation
- SD:
-
Standard Deviation
- UKPDS:
-
UK Prospective Diabetes Study
References
Countdown, N., 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4 Lancet, 2018. 392(10152): p. 1072-88.
Bennett, J.E., et al., NCD countdown 2030: worldwide trends in non-communicable disease mortality and progress towards sustainable development goal target 3.4. The Lancet, 2018. 392(10152): p. 1072–1088.
Manemann, S.M., et al., Recent trends in cardiovascular disease deaths: a state specific perspective. BMC Public Health, 2021. 21(1): p. 1–7.
Sun, H., et al., IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045 Diabetes research and clinical practice, 2022. 183: p. 109119.
Roth, G.A., et al., Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. Journal of the American College of Cardiology, 2020. 76(25): p. 2982–3021.
Hajar, R., Framingham contribution to cardiovascular disease. Heart views: the official journal of the Gulf Heart Association, 2016. 17(2): p. 78.
Al-Mawali, A., Non-communicable diseases: shining a light on cardiovascular disease, Oman’s biggest killer. Oman medical journal, 2015. 30(4): p. 227.
Olaniyi, E.O., et al. Neural network diagnosis of heart disease. in 2015 International Conference on Advances in Biomedical Engineering (ICABME). 2015. IEEE.
Pyakurel, P., et al., Cardiovascular risk factors among industrial workers: a cross–sectional study from eastern Nepal. Journal of Occupational Medicine and Toxicology, 2016. 11(1): p. 1–7.
Yang, W., et al., Comparison between metabolic syndrome and the framingham risk score as predictors of cardiovascular diseases among Kazakhs in Xinjiang. Scientific reports, 2018. 8(1): p. 1–8.
Malahfji, M. and J.J. Mahmarian, Imaging to stratify coronary artery disease risk in asymptomatic patients with diabetes. Methodist DeBakey cardiovascular journal, 2018. 14(4): p. 266.
Xu, G., et al., Risk of all-cause and CHD mortality in women versus men with type 2 diabetes: a systematic review and meta-analysis. European journal of endocrinology, 2019. 180(4): p. 243–255.
Hadaegh, F., et al., New and known type 2 diabetes as coronary heart disease equivalent: results from 7.6 year follow up in a Middle East population. Cardiovascular diabetology, 2010. 9(1): p. 1–8.
Lloyd-Jones, D.M., et al., Framingham risk score and prediction of lifetime risk for coronary heart disease. The American journal of cardiology, 2004. 94(1): p. 20–24.
Hense, H.-W., et al., Evaluation of a recalibrated systematic coronary risk evaluation cardiovascular risk chart: results from systematic coronary risk evaluation Germany. European Journal of Preventive Cardiology, 2008. 15(4): p. 409–415.
Coleman, R.L., et al., Framingham, SCORE, and DECODE risk equations do not provide reliable cardiovascular risk estimates in type 2 diabetes. Diabetes care, 2007. 30(5): p. 1292–1293.
Stevens, R.J., et al., The UKPDS risk engine: a model for the risk of coronary heart disease in type II diabetes (UKPDS 56). Clinical science, 2001. 101(6): p. 671–679.
Bannister, C.A., et al., External validation of the UKPDS risk engine in incident type 2 diabetes: a need for new type 2 diabetes–specific risk equations. Diabetes care, 2014. 37(2): p. 537–545.
Laxy, M., et al., Performance of the UKPDS outcomes model 2 for predicting death and cardiovascular events in patients with type 2 diabetes mellitus from a german population-based cohort. Pharmacoeconomics, 2019. 37(12): p. 1485–1494.
McEwan, P., et al., Validation of the UKPDS 82 risk equations within the Cardiff Diabetes Model. Cost effectiveness and resource allocation, 2015. 13(1): p. 1–7.
Ezenwaka, C., et al., Prediction of 10-year coronary heart disease risk in caribbean type 2 diabetic patients using the UKPDS risk engine. International journal of cardiology, 2009. 132(3): p. 348–353.
Clarke, P., et al., A model to estimate the lifetime health outcomes of patients with type 2 diabetes: the United Kingdom prospective diabetes study (UKPDS) Outcomes Model (UKPDS no. 68). Diabetologia, 2004. 47(10): p. 1747–1759.
Van Dieren, S., et al., External validation of the UK prospective diabetes study (UKPDS) risk engine in patients with type 2 diabetes. Diabetologia, 2011. 54(2): p. 264–270.
Marshall SM, B.J., Standardization of HbA1c measurements: a consensus statement. Annals of clinical biochemistry, 2000. 1(1): p. 45–6.
Koo, B.K., et al., Prediction of coronary heart disease risk in korean patients with diabetes mellitus. J Lipid Atheroscler, 2018. 7(2): p. 110.
Yew, S.Q., Y.C. Chia, and M. Theodorakis, Assessing 10-Year Cardiovascular Disease Risk in Malaysians with type 2 diabetes Mellitus: Framingham Cardiovascular Versus United Kingdom prospective diabetes study equations. Asia Pacific Journal of Public Health, 2019. 31(7): p. 622–632.
Yang, X., et al., Development and validation of a total coronary heart disease risk score in type 2 diabetes mellitus. The American journal of cardiology, 2008. 101(5): p. 596–601.
Simmons, R.K., et al., Performance of the UK prospective diabetes study risk engine and the Framingham risk equations in estimating cardiovascular disease in the EPIC-Norfolk cohort. Diabetes care, 2009. 32(4): p. 708–713.
Piniés, J.A., et al., Development of a prediction model for fatal and non-fatal coronary heart disease and cardiovascular disease in patients with newly diagnosed type 2 diabetes mellitus: the basque country prospective complications and Mortality Study risk engine (BASCORE). Diabetologia, 2014. 57(11): p. 2324–2333.
Acknowledgements
We thank all health care professionals in Lorestan province who helped to carry out this study.
Funding
This work was supported from Iran University of Medical Sceinces ( Nunmber-96-01-27-30511).
Author information
Authors and Affiliations
Contributions
MV, HRB, DK, SAM: conception or design of the work. MV, DK, HRB data collection, data analysis and interpretation, drafting the article,. MEK, SAM and MSD interpretation and critical revision of the article, final approval of the version to be published. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethics institutional review board of Iran University of Medical Sceinces for studies in the community. It was exempted from signing informed consent forms.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Valipour, M., Khalili, D., Solaymani-Dodaran, M. et al. External validation of the UK prospective diabetes study (UKPDS) risk engine in patients with type 2 diabetes identified in the national diabetes program in Iran. J Diabetes Metab Disord 22, 1145–1150 (2023). https://doi.org/10.1007/s40200-023-01224-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-023-01224-2