Abstract
Purpose of the Review
Combining interventions into a multimodal prehabilitation approach is recommended to maximize benefits due to synergistic and cumulative effects of modalities. The purpose of this review was to (i) highlight the rationale for multimodal prehabilitation, (ii) summarize related contemporary literature, and (iii) discuss emerging modalities that may be combined into a comprehensive, personalized prehabilitation program.
Recent Findings
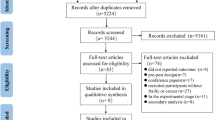
Our systematic search of multimodal prehabilitation literature over the past 5 years yielded 11 studies: five randomized controlled trials, four systematic reviews, and two meta-analyses. These studies included multimodal prehabilitation prior to major abdominal and cancer surgeries and have demonstrated benefits pre, peri-, and postoperatively. Evidence directly comparing unimodal and multimodal prehabilitation remains limited.
Summary
Multimodal prehabilitation has demonstrated benefits for patients undergoing major abdominal and cancer surgeries. Research is needed on the specific value of combining modalities, multimodal approaches in other treatment settings, and further personalization of prehabilitation to meet the unique needs of patients.

Similar content being viewed by others
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Silver JK, Baima J. Cancer prehabilitation. Am J Phys Med Rehabil. 2013. https://doi.org/10.1097/PHM.0b013e31829b4afe.
Huisman MG, Kok M, de Bock GH, van Leeuwen BL. Delivering tailored surgery to older cancer patients: preoperative geriatric assessment domains and screening tools – a systematic review of systematic reviews. Eur J Surg Oncol. 2017. https://doi.org/10.1016/j.ejso.2016.06.003.
Tang MH, Castle DJ, Choong PFM. Identifying the prevalence, trajectory, and determinants of psychological distress in extremity sarcoma. Sarcoma. 2015. https://doi.org/10.1155/2015/745163.
Hellstadius Y, Lagergren J, Zylstra J, Gossage J, Davies A, Hultman CM, et al. A longitudinal assessment of psychological distress after oesophageal cancer surgery. Acta Oncol (Madr). 2017. https://doi.org/10.1080/0284186X.2017.1287945.
Santa Mina D, van Rooijen SJ, Minnella EM, Alibhai SMH, Brahmbhatt P, Dalton SO, et al. Multiphasic prehabilitation across the cancer continuum: a narrative review and conceptual framework. Front Oncol. 2021. https://doi.org/10.3389/fonc.2020.598425.
Baldini G. Perioperative smoking and alcohol cessation. In: Enhanced recovery after surgery. Springer International Publishing; 2020. https://doi.org/10.14797/mdcj-14-2-77.
Humeidan ML, Reyes JPC, Mavarez-Martinez A, Roeth C, Nguyen CM, Sheridan E, et al. Effect of cognitive prehabilitation on the incidence of postoperative delirium among older adults undergoing major noncardiac surgery: the Neurobics Randomized Clinical Trial. JAMA Surg. 2020. https://doi.org/10.1001/jamasurg.2020.4371.
Vlisides PE, Das AR, Thompson AM, Kunkler B, Zierau M, Cantley MJ, et al. Home-based cognitive prehabilitation in older surgical patients: a feasibility study. J Neurosurg Anesthesiol. 2019. https://doi.org/10.1097/ana.0000000000000569.
Kirkham AA, Eves ND, Shave RE, Bland KA, Bovard J, Gelmon KA, et al. The effect of an aerobic exercise bout 24 h prior to each doxorubicin treatment for breast cancer on markers of cardiotoxicity and treatment symptoms: a RCT. Breast Cancer Res Treat. 2018. https://doi.org/10.1007/s10549-017-4554-4.
Kirkham AA, Shave RE, Bland KA, Bovard JM, Eves ND, Gelmon KA, et al. Protective effects of acute exercise prior to doxorubicin on cardiac function of breast cancer patients: a proof-of-concept RCT. Int J Cardiol. 2017. https://doi.org/10.1016/j.ijcard.2017.07.037.
O’Loughlin L, Lukez A, Ma Y, Baima J, Moni J. Prehabilitation for patient positioning: pelvic exercises assist in minimizing inter-fraction sacral slope variability during radiation therapy. Med Oncol. 2020.
van Haren IEPM, Staal JB, Potting CM, Atsma F, Hoogeboom TJ, Blijlevens NMA, et al. Physical exercise prior to hematopoietic stem cell transplantation: a feasibility study. Physiother Theory Pract. 2018. https://doi.org/10.1080/09593985.2018.1423655.
Rupnik E, Skerget M, Sever M, Zupan IP, Ogrinec M, Ursic B, et al. Feasibility and safety of exercise training and nutritional support prior to haematopoietic stem cell transplantation in patients with haematologic malignancies. BMC Cancer. 2020. https://doi.org/10.1186/s12885-020-07637-z.
Santa Mina D, Dolan LB, Lipton JH, Au D, Camacho Pérez E, Franzese A, et al. Exercise before, during, and after hospitalization for allogeneic hematological stem cell transplant: a feasibility randomized controlled trial. J Clin Med. 2020. https://doi.org/10.3390/jcm9061854.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009. https://doi.org/10.1136/bmj.b2700.
Higgins J, Savović J, Page M, Elbers R, Sterne J. Chapter 8: assessing risk of bias in a randomized trial. In: Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al., editors. Cochrane Handbook for Systematic Reviews of Interventions version 61. Cochrane; 2020.
Carli F, Bousquet-Dion G, Awasthi R, Elsherbini N, Liberman S, Boutros M, et al. Effect of multimodal prehabilitation vs postoperative rehabilitation on 30-day postoperative complications for frail patients undergoing resection of colorectal cancer: a randomized clinical trial. JAMA Surg. 2020. https://doi.org/10.1001/jamasurg.2019.5474.
Bousquet-Dion G, Awasthi R, Loiselle S-È, Minnella EM, Agnihotram RV, Bergdahl A, et al. Evaluation of supervised multimodal prehabilitation programme in cancer patients undergoing colorectal resection: a randomized control trial. Acta Oncol (Madr). 2018. https://doi.org/10.1080/0284186X.2017.1423180.
Huang J, Lai Y, Zhou X, Li S, Su J, Yang M, et al. Short-term high-intensity rehabilitation in radically treated lung cancer: a three-armed randomized controlled trial. J Thorac Dis. 2017. https://doi.org/10.21037/jtd.2017.06.15.
Liu Z, Qiu T, Pei L, Zhang Y, Xu L, Cui Y, et al. Two-week multimodal prehabilitation program improves perioperative functional capability in patients undergoing thoracoscopic lobectomy for lung cancer: a randomized controlled trial. Anesth Analg. 2020. https://doi.org/10.1213/ANE.0000000000004342.
• Barberan-Garcia A, Ubré M, Roca J, Lacy AM, Burgos F, Risco R, et al. Personalised prehabilitation in high-risk patients undergoing elective major abdominal surgery. Ann Surg. https://doi.org/10.1097/SLA.0000000000002293. To our knowledge, this is the first study to examine the effect of multimodal prehabilitaiton on a group of high-risk patients. The prehabilitation literature is commonly criticized for not including higher risk individuals in trials and this study provides the first data looking exclusively at that group.
Bolshinsky V, Li MH-G, Ismail H, Burbury K, Riedel B, Heriot A. Multimodal prehabilitation programs as a bundle of care in gastrointestinal cancer surgery. Dis Colon Rectum. 2018. https://doi.org/10.1097/DCR.0000000000000987.
Luther A, Gabriel J, Watson RP, Francis NK. The impact of total body prehabilitation on post-operative outcomes after major abdominal surgery: a systematic review. World J Surg. 2018. https://doi.org/10.1007/s00268-018-4569-y.
• Thomas G, Tahir MR, Bongers BC, Kallen VL, Slooter GD, van Meeteren NL. Prehabilitation before major intra-abdominal cancer surgery: a systematic review of randomised controlled trials. Eur J Anaesthesiol. 2019. https://doi.org/10.1097/EJA.0000000000001030. This review compiles data from multimodal prehabilitation studies and reports the effects of studies with high therapeutic validity compared to those with lower therapeutic validity. These data are the first to highlight the differences in outcomes between interventions that are deemed to be more versus less rigorous.
Chou Y-J, Kuo H-J, Shun S-C. Cancer prehabilitation programs and their effects on quality of life. Oncol Nurs Forum. 2018. https://doi.org/10.1188/18.ONF.726-736.
• Gillis C, Buhler K, Bresee L, Carli F, Gramlich L, Culos-Reed N, et al. Effects of nutritional prehabilitation, with and without exercise, on outcomes of patients who undergo colorectal surgery: a systematic review and meta-analysis. Gastroenterology. 2018. https://doi.org/10.1053/j.gastro.2018.05.012. This review and meta-analysis compares the effects of a unimodal (nutrition-only) versus multimodal (nutrition and exercise combined) on surgical outcomes. No RCT data to date have directly compared uni- and multimodal prehabilitation interventions.
Daniels SL, Lee MJ, George J, Kerr K, Moug S, Wilson TR, et al. Prehabilitation in elective abdominal cancer surgery in older patients: systematic review and meta-analysis. BJS Open. 2020. https://doi.org/10.1002/bjs5.50347.
Gillis C, Fenton TR, Gramlich L, Sajobi TT, Culos-Reed SN, Bousquet-Dion G, et al. Older frail prehabilitated patients who cannot attain a 400 m 6-min walking distance before colorectal surgery suffer more postoperative complications. Eur J Surg Oncol. 2020. https://doi.org/10.1016/j.ejso.2020.09.041.
• Barberan-Garcia A, Ubre M, Pascual-Argente N, Risco R, Faner J, Balust J, et al. Post-discharge impact and cost-consequence analysis of prehabilitation in high-risk patients undergoing major abdominal surgery: secondary results from a randomised controlled trial. Br J Anaesth. 2019. https://doi.org/10.1016/j.bja.2019.05.032. This study is a secondary analysis of the RCT examining the effects of multimodal prehabilitation in only high-risk patients and reports cost-effectiveness data of such an intervention.
van Rooijen S, Carli F, Dalton S, Thomas G, Bojesen R, Le Guen M, et al. Multimodal prehabilitation in colorectal cancer patients to improve functional capacity and reduce postoperative complications: the first international randomized controlled trial for multimodal prehabilitation. BMC Cancer. 2019. https://doi.org/10.1186/s12885-018-5232-6.
Santa Mina D, Sellers D, Au D, Alibhai SMH, Clarke H, Cuthbertson BH, et al. A pragmatic non-randomized trial of prehabilitation prior to cancer surgery: study protocol and COVID-19-related adaptations. Front Oncol. 2021. https://doi.org/10.3389/fonc.2021.629207.
Thomsen T, Villebro N, Møller AM. Interventions for preoperative smoking cessation. Vol. 2014, Cochrane Database of Systematic Reviews. John Wiley and Sons Ltd; 2014. https://doi.org/10.1002/14651858.CD002294.pub4.
Shabanzadeh DM, Sørensen LT. Alcohol consumption increases post-operative infection but not mortality: a systematic review and meta-analysis. Surg Infect (Larchmt). 2015. https://doi.org/10.1089/sur.2015.009.
Fadayomi AB, Ibala R, Bilotta F, Westover MB, Akeju O. A systematic review and meta-analysis examining the impact of sleep disturbance on postoperative delirium. Crit Care Med. 2018. https://doi.org/10.1097/CCM.0000000000003400.
Leung JM, Sands LP, Newman S, Meckler G, Xie Y, Gay C, et al. Preoperative sleep disruption and postoperative delirium. J Clin Sleep Med. 2015. https://doi.org/10.5664/jcsm.4944.
Wang J, Lu S, Guo L, Ren C, Zhang Z. Poor preoperative sleep quality is a risk factor for severe postoperative pain after breast cancer surgery. Medicine (Baltimore). 2019. https://doi.org/10.1097/MD.0000000000017708.
Ida M, Onodera H, Yamauchi M, Kawaguchi M. Preoperative sleep disruption and postoperative functional disability in lung surgery patients: a prospective observational study. J Anesth. 2019. https://doi.org/10.1007/s00540-019-02656-y.
Petrie K, Matzkin E. Can pharmacological and non-pharmacological sleep aids reduce post-operative pain and opioid usage? A review of the literature. Vol. 11, Orthopedic Reviews. Page Press Publications; 2019. p. 179–82. https://doi.org/10.4081/or.2019.8306.
Trauer JM, Qian MY, Doyle JS, Rajaratnam SMW, Cunnington D. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Vol. 163, Annals of Internal Medicine. American College of Physicians; 2015. p. 191–204. https://doi.org/10.7326/M14-2841.
Raats JW, van Eijsden WA, Crolla RMPH, Steyerberg EW, van der Laan L. Risk factors and outcomes for postoperative delirium after major surgery in elderly patients. Marengoni A, editor. PLoS One. 2015. https://doi.org/10.1371/journal.pone.0136071.
Austin CA, O’Gorman T, Stern E, Emmett D, Stürmer T, Carson S, et al. Association between postoperative delirium and long-term cognitive function after major nonemergent surgery. JAMA Surg. 2019. https://doi.org/10.1001/jamasurg.2018.5093.
Khadaroo RG, Warkentin LM, Wagg AS, Padwal RS, Clement F, Wang X, et al. Clinical effectiveness of the elder-friendly approaches to the surgical environment initiative in emergency general surgery. JAMA Surg. 2020. https://doi.org/10.1001/jamasurg.2019.6021.
Rengel KF, Mehdiratta N, Vanston SW, Archer KR, Jackson JC, Thompson JL, et al. A randomised pilot trial of combined cognitive and physical exercise prehabilitation to improve outcomes in surgical patients. Vol. 126, British Journal of Anaesthesia. Elsevier Ltd; 2021. https://doi.org/10.1016/j.bja.2020.11.004.
Joseph HK, Whitcomb J, Taylor W. Effect of anxiety on individuals and caregivers after coronary artery bypass grafting surgery: a review of the literature. Dimens Crit Care Nurs. 2015. https://doi.org/10.1097/DCC.0000000000000137.
Applebaum AJ, Breitbart W. Care for the cancer caregiver: a systematic review. Vol. 11, Palliative and Supportive Care. NIH Public Access; 2013. https://doi.org/10.1017/S1478951512000594.
Fu F, Zhao H, Tong F, Chi I. A systematic review of psychosocial interventions to cancer caregivers. Front Psychol. 2017. https://doi.org/10.3389/fpsyg.2017.00834.
Hoogeboom TJ, Oosting E, Vriezekolk JE, Veenhof C, Siemonsma PC, de Bie RA, et al. Therapeutic validity and effectiveness of preoperative exercise on functional recovery after joint replacement: a systematic review and meta-analysis. PLoS ONE. 2012. https://doi.org/10.1371/journal.pone.0038031.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors do not have any potential conflicts of interest to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Prehabilitation
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Brahmbhatt, P., Minnella, E.M., Randall, I.M. et al. Multimodal Prehabilitation: a Mini Review of Contemporary Research. Curr Anesthesiol Rep 12, 99–108 (2022). https://doi.org/10.1007/s40140-021-00490-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-021-00490-1