Abstract
Purpose of Review
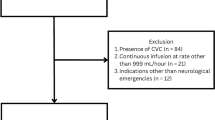
In this article, we review the use of hypertonic saline (HTS) for FDA-approved indications, namely treatment of hyponatremia and elevated intracranial pressure (ICP), as well as the routes of administration appropriate for infusion.
Recent Findings
Though society guidelines for treating hyponatremia have not recently changed, new data is emerging that supports the use of bolus-based HTS treatment regimens. HTS is at least as effective as mannitol for lowering elevated ICP from cerebral edema and is also now the preferred hyperosmolar treatment in patients with intracranial hemorrhage (ICH) and traumatic brain injury (TBI). Central venous catheter (CVC) has been recommended in the past for HTS infusions, but emerging data suggest infusion via peripheral intravenous catheters (IV) is likely safe and may be worth avoiding the time intensive and potentially harmful process of placing a CVC.
Summary
HTS infusion via peripheral IV appears to be safe, effective, and more time efficient than infusion via CVC in treating acute hyponatremia and increased ICP.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Mohan S, Gu S, Parikh A, Radhakrishnan J. Prevalence of hyponatremia and association with mortality: results from NHANES. Am J Med. 2013;126:1127-1137.e1.
Zhang X, Li X-Y. Prevalence of hyponatremia among older inpatients in a general hospital. Eur Geriatr Med. 2020;11:685–92.
Upadhyay A, Jaber BL, Madias NE. Incidence and prevalence of hyponatremia. Am J Med. 2006;119:S30–5.
•• Verbalis JG, Goldsmith SR, Greenberg A, Korzelius C, Schrier RW, Sterns RH, Thompson CJ. Diagnosis, evaluation, and treatment of hyponatremia: expert panel recommendations. Am J Med. 2013;126:S1-42. Most recent American guidelines on treating hyponatremia.
•• Spasovski G, Vanholder R, Allolio B, et al. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Eur J Endocrinol. 2014;170:G1-47. Most recent European guidelines on treating hyponatremia.
Buffington MA, Abreo K. Hyponatremia: a review. J Intensive Care Med. 2016;31:223–36.
Sterns RH, Riggs JE, Schochet SS. Osmotic demyelination syndrome following correction of hyponatremia. N Engl J Med. 1986;314:1535–42.
Lambeck J, Hieber M, DreBing A, Niesen WD. Central pontine myelinosis and osmotic demyelination syndrome. Dtsch Arxtebl Int. 2019;116:600–6.
Sterns RH, Nigwekar SU, Hix JK. The treatment of hyponatremia. Semin Nephrol. 2009;29:282–99.
Ayus JC, Caputo D, Bazerque F, Heguilen R, Gonzalez CD, Moritz ML. Treatment of hyponatremic encephalopathy with a 3% sodium chloride protocol: a case series. Am J Kidney Dis. 2015;65:435–42.
Garrahy A, Dineen R, Hannon AM, Cuesta M, Tormey W, Sherlock M, Thompson CJ. Continuous versus bolus infusion of hypertonic saline in the treatment of symptomatic hyponatremia caused by SIAD. J Clin Endocrinol Metab. 2019;104:3595–602.
Baek SH, Jo YH, Ahn S, Medina-Liabres K, Oh YK, Lee JB, Kim S. Risk of overcorrection in rapid intermittent bolus vs slow continuous infusion therapies of hypertonic saline for patients with symptomatic hyponatremia: The SALSA randomized clinical trial. JAMA Intern Med. 2021;181:81–92.
Sigal SH, Amin A, Chiodo JA, Sanyal A. Management strategies and outcomes for hyponatremia in cirrhosis in the hyponatremia registry. Can J Gatroenterol Hepatol. 2018;2018:1579508.
Hoorn EJ, Spasovski G. Recent developments in the management of acute and chronic hyponatremia. Curr Opin Nephrol Hypertens. 2019;28:424–32.
•• Cook AM, Morgan Jones G, Hawryluk GWJ, et al. Guidelines for the acute treatment of cerebral edema in neurocritical care patients. Neurocrit Care. 2020;32:647–66. Most recent Neurocritical Care Society Guidelines based on an in depth literature review.
Rangel-Castillo L, Gopinath S, Robertson CS. Management of intracranial hypertension. Neurol Clin. 2008;26:521–41.
Carter C, Human T. Efficacy, safety, and timing of 5% sodium chloride compared with 23.4% sodium chloride for osmotic therapy. Ann Pharmacother. 2017;51:625–9.
Busey K, Ferreira J, Aldridge P, Crandall M, Johnson D (2020) Comparison of weight-based dosing versus fixed dosing of 23.4% hypertonic saline for intracranial pressure reduction in patients with severe traumatic brain injury. J Emerg Trauma Shock 13:252
Maguigan KL, Dennis BM, Hamblin SE, Guillamondegui OD. Method of hypertonic saline administration: effects on osmolality in traumatic brain injury patients. J Clin Neurosci. 2017;39:147–50.
Vialet R, Albanèse J, Thomachot L, Antonini F, Bourgouin A, Alliez B, Martin C. Isovolume hypertonic solutes (sodium chloride or mannitol) in the treatment of refractory posttraumatic intracranial hypertension: 2 mL/kg 7.5% saline is more effective than 2 mL/kg 20% mannitol. Crit Care Med. 2003 Jun;31(6):1683–7. https://doi.org/10.1097/01.CCM.0000063268.91710.DF. PMID:12794404.
Kerwin AJ, Schinco MA, Tepas JJ 3rd, Renfro WH, Vitarbo EA, Muehlberger M. The use of 23.4% hypertonic saline for the management of elevated intracranial pressure in patients with severe traumatic brain injury: a pilot study. J Trauma. 2009 Aug;67(2):277–82. https://doi.org/10.1097/TA.0b013e3181acc726. PMID:19667879.
• Mekonnen M, Ong V, Florence TJ, Mozaffari K, Mahgerefteh N, Rana S, Duong C, Plurad DS, Yang I (2022) Hypertonic saline treatment in traumatic brain injury: a systematic review. World Neurosurgery 162:98–110. Most recent meta-analysis on HTS in TBI. This study confirms significant ICP reduction and suggests using lower concentrations for sustained reduction.
Pasarikovski CR, Alotaibi NM, Al-Mufti F, Macdonald RL. Hypertonic saline for increased intracranial pressure after aneurysmal subarachnoid hemorrhage: a systematic review. World Neurosurgery. 2017;105:1–6.
Hauer E-M, Stark D, Staykov D, Steigleder T, Schwab S, Bardutzky J. Early continuous hypertonic saline infusion in patients with severe cerebrovascular disease. Crit Care Med. 2011;39:1766–72.
Wagner I, Hauer E-M, Staykov D, Volbers B, Dörfler A, Schwab S, Bardutzky J. Effects of continuous hypertonic saline infusion on perihemorrhagic edema evolution. Stroke. 2011;42:1540–5.
Chen H, Song Z, Dennis JA. Hypertonic saline versus other intracranial pressure-lowering agents for people with acute traumatic brain injury. Cochrane Database Syst Rev. 2020. https://doi.org/10.1002/14651858.CD010904.pub3.
Rockswold GL, Solid CA, Paredes-Andrade E, Rockswold SB, Jancik JT, Quickel RR. Hypertonic saline and its effect on intracranial pressure, cerebral perfusion pressure, and brain tissue oxygen. Neurosurgery. 2009;65:1035–42.
F Munar AM Ferrer de NADAL M, Poca MA, Pedraza S, Sahuquillo J, Garnacho A, 2000 Cerebral hemodynamic effects of 7.2% hypertonic saline in patients with head injury and raised intracranial pressure J Neurotrauma 17:41–51
Boone M, Oren-Grinberg A, Robinson T, Chen C, Kasper E. Mannitol or hypertonic saline in the setting of traumatic brain injury: what have we learned? Surg Neurol Int. 2015;6:177.
Mangat HS, Chiu Y-L, Gerber LM, Alimi M, Ghajar J, Härtl R. Hypertonic saline reduces cumulative and daily intracranial pressure burdens after severe traumatic brain injury. JNS. 2015;122:202–10.
Kochanek PM, Adelson PD, Rosario BL, et al. Comparison of intracranial pressure measurements before and after hypertonic saline or mannitol treatment in children with severe traumatic brain injury. JAMA Netw Open. 2022;5: e220891.
Berger-Pelleiter E, Émond M, Lauzier F, Shields J-F, Turgeon AF. Hypertonic saline in severe traumatic brain injury: a systematic review and meta-analysis of randomized controlled trials. CJEM. 2016;18:112–20.
Shi J, Tan L, Ye J, Hu L. Hypertonic saline and mannitol in patients with traumatic brain injury: a systematic and meta-analysis. Medicine. 2020;99: e21655.
Strandvik GF. Hypertonic saline in critical care: a review of the literature and guidelines for use in hypotensive states and raised intracranial pressure. Anaesthesia. 2009;64:990–1003.
Mirtallo J, Canada T, Johnson D, Kumpf V, Petersen C, Sacks G, Seres D, Guenter P. Safe practices for parenteral nutrition. JPEN J Parenter Enteral Nutr. 2004;28:S39–70.
Parienti J-J, Mongardon N, Mégarbane B, et al. Intravascular complications of central venous catheterization by insertion site. N Engl J Med. 2015;373:1220–9.
Song Z, Chen S, Zhang Y, Shi X, Zhao N, Liao Z. Lidocaine coinfusion alleviates vascular pain induced by hypertonic saline infusion: a randomized, placebo-controlled trial. BMC Anesthesiol. 2021;21:109.
Brenkert TE, Estrada CM, McMorrow SP, Abramo TJ. Intravenous hypertonic saline use in the pediatric emergency department. Pediatr Emerg Care. 2013;29:71–3.
Dillon RC, Merchan C, Altshuler D, Papadopoulos J. Incidence of adverse events during peripheral administration of sodium chloride 3%. J Intensive Care Med. 2018;33:48–53.
Faiver L, Hensler D, Rush SC, Kashlan O, Williamson CA, Rajajee V. Safety and efficacy of 23.4% sodium chloride administered via peripheral venous access for the treatment of cerebral herniation and intracranial pressure elevation. Neurocrit Care. 2021;35:845–52.
Jannotta GE, Gulek BG, Dempsey JS, Blissitt PA, Sullivan HC, Tran K, Joffe A, Lele AV. Administration of 3% sodium chloride through peripheral intravenous access: development and implementation of a protocol for clinical practice. Worldviews on Evidence-Based Nursing. 2021;18:147–53.
Jones GM, Bode L, Riha H, Erdman MJ. Safety of continuous peripheral infusion of 3% sodium chloride solution in neurocritical care patients. Am J Crit Care. 2017;26:37–42.
Mesghali E, Fitter S, Bahjri K, Moussavi K. Safety of peripheral line administration of 3% hypertonic saline and mannitol in the emergency department. J Emerg Med. 2019;56:431–6.
Perez CA, Figueroa SA. Complication rates of 3% hypertonic saline infusion through peripheral intravenous access. J Neurosci Nurs. 2017;49:191–5.
Pohl CE, Harvey H, Foley J, Lee E, Xu R, O’Brien NF, Coufal NG. Peripheral IV administration of hypertonic saline: single-center retrospective picu study*. Pediatr Crit Care Med. 2022;23:277–85.
Meng L, Nguyen CM, Patel S, Mlynash M, Caulfield AF. Association between continuous peripheral i.v. infusion of 3% sodium chloride injection and phlebitis in adults. Am J Health Syst Pharm. 2018;75:284–91.
Lawson T, Hussein O, Nasir M, Hinduja A, Torbey MT. Intraosseous administration of hypertonic saline in acute brain-injured patients: a prospective case series and literature review. Neurologist. 2019;24:176–9.
Farrokh S, Cho S-M, Lefebvre AT, Zink EK, Schiavi A, Puttgen HA. Use of intraosseous hypertonic saline in critically ill patients. J Vasc Access. 2019;20:427–32.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dangers, J., Enders, M. & Helberg, T. Hypertonic Saline in the Critically Ill: A Review of Indications, Routes, and Dosing. Curr Emerg Hosp Med Rep 11, 95–102 (2023). https://doi.org/10.1007/s40138-023-00267-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40138-023-00267-2