Abstract
Purpose of Review
To find the best anesthesia practices for patients with aerodigestive disorders undergoing triple endoscopy.
Recent Findings
While there is abundant literature on the utility of aerodigestive programs as well as the triple endoscopy performed in aerodigestive patients, there is a lack of studies investigating the optimal anesthetic technique for this patient population.
Summary
Triple endoscopy has been shown to expedite diagnosis and treatment while exposing patients to less anesthesia and decreasing the frequency of unnecessary evaluations. Due to the high-risk nature of airway procedures and the frequent underlying comorbidities in this special patient population, perioperative respiratory complications are common. Collaborative, multidisciplinary care among anesthesiologists, otolaryngologists, pulmonologists, and gastroenterologists is essential to meet the specific needs of each aerodigestive patient and safely perform the triple endoscopy. This article outlines our anesthetic approach and the perioperative considerations taken for each stage of the process.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aerodigestive disorders include a variety of conditions affecting the respiratory and digestive systems and commonly manifest with difficulty swallowing and/or feeding, gastroesophageal reflux disease, failure to thrive, recurrent pneumonia, stridor, shortness of breath, and chronic cough. According to a consensus statement by Boesch et al., aerodigestive patients are children with a combination of multiple and interrelated congenital and/or acquired conditions affecting airway, breathing, feeding, swallowing, or growth that require a coordinated interdisciplinary diagnostic and therapeutic approach to achieve optimal outcomes [1]. Aerodigestive programs have been emerging in many parts of the USA since the 1990s, with the largest subset in children’s academic centers [2, 3]. The aerodigestive program at Children’s Hospital Los Angeles (CHLA) was launched in 2016, to address the needs of children with these disorders in Southern California. Table 1 illustrates the commonly seen conditions in aerodigestive clinics at various centers.
Patients are initially evaluated by specialists from otolaryngology (ENT), pulmonology, and gastroenterology to develop a comprehensive plan of care in the clinic. Dedicated specialists from pediatric surgery, anesthesiology, speech, and language pathology as well as a registered dietitian are also available for consultation during the same visit. Patients who require further evaluation with a direct assessment of the aerodigestive tract are offered a triple endoscopy in the operating room which consists of a flexible bronchoscopy and bronchoalveolar lavage (BAL) performed by a pulmonologist, rigid laryngoscopy and bronchoscopy by an otolaryngologist, and upper gastrointestinal (GI) endoscopy with biopsies performed by a gastroenterologist, all under one general anesthetic. We conducted a literature search to review the best anesthetic practices to care for aerodigestive patients undergoing triple endoscopy.
Methods
PubMed, EMBASE, Google Scholar, and Cochrane databases were searched using the keywords: anesthesia, aerodigestive, aero-digestive, triple scope, and triple endoscopy from July 2002 to July 2022. To be included, articles had to be human studies, in the English language, and concentrate on the anesthetic considerations for aerodigestive patients undergoing triple endoscopy. Two independent reviewers (AK and JY) screened articles for inclusion, and any uncertainties or disagreements were resolved via discussion.
Results
After an extensive search, we did not find any other articles meeting the inclusion criteria other than our previously published article on perioperative respiratory adverse events (PRAE) in aerodigestive patients [4••]. While there were studies describing the utility and feasibility of the multidisciplinary approach of aerodigestive clinics and triple endoscopy, there were no published studies on best practices for anesthesia for triple endoscopy or studies describing outcomes other than PRAE.
Anesthesia Implications of Triple Endoscopy
Due to frequent underlying respiratory comorbidities and the high-risk nature of airway procedures, intraoperative complications are not uncommon. Among pediatric patients undergoing elective bronchoscopies, perioperative respiratory complications have been previously reported in 33% of patients [5]. This study also demonstrated that patients with complex syndromes and cardiac comorbidities experienced a higher rate of severe complications.
In our 2019 review of triple endoscopies in aerodigestive patients (n = 122), 57% of the patients were noted to have at least one perioperative respiratory adverse event (PRAE) which included oxygen desaturation less than 90% that lasted longer than 1 min, any severe oxygen desaturation (< 70%) for any length of time, bronchospasm, laryngospasm, or escalation in the level of respiratory support compared to baseline [4••]. Other than the male sex, patient characteristics such as age, weight, body mass index, and comorbidities including preexisting lung disease were not statistically significant for increased risk of PRAE. Procedure-specific risk factors such as the experience level of the anesthesiologist, anesthetic technique (induction and maintenance of anesthesia), and adjunct medications (i.e., opioids and ketamine) used were also not statistically significant. There was no statistically significant difference in the incidence of perioperative respiratory events between those children who had an illness at the time of surgery, those who had an illness up to 4 weeks before surgery, and those who did not have an illness. However, there was a higher incidence of patients with respiratory illness, particularly those with symptoms at the time of surgery, ultimately having a respiratory adverse event. Due to the high risk of respiratory complications, triple endoscopy in aerodigestive patients warrants a high degree of vigilance, planning, and communication with all team members.
Aerodigestive Anesthesiology Protocol
There is limited literature describing anesthesia protocols for triple endoscopy; however, the principles for performing anesthesia during dynamic upper airway evaluation (i.e., drug-induced sleep endoscopy) and distal airway evaluations generally apply [6, 7]. The following perioperative outline summarizes what we find to be a rational approach to providing anesthesia in these cases. As the clinical presentation can vary, adjustments are made based on the anesthesiologist’s experience and clinical assessment along with the patient’s specific needs and comorbidities.
Preoperative
Given the high incidence of pulmonary comorbidities in aerodigestive patients, special attention is given to evaluating the patient’s pulmonary status before and on the day of surgery. Premedication with albuterol has been suggested to decrease PRAE in children undergoing airway surgery, although the utility of this practice remains mixed in the literature [5, 8]. Patients with a cough, reactive airway disease, or wheezing on exam receive albuterol in the preoperative area if they had not already received treatment on the morning of surgery. Patients prescribed inhaled corticosteroids are encouraged to continue these perioperatively. Premedication with oral midazolam up to 0.5 mg/kg is commonly used to reduce anxiety unless there are concerns for obstructive sleep apnea (OSA), in which case intravenous (IV) or intranasal dexmedetomidine may be substituted.
Intraoperative
The primary anesthetic goal during flexible and rigid bronchoscopy is to maintain spontaneous ventilation while achieving an adequate depth of anesthesia to avoid unwanted coughing and movement. This balance can prove challenging; therefore, patience and open communication between aerodigestive team members are crucial for preoperative planning, intraoperative execution, and post-operative care, especially since the airway is shared among specialties in a confined space. While definitive data on the agent of choice is lacking, volatile anesthetics and IV anesthetics such as propofol, remifentanil, dexmedetomidine, and ketamine have all been utilized in sleep endoscopies [9].
Induction
Mask or IV induction is performed at the discretion of the anesthesiologist; however, mask induction is more commonly done given the young age of these patients. Inhalational induction is typically done with sevoflurane, and the addition of nitrous oxide is decided by weighing the benefit of speeding up induction versus the risk of decreasing the oxygen concentration. If IV induction is performed, then propofol 2–4 mg/kg is administered as needed. Anesthesia is maintained with a propofol infusion starting at 200–300 mcg/kg/min, and this is titrated to a dose to maintain an adequate plane of anesthesia to safely allow for airway evaluation while preserving spontaneous ventilation. At this stage, inhaled anesthetics are often avoided due to operating room contamination and the inability to maintain a steady state. Supplemental agents such as ketamine 0.5–1 mg/kg and dexmedetomidine 0.5–1 mcg/kg can be administered as intravenous boluses, as needed. Low-dose remifentanil infusion at 0.05 mcg/kg/min has also been used successfully at other institutions. Dexamethasone 0.5 mg/kg IV (maximum dose 10 mg) is given prophylactically to prevent airway edema. Topicalization of the airway with aerosolized lidocaine without epinephrine, up to 5 mg/kg, can be effective in reducing anesthetic requirements.
We recommend avoiding opioids such as fentanyl during induction as well as maintenance, as it has been shown that under inhalational anesthesia, administration of fentanyl 0.5 mcg/kg may lead to apnea in 5% of patients without OSA and in 46% of patients with OSA [10].
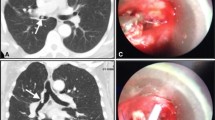
Flexible Bronchoscopy With or Without BAL
During flexible bronchoscopy, the pulmonologist passes an endoscope via the nares to assess the nasopharynx, oropharynx, larynx, and trachea. BAL is then performed as indicated [9]. The pulmonologist first assesses the airway dynamics of the upper airway and observes for any abnormalities like upper airway collapse, laryngomalacia, tracheomalacia, and abnormalities of the vocal cords. Evaluating the airway dynamics in a state that resembles sleep is important in the diagnostic workup; therefore, our pulmonologists prefer the patient to be at a lighter anesthetic plane if deemed safe by the anesthesiologist [11]. A lighter plane will allow for coughing that may reveal a diagnosis of dynamic tracheomalacia.
After evaluating upper airway dynamics, the depth of anesthesia is increased for evaluation of the lower airway anatomy. For this portion of the procedure, a natural airway is maintained and supplemented with a traditional low-flow nasal cannula, as it allows for ETCO2 monitoring without additional equipment. However, a traditional nasal cannula can only effectively provide only up to 4 to 6 l per minute of supplemental oxygen which equates to a FiO2 of approximately 0.37 to 0.45. Higher flows can lead to the drying of the nasal mucosa and an increased potential for bleeding. As an alternative, a high-flow nasal cannula (HFNC) such as transnasal humidified rapid-insufflation ventilatory exchange (THRIVE) can deliver up to 100% humidified and heated oxygen at a flow rate of up to 60 l per minute and has been shown to extend the apneic time and improve upper airway patency in pediatric patients undergoing sleep endoscopy [12, 13].
Upper airway obstruction commonly occurs during the evaluation of the lower airway anatomy. Due to the larger occiput in pediatric patients, overextending the neck may worsen airway obstruction, especially in the presence of tracheomalacia. A combination of head tilt-chin lift or jaw-thrust maneuvers may be helpful in selected cases to relieve obstruction from a large floppy tongue. As an initial step, an oropharyngeal or nasopharyngeal airway (NPA) can be utilized to assist with oxygenation and ventilation until the airway obstruction improves by titrating the level of anesthesia. These airway adjuncts also serve as a bridge to more advanced airway placement like a laryngeal mask airway (LMA) or endotracheal tube (ETT), if clinically indicated. A modified NPA can also be used to relieve the upper airway obstruction and allow for end-tidal carbon dioxide (ETCO2) sampling. This is easily achieved by inserting a 15-mm plastic adapter from an appropriately sized ETT into an NPA, which can then be connected to the circuit (Fig. 1). The NPA may need to be withdrawn if it obscures the view during the bronchoscopy.
Rigid Laryngoscopy and Bronchoscopy
Rigid bronchoscopy is considered the gold standard for diagnostic airway assessment of structures below the vocal cords, including the trachea and bronchi. It offers the ability to measure the size of areas of narrowing and provides an opportunity to perform a variety of interventions such as biopsy, laryngeal cleft injection or suturing, supraglottoplasty, balloon dilation, vocal cord injection, and laryngotracheal reconstruction [14, 15]. The anesthetic goal for this portion is to preserve spontaneous ventilation while maintaining a level of anesthesia deep enough to avoid movement during laryngoscopy or bronchoscopy. Supplemental oxygen can be provided through an ETT placed in the oropharynx by ENT or by ventilating through the side port of the rigid bronchoscope.
Bronchoscopy whether rigid or flexible yields information based on anesthesia level. Close communication between the anesthesiologist and bronchoscopist is important not just for patient safety but also to obtain a valuable and meaningful evaluation [6, 11].
Upper Gastrointestinal Endoscopy
The gastroenterologist’s evaluation and assessment of the esophagus, stomach, and duodenum for any anatomical or mucosal abnormality is a vital step in aerodigestive assessment [16]. For this part of the procedure, the airway can be managed with a natural airway, LMA, or ETT at the discretion of the anesthesiologist, patient’s comorbidities, and intraoperative course. After completion of the upper endoscopy, the gastroenterologist will confirm the evacuation of any gastric contents such as air and secretions.
Postoperative
Parents are informed in advance that patients may take longer (up to 2 h) to fully emerge from anesthesia in the post-anesthesia care unit (PACU). This is due to the context-sensitive half-time of agents typically used. There are currently no evidence-based guidelines for overnight admission criteria specific to the aerodigestive population. Many patients can be discharged home; however, overnight admissions are indicated in a subset of patients. At our institution, we follow the post-operative admission indications used for patients undergoing airway surgeries. Patients are admitted if they have severe OSA or obesity with OSA symptoms (Fig. 2), a history of significant cardiovascular disease, multiple episodes of apnea or hypoxia in the perioperative period, or an inability to return to respiratory baseline in the postoperative period. Overall, 9% of aerodigestive patients undergoing triple endoscopy at our institution required ICU admission postoperatively, of which the majority (78%) were planned admissions due to the medical complexity of the patient. Patients with recent or frequent respiratory illness who undergo triple endoscopy are at higher risk for respiratory complications and are admitted overnight for observation. The final disposition eventually depends on their perioperative course.
Discussion
Triple endoscopy has been described to expedite diagnosis and treatment for patients with symptoms such as chronic cough, obstruction, or aspiration. The multidisciplinary approach allows several specialists to discuss and make treatment plans on real-time findings during the procedures [16]. In 2019, Fracchia et al. reported that of the children who underwent triple endoscopy for chronic cough, 83% had at least one positive finding and 41% had more than one specialty-specific finding that would have not been found with a single procedure [8]. This has been shown to decrease the frequency of unnecessary evaluation and exposure to anesthesia. Ruiz et al. found that the average anesthesia time for a triple endoscopy was significantly less than the estimated time of having all three procedures done separately [17••]. In addition, multiple studies have shown there have been significant cost reductions for the patients and their families with an integrated aerodigestive approach, compared to when patients had to see individual specialists sequentially. Overall, this approach led to high family satisfaction [8, 15, 17••,18,19,20].
Conclusion
Aerodigestive programs have shown that the multidisciplinary approach to taking care of these patients provides many advantages over the fragmented approach of individual evaluations by isolated specialists. Anesthesiologists care for the subset of aerodigestive patients who come to the operating room for triple endoscopy. Given the high incidence of PRAEs associated with this procedure, a thorough preoperative assessment and an individualized anesthetic plan are needed for these complex patients. This article outlines a common sequence of events during a triple endoscopy and one rational anesthetic approach. We found that there were no articles that specifically investigated the best practice for anesthetic management of aerodigestive patients undergoing triple endoscopy. More research is needed for a consensus on anesthetic management for this patient population.
Data Availability
The data that support the findings of this study are available from the corresponding author, [AK], upon reasonable request.
References
Papers of particular interest, published recently, have been highlighted as:•• Of major importance
Boesch RP, Balakrishnan K, Acra S, et al. Structure and functions of pediatric aerodigestive programs: a consensus statement. Pediatrics. 2018;141(3). https://doi.org/10.1542/peds.2017-1701.
Gumer L, Rosen R, Gold BD, et al. Size and prevalence of pediatric aerodigestive programs in 2017. J Pediatr Gastroenterol Nutr. 2019;68(5):e72–6. https://doi.org/10.1097/MPG.0000000000002268.
Gendler Y, Seguier-Lipszyc E, Silbermintz A, et al. Aerodigestive Clinics as Emerging Pediatric Care Model: The First 100 Patients in Israel. Isr Med Assoc J. 2021;23(9):569–75.
Sanders K, Osterbauer B, Forman N, et al. Perioperative respiratory adverse events in children undergoing triple endoscopy. Paediatr Anaesth. 2021;31(12):1290–7. https://doi.org/10.1111/pan.14285. This was a retrospective study of aerodigestive pediatric patients who underwent triple endoscopy that found that the incidence of perioperative respiratory adverse events was 57% higher in aerodigestive patients compared to the general pediatric surgical population. Only male gender was found to be an independent risk factor associated with these events..
Carlens J, Fuge J, Price T, et al. Complications and risk factors in pediatric bronchoscopy in a tertiary pediatric respiratory center. Pediatr Pulmonol. 2018;53(5):619–27. https://doi.org/10.1002/ppul.23957.
Londino AV, Jagannathan N. Anesthesia in diagnostic and therapeutic pediatric bronchoscopy. Otolaryngol Clin North Am. 2019;52(6):1037–48. https://doi.org/10.1016/j.otc.2019.08.005.
Benjamin B. Anesthesia for pediatric airway endoscopy. Otolaryngol Clin North Am. 2000;33(1):29–47. https://doi.org/10.1016/s0030-6665(05)70206-1.
Fracchia MS, Diercks G, Cook A, et al. The diagnostic role of triple endoscopy in pediatric patients with chronic cough. Int J Pediatr Otorhinolaryngol. 2019;116:58–61. https://doi.org/10.1016/j.ijporl.2018.10.017.
Arganbright JM, Lee JC, Weatherly RA. Pediatric drug-induced sleep endoscopy: an updated review of the literature. World J Otorhinolaryngol Head Neck Surg. 2021;7(3):221–7. https://doi.org/10.1016/j.wjorl.2021.05.002.
Waters KA, McBrien F, Stewart P, et al. Effects of OSA inhalational anesthesia, and fentanyl on the airway and ventilation of children. J Appl Physiol (1985). 2002;92(5):1987–94. https://doi.org/10.1152/japplphysiol.00619.2001.
Faro A, Wood RE, Schechter MS, et al. Official American Thoracic Society technical standards: flexible airway endoscopy in children. Am J Respir Crit Care Med. 2015;191(9):1066–80. https://doi.org/10.1164/rccm.201503-0474ST.
Okland TS, Liu GS, Caruso TJ, et al. Prospective evaluation of the safety and efficacy of THRIVE for children undergoing airway evaluation. Pediatr Qual Saf. 2020;5(5):e348. https://doi.org/10.1097/pq9.0000000000000348.
Caruso TJ, Gupta A, Sidell DR, et al. The successful application of high flow nasal oxygen during microdirect laryngoscopy and bronchoscopy in patients under 7 kg. J Clin Anesth. 2019;52:27–8. https://doi.org/10.1016/j.jclinane.2018.08.027.
Day KE, Smith NJ, Kulbersh BD. Early surgical intervention in type I laryngeal cleft. Int J Pediatr Otorhinolaryngol. 2016;90:236–40. https://doi.org/10.1016/j.ijporl.2016.09.017.
Kanotra SP, Weiner R, Rahhal R. Making the case for multidisciplinary pediatric aerodigestive programs. World J Gastroenterol. 2022;28(28):3620–6. https://doi.org/10.3748/wjg.v28.i28.3620.
Rotsides JM, Krakovsky GM, Pillai DK, et al. Is a multidisciplinary aerodigestive clinic more effective at treating recalcitrant aerodigestive complaints than a single specialist? Ann Otol Rhinol Laryngol. 2017;126(7):537–43. https://doi.org/10.1177/0003489417708579.
Ruiz AG, Bhatt JM, DeBoer EM, et al. Demonstrating the benefits of a multidisciplinary aerodigestive program. Laryngoscope. 2020;130(2):521–5. https://doi.org/10.1002/lary.27939. The Aerodigestive Program at Children’s Hospital Colorado showed that a multidisciplinary approach to taking care of aerodigestive patients led to higher family satisfaction and cost-effective care that decreased the patient’s travel time, opportunity costs, and anesthesia time.
Collaco JM, Aherrera AD, Au Yeung KJ, et al. Interdisciplinary pediatric aerodigestive care and reduction in health care costs and burden. JAMA Otolaryngol Head Neck Surg. 2015;141(2):101–5. https://doi.org/10.1001/jamaoto.2014.3057.
Mudd PA, Silva AL, Callicott SS, et al. Cost analysis of a multidisciplinary aerodigestive clinic: are such clinics financially feasible? Ann Otol Rhinol Laryngol. 2017;126(5):401–6. https://doi.org/10.1177/0003489417699420.
Garcia JA, Mistry B, Hardy S, et al. Time-driven activity-based costing to estimate cost of care at multidisciplinary aerodigestive centers. Laryngoscope. 2017;127(9):2152–8. https://doi.org/10.1002/lary.26354.
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Karnwal, A., Yoo, J., Sanders, K. et al. Anesthesia for Triple Endoscopy in Aerodigestive Patients. Curr Anesthesiol Rep 13, 159–164 (2023). https://doi.org/10.1007/s40140-023-00569-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-023-00569-x