Abstract
Background
Polycythemia has been reported to be associated with cardiometabolic risk factors. However, it remains to be determined whether age affects their associations.
Methods
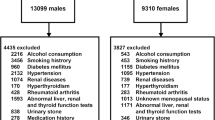
The subjects were 11,261 men at ages of 30 ~ 65 years who had received annual health checkup examinations. They were divided by age into four groups of 30 ~ 39, 40 ~ 49, 50 ~ 59 and 60 ~ 65 years. Variables related to polycythemia and cardiometabolic risk and their associations were compared in the different age groups.
Results
The prevalences of polycythemia and metabolic syndrome tended to be lower and higher, respectively, with an increase of age. Odds ratios (ORs) of subjects with vs. subjects without polycythemia for high LDL-C/HDL-C ratio and metabolic syndrome were significantly high in the age group of 30 ~ 39 years when compared with the reference level (OR with 95% confidence interval: 3.21 [2.35 ~ 4.37] [high LDL-C/HDL-C ratio] and 3.49 [2.38 ~ 5.12] [metabolic syndrome]) and tended to be lower with an increase of age (60 ~ 65 years, OR with 95% confidence interval: 1.36 [0.63 ~ 2.93] [high LDL-C/HDL-C ratio] and 1.88 [1.16 ~ 3.03] [metabolic syndrome]).
Conclusion
The prevalence of polycythemia was higher and its associations with cardiometabolic risk such as high LDL-C/HDL-C ratio and metabolic syndrome were stronger in the youngest group than in the older groups. The results suggest that early detection and correction of polycythemia are more effective than its later correction for prevention of cardiovascular disease in middle-aged men.
Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author (IW) upon reasonable request.
Code Availability
Not applicable.
References
Cinar Y, Demir G, Paç M, Cinar AB. Effect of hematocrit on blood pressure via hyperviscosity. Am J Hypertens. 1999;12:739–43.
Malek AM, Alper SL, Izumo S. Hemodynamic shear stress and its role in atherosclerosis. J Am Med Assoc. 1999;282:2035–42.
Wakabayashi I. Associations between polycythemia and cardiometabolic risk factors in middle-aged men. Clin Chim Acta. 2022;531:248–53.
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127:2391–405.
Moulard O, Mehta J, Fryzek J, Olivares R, Iqbal U, Mesa RA. Epidemiology of myelofibrosis, essential thrombocythemia, and polycythemia vera in the European Union. Eur J Haematol. 2014;92:289–97.
Mehta J, Wang H, Iqbal SU, Mesa R. Epidemiology of myeloproliferative neoplasms in the United States. Leuk Lymphoma. 2014;55:595–600.
Souresho H, Mgerian M, Havican S, Suniega E, Gambrill C. A practical approach to polycythemia in the outpatient setting and its importance. Cureus. 2021;13:e19368.
Lakatta EG, Levy D. Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part I: aging arteries: a “set up” for vascular disease. Circulation. 2003;107:139–46.
Sniderman AD, Furberg CD. Age as a modifiable risk factor for cardiovascular disease. Lancet. 2008;371(9623):1547–9.
Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al, American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2020 update: A report from the American Heart Association. Circulation. 2020;141:e139–596.
Cheng S, Xanthakis V, Sullivan LM, Vasan RS. Blood pressure tracking over the adult life course: patterns and correlates in the Framingham heart study. Hypertension. 2012;60:1393–9.
Jack L Jr, Boseman L, Vinicor F. Aging Americans and diabetes. A public health and clinical response. Geriatrics. 2004;59:14–7.
Wang M, Liu M, Li F, Guo C, Liu Z, Pan Y, et al. Gender heterogeneity in dyslipidemia prevalence, trends with age and associated factors in middle age rural Chinese. Lipids Health Dis. 2020;19:135.
Wakabayashi I. Age-related change in relationship between body-mass index, serum sialic acid, and atherogenic risk factors. J Atheroscler Thromb. 1998;5:60–5.
Wakabayashi I, Daimon T. Age-dependent decline of association between obesity and hyperglycemia in men and women. Diabetes Care. 2012;35:175–7.
Wakabayashi I. Influence of age and gender on triglycerides-to-HDL-cholesterol ratio (TG/HDL ratio) and its association with adiposity index. Arch Gerontol Geriatr. 2012;55:729–34.
Wakabayashi I. Relationships of body mass index with blood pressure and serum cholesterol concentrations at different ages. Aging Clin Exp Res. 2004;16:461–6.
Kannel WB. Lipids, diabetes, and coronary heart disease: insights from the Framingham Study. Am Heart J. 1985;110:1100–7.
Wakabayashi I, Daimon T. The “cardiometabolic index” as a new marker determined by adiposity and blood lipids for discrimination of diabetes mellitus. Clin Chim Acta. 2015;438:274–8.
Anonymous. Metabolic Syndrome-Definition and Diagnostic Criteria in Japan. J Jpn Soc Intern Med. 2005;94:794–809. (in Japanese).
Kashiwagi A, Kasuga M, Araki E, Oka Y, Hanafusa T, Ito H, et al, Committee on the Standardization of Diabetes Mellitus - Related Laboratory Testing of Japan Diabetes Society. International clinical harmonization of glycated hemoglobin in Japan: From Japan Diabetes Society to National Glycohemoglobin Standardization Program values. J Diabetes Investig. 2012;3:39–40.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al.; International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009; 120: 1640–45.
Hsieh SD, Muto T. Metabolic syndrome in Japanese men and women with special reference to the anthropometric criteria for the assessment of obesity: Proposal to use the waist-to-height ratio. Prev Med. 2006;42:135–9.
Flack JM, Adekola B. Blood pressure and the new ACC/AHA hypertension guidelines. Trends Cardiovasc Med. 2020;30:160–4.
Teramoto T, Sasaki J, Ishibashi S, Birou S, Daida H, Dohi S, et al. Japan Atherosclerosis Society. Executive summary of the Japan Atherosclerosis Society (JAS) guidelines for the diagnosis and prevention of atherosclerotic cardiovascular diseases in Japan – 2012 version. J Atheroscler Thromb. 2013;20:517–23.
Anonimous, American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):62–9.
Wouters HJCM, Mulder R, van Zeventer IA, Schuringa JJ, van der Klauw MM, van der Harst P, et al. Erythrocytosis in the general population: clinical characteristics and association with clonal hematopoiesis. Blood Adv. 2020;4:6353–63.
Craig WY, Palomaki GE, Haddow JE. Cigarette smoking and serum lipid and lipoprotein concentrations: an analysis of published data. BMJ. 1989;298:784–8.
Drager LF, Togeiro SM, Polotsky VY, Lorenzi-Filho G. Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol. 2013;62:569–76.
Sasaki Y, Ikeda Y, Miyauchi T, Uchikado Y, Akasaki Y, Ohishi M. Estrogen-SIRT1 axis plays a pivotal role in protecting arteries against menopause-induced senescence and atherosclerosis. J Atheroscler Thromb. 2020;27:47–59.
Funding
This work was supported by the Grant-in-Aid for Scientific Research (No. 21H03386) from the Japan Society for the Promotion of Science.
Author information
Authors and Affiliations
Contributions
Conceptualization, analysis, writing, and visualization, IW.
Corresponding author
Ethics declarations
Conflict of interest
The author declares no conflict of interest.
Ethical approval
The database used in this study was supplied from a local health checkup system without individual identification, and no informed consent was obtained from each subject. This study was approved by the Ethics Committee of Yamagata University School of Medicine (No. 112 from April 2005 to March 2006, approved on March 13, 2006) and the Hyogo College of Medicine Ethics Committee (No. 3003 in 2020).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wakabayashi, I. Effects of age on polycythemia, cardiometabolic risk and their associations in middle-aged men. J Diabetes Metab Disord 22, 287–295 (2023). https://doi.org/10.1007/s40200-022-01130-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-022-01130-z